Clinical evidence and potential mechanisms of Chinese medicines for the treatment of diabetic retinopathy
Jian Huo, Ke-Yu Zhu, Qian Yang, Wen Liu, Jun-Guo Duan*
1Academy of Ophthalmology, Chengdu University of Traditional Chinese Medicine, Chengdu, Sichuan, China.2Chengdu University of Traditional Chinese Medicine Affiliated Ineye Hospital, Chengdu, Sichuan, China.
Background
Diabetic retinopathy (DR) is one of the main causes of visual impairment and blindness on a global scale [1].Major complications of DR include intraocular neovascularization, intraretinal edema, hemorrhage,exudates, and microaneurysms. DR is the result of several hyperglycemia-induced pathological changes, such as increased oxidative stress-induced apoptosis of retinal endothelial and neuronal cells, angiogenesis, and inflammatory responses [2]. At present, strict control of blood sugar, blood pressure, and blood lipid levels within the normal range is still vital to delay the development of DR. Treatments for DR include anti-vascular endothelial growth factor (VEGF) agents, steroids, laser photocoagulation, and vitreous surgery. However, these therapeutic methods cannot reverse the existing retinal damage. Moreover, some adverse events are associated with these treatments [3].
Traditional Chinese medicine (TCM) is an alternative therapy that has been used for thousands of years in China, which regards DR as Yin deficiency of the liver and kidney, Yin deficiency with dryness-heat, Yin deficiency with fluid inadequacy, and Yin deficiency with blood stasis [4]. “Qi is the essence of the body” means that blood flow and body fluid transfusion depend on Qi promotion. Further, Qi can control blood circulation in the vessels. Qi-Yin insufficiency is the root cause of DR,while Qi stagnation and blood stasis are the symptoms of DR. Qi-Yin deficiency and blood stasis are the key pathogeneses of DR [5, 6]. DR develops because of blood stasis, which causes hemorrhage, microaneurysms, and angiogenesis [7]. Several Chinese herbs, including Huangqi (Radix Astragali seu Hedysari), Dihuang (Radix Rehmanniae), and Danshen (Radix Salviae Miltiorrhizae),have the effect of tonifying Qi, nourishing Yin, and removing blood stasis. Some well-established Chinese herbal formulae and Chinese patent drugs have also been shown to effectively treat DR in basic and clinical studies.According to the Guidelines for Diagnosis and Treatment of DR in Chinese Medicine [7], there are some formulaes for DR that are based on syndrome differentiation and are listed in Table 1. This review focuses on both clinical and basic researches to summarize the application of Chinese medicines and their mechanisms of action in the treatment of DR (Table 2).
Method of literature search
This review was conducted with a comprehensive Pubmed and China National Knowledge Infrastructure(www.cnki.net) search of references related to the following key words: diabetic retinopathy, herbal,medicine, traditional, Heyingqingre, Buyanghuanwu Decoction, Zhenwu Decoction, Giming Granule, Fufang Xueshuantong, Fufang Danshen Dripping Pill, Yinxing,Qishenyiqi Dropping Pill, Liuweidihuang, and Naoxintong. The search included non-English language articles. All articles published from 2000 to March 2017 were searched.
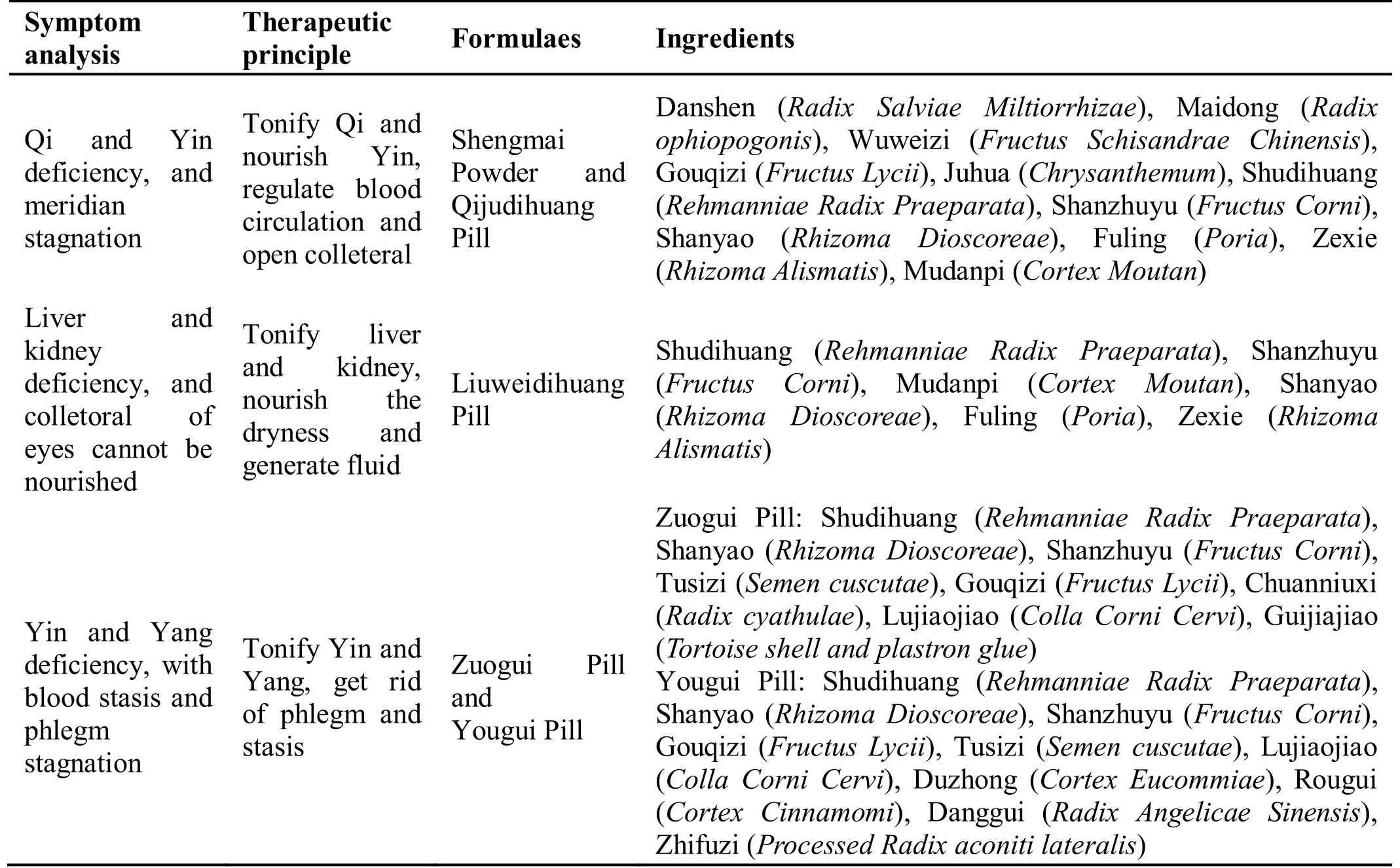
Table 1 Formulaes for diabetic retinopathy based on syndrome differentiation
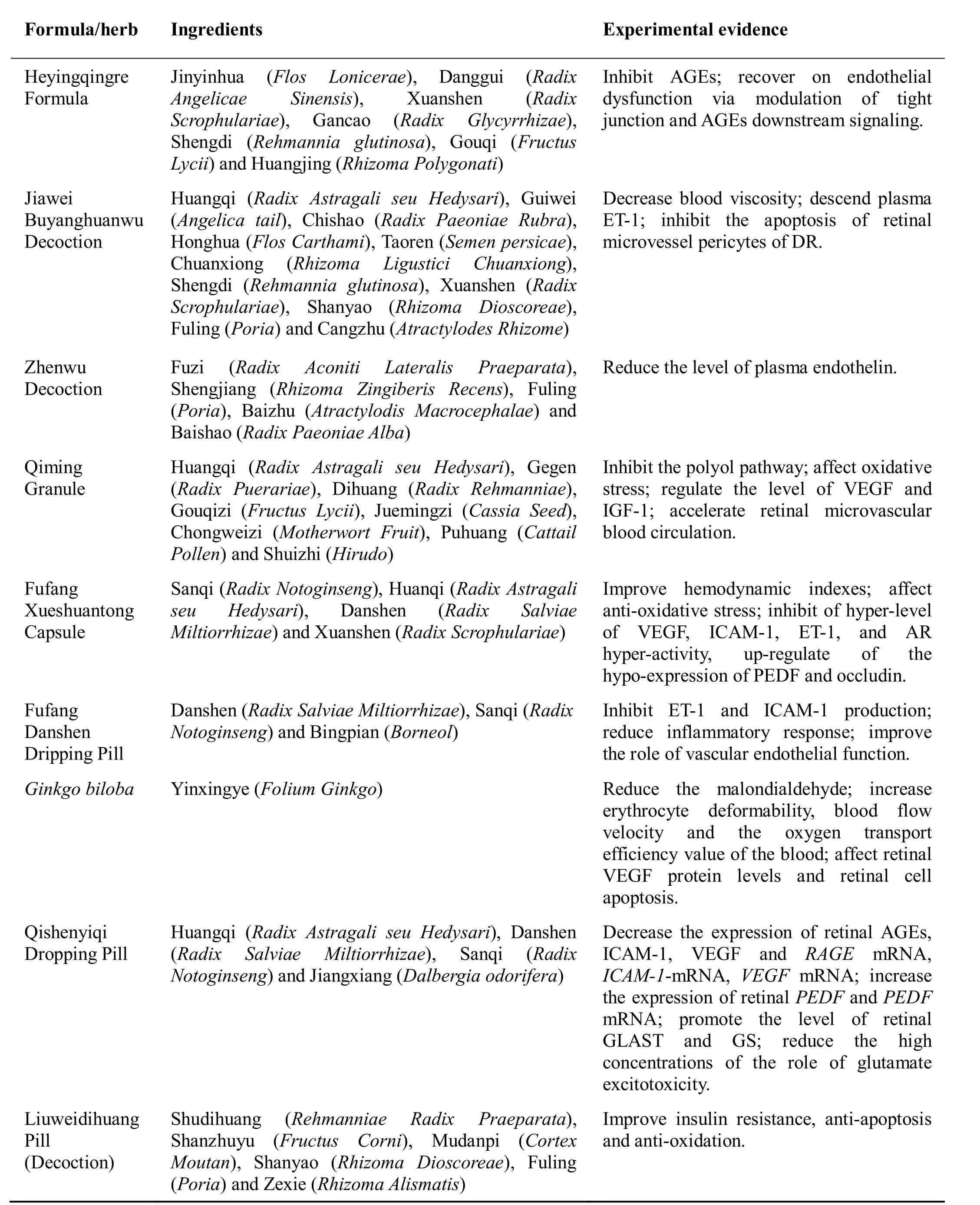
Table 2 Experimental evidence of formulaes/herbs for diabetic retinopathy
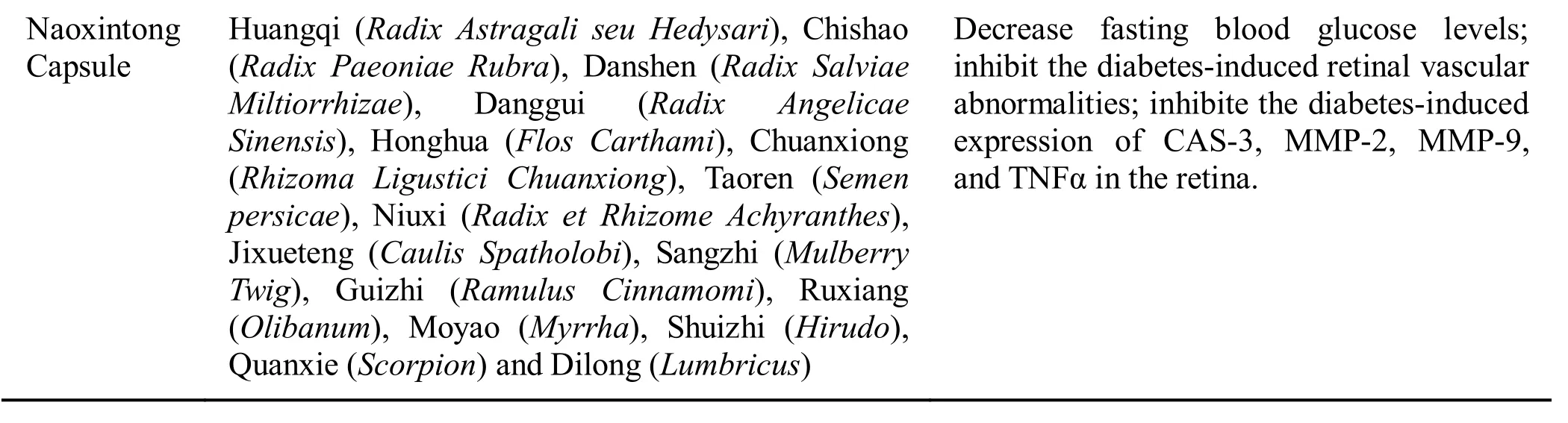
Table 2: Continued.
Chinese herbal formulaes
Heyingqingre Formula
Heyingqingre Formula (HF) is a formula modified from Simiaoyongan Decoction by Zou Jusheng, a prominent TCM doctor. Simiaoyongan Decoction emerged in the Qing Dynasty of China (1644 B.C.-1912B.C.) and has also been shown more recently to be beneficial for vascular diseases. It can clear heat and activate blood flow owing to the presence of Jinyinhua (Flos Lonicerae),Danggui (Radix Angelicae Sinensis), Xuanshen (Radix Scrophulariae), and Gancao (Radix Glycyrrhizae). HF has been used in a local hospital for decades as a complementary treatment method for DR with retinal vascular dysfunction. HF was modified for effective DR treatment by adding some herbs as nourishing Yin, such as Shengdi (Rehmannia glutinosa), Gouqi (Fructus Lycii),and Huangjing (Rhizoma Polygonati). Furthermore,chlorogenic acid, ferulic acid, and arctin have been identified as the major components of HF [8].
Clinical reports revealed that HF could ameliorate visual defects, microaneurysms, hemorrhages, and macular edema. In a clinical report [9] of 61 patients(Heyingqingre group: 31 cases, 52 eyes; Calcium dobesilate group: 30 cases, 50 eyes) with DR in the non-proliferative stage, use of HF for 3 months was much more effective compared with the control group (calcium dobesilate) with respect to visual acuity, fundus examination, and TCM syndrome, indicating that HF has definite effects on DR in the non-proliferative stage.Compared with the results of laser treatment alone, the combination of laser and HF decreased fundus hemorrhages, exudation, and macular edema, which indicated that HF is a potential complementary treatment for DR [10]. Wang et al. [8] investigated the anti-DR action of HF and its underlying mechanism experimentally in a rodent model of DR. The data indicated that HF suppresses retinal vasculature degeneration and blood-retina-barrier permeability damage without significant inhibition of hyperglycemia in vitro and in vivo. HF also reduced the formation of advanced glycation end products (AGEs) and AGE-induced migration as well as the permeability of retinal vascular endothelial cells. The level of the tight junction proteins, Zo-1 and Claudin-1 was increased,while activation of the AGE receptor and downstream signaling to Akt was suppressed upon HF treatment.Therefore, HF exhibits protective effects against DR,which might be associated with inhibition of AGEs and recovery of endothelial dysfunction via modulation of tight junctions and AGE downstream signaling.
Jiawei Buyanghuanwu Decoction (JBHD)
Buyanghuanwu Decoction (BHD) is a classic traditional Chinese herbal prescription for stroke, which was first recorded in the Yilingaicuo written by Wang Qingren in 1830 B.C. during the late Qing Dynasty of China [11].BHD is composed of seven types of Chinese medicine:Huangqi (Radix Astragali seu Hedysari), Guiwei(Angelica root tail), Chishao (Radix Paeoniae Rubra),Dilong (Lumbricus), Honghua (Flos Carthami), Taoren(Semen persicae) and Chuanxiong (Rhizoma Ligustici Chuanxiong), with functions of tonifying Qi, invigorating blood circulation, and dredging collaterals. Based on the TCM theory of concerted application, the main characteristics of BHD arise from the use of its principal drug, Huangqi (Radix Astragali seu Hedysari), in larger doses, invigorating Qi to activate blood circulation. In modern times, BHD is still widely used throughout China and elsewhere in the world for the treatment of ischemic stroke [12]. In addition, it has been confirmed that BHD has curative effects on cardiovascular diseases,cerebrovascular diseases, and other disorders with Qi deficiency and blood stasis patterns [13, 14].
Based on the TCM theory of treating different diseases with the same method, BHD is a classical representative prescription of the Qi-tonifying and stasis-eliminating method [15]. BHD has also been used to treat diabetes and its complications [16]. Based on BHD, JBHD is modified for effective DR treatment by removing Dilong(Lumbricus) and adding Shengdi (Rehmannia glutinosa)and Xuanshen (Radix Scrophulariae), whose function to nourish Yin, as well as adding Shanyao (Rhizoma Dioscoreae), Fuling (Poria), and Cangzhu (Atractylodes Rhizome), whose function to regulate “Qi-flowing” for spleen strengthening. According to TCM, JBHD is suitable for the treatment of non-proliferative DR (NPDR)with the syndrome of Qi and Yin deficiency and blood stasis [17].
JBHD can effectively improve a hypercoagulable state,retinal microcirculation, and retinal function; it can also retrogress macular edema, decrease blood viscosity,reduce plasma endothelin-1 (ET-1), and inhibit apoptosis of retinal microvascular pericytes in DR. In a preliminary clinical study [18], Tang and his colleagues concluded that 8-week oral administration of JBHD could improve hemorheologic indexes in 60 patients with simple DR. A favorable effect of JBHD was observed in the treatment of DR in that it protected visual acuity and improved macular edema retrogression by analyzing fluorescence fundus angiography after 3-12 months of medication in a clinical trial (58 cases, 116 eyes of DR patients). The study showed that the combination of retinal laser photocoagulation (532 nm double frequency laser) and JBHD is an effective method to treat DR, which could protect visual acuity and improve macular edema retrogression [19]. A similar finding was observed by Jin and his colleagues indicating that JBHD and retinal laser photocoagulation could improve retinal microcirculation and retinal function partially when treating NPDR, and that JBHD could reduce the ET-1 in NPDR [20].Furthermore, in another report by Dong et al., apoptosis of retinal microvascular pericytes was observed in rats with diabetes mellitus (DM) on the twelfth week, and JBHD could inhibit this apoptosis [17]. However,multicenter, randomized, parallel controlled clinical trials are required to determine the effect of JBHD on DR.
Zhenwu Decoction
Zhenwu Decoction was first introduced by Zhang Zhongjing in the third century. His book, Shanghanlun has been widely used for the treatment of internal,external, and gynecological diseases, and for many other clinical treatments [21]. There are five components in Zhenwu Decoction: Fuzi (Radix Aconiti Lateralis Praeparata), Shengjiang (Rhizoma Zingiberis Recens),Fuling (Poria), Baizhu (Atractylodis macrocephala), and Baishao (Radix Paeoniae Alba). In the prescription, Fuzi(Radix Aconiti Lateralis Praeparata) dispels cold;Shengjiang (Rhizoma Zingiberis Recens) helps to dispel cold and expel the cold fluid; both Fuling (Poria) and Baizhu (Atractylodis macrocephala) invigorate the spleen for diuresis; and Baishao (Radix Paeoniae Alba) helps nourish the blood [22].
Zhenwu Decoction exhibited a beneficial effect in patients with DR. In a preliminary, double-blind clinical study of 80 elderly patients with type 2 DR, Zhenwu Decoction combined with western medicine for treating DR, reduced the level of plasma ET-1 [23]. A similar report by Zhu KJ, et al. also indicated that Zhenwu Decoction had a significant therapeutic effect on DR [24].
Chinese patent drugs
Modern developed drugs
Qiming Granule.The Chinese compound medicine,Qiming (QM) Granule, is the first drug approved by China FDA for the treatmen of DR. It was studied by Professor Liao Pinzheng and Professor Duan Junguo of Chengdu University of TCM. The functions of QM Granule is to replenish Qi, produce Yin, nourish the liver and kidney, and activate eye channels to improve eyesight[25]. QM Granule is suitable for the treatment of NPDR.In addition , based on syndrome differentiation in TCM,QM Granule is suitable for deficiency of both Qi and Yin[26].
QM Granule consists of eight traditional plants, namely Huangqi (Radix Astragali seu Hedysari), Gegen (Radix Puerariae), Dihuang (Radix Rehmanniae), Gouqi(Fructus Lycii), Juemingzi (Cassia Seed), Chongweizi(Motherwort Fruit), Puhuang (Cattail Pollen), and Shuizhi (Hirudo) [27]. Huangqi (Radix Astragali seu Hedysari) contains saponins, flavonoids, amino acids,proteins, vitamins, glycans, organic acids,polysaccharides, and other substances. It is used to treat Qi deficiency and blood stagnation syndrome. Gegen(Radix Puerariae) helps produce saliva, slake thirst, and invigorating spleen Yang. Puerarin is the main active compound extracted from Gegen (Radix Puerariae).Dihuang (Radix Rehmanniae) has the effect of heat-clearing and blood-cooling, nourishing Yin, and generating body fluid [28]. The main chemical constituents of Dihuang (Radix Rehmanniae) are polysaccharides [29], iridoid glycosides [30],phenylethanoid glycosides [31], nucleosides [32], and other ingredients.
In a 3-month, randomized, controlled, double-blind,multicenter clinical trial, with 212 eyes from 212 patients with NPDR (QM Granule group, 107 patients;Doxium®-controlled group, 105 patients), QM Granule was more effective than Doxium®with respect to the excellence rate and total effective rate of the TCM. The adverse effect rate in the QM Granule group was 0.935%,while that of the Doxium®-controlled group was 7.619%,indicating that the QM Granule was safe. Therefore, the QM Granule may be superior to Doxium®Tablets in treating NPDR [26]. A favorable effect of QM Granule in the treatment of DR that was observed by analyzing fluorescence fundus angiography after 3 months of medication in a multicenter, randomized, parallel controlled clinical trial (360 DR patients) was improved retinal blood circulation, indicating that QM Granule might alleviate retinal hypoxia and ischemia by increasing retinal blood flow and improving blood circulation [33]. QM Granule combined with calcium dobesilate therapy could improve choroidal circulation,inhibit angiogenesis mediated by a variety of cytokines in the retina, and alter branched chain amino acid metabolism [34]. Feng HJ, et al. reported a clinical study on NPDR patients treated with QM Granule combined with Xueshuantong Capsule, and planned to evaluate the efficiency and safety of QM Granule in patients with DR.The data obtained from the research showed that the effect in the observation group (QM Granule combined with Xueshuangtong Capsule) was significantly better than the effect in the control group (Xueshuantong Capsule); the patients in both groups had no drug-related complications, and the mechanism may have involved lower VEGF and insulin-like growth factor 1 (IGF-1)levels [35]. Furthermore, panretinal photocoagulation combined with medication (QM Granule and/or calcium dobesilate) therapy was not only effective in promoting regression of neovascularization, but it also improved DR-induced vision loss in patients receiving panretinal photocoagulation [36]. These studies provide evidence of the clinical utility of QM Granule for the treatment of DR.
QM Granule can delay the progression of DR. The therapeutic effect and mechanism of QM Granule may occur through inhibition of the polyol pathway(increasing synthesis of inositol, thus reducing histiocytic damage) [37], affecting oxidative stress (reducing the content of malondialdehyde, increasing the activity of superoxide dismutase and glutathione peroxidase) [38],regulating the expression of VEGF [39] and IGF-1 [39,40], and accelerating retinal microvascular blood circulation [41].
Fufang Xueshuantong Capsule.Fufang Xueshuantong(FXT) Capsule is a herbal formula licensed for clinical use in China [42], which is composed of Sanqi (Radix Notoginseng), Huangqi (Radix Astragali seu Hedysari),Danshen (Radix Salviae Miltiorrhizae), and Xuanshen(Radix Scrophulariae) [43], with functions of dilating the vessels, increasing blood flow, improving blood circulation, and improving microcirculation [44]. The saponins of Sanqi (Radix Notoginseng), harpagoside,cryptotanshinone, tanshinone I, and astragaloside A, are the core constituents of FXT Capsule [45].
FXT Capsule has beneficial effects on DR [46], which could improve retinal blood perfusion for NPDR after photocoagulation [47]. A clinical study reported that FXT Capsule could improve hemodynamic indexes (including peak systolic velocity, end diastolic velocity, mean velocity, pulsatility index, and resistance index in the central retinal artery, as well as maximum velocity and minimum velocity in the central retinal vein) in the retinas of NPDR patients and improve their vision [48].In another clinic study, FXT Capsule administered to DR patients for 5 months induced a decrease in the levels of high-sensitivity C-reactive protein, VEGF, and IGF-1.From these data, it was concluded that FXT Capsule combined with calcium dobesilate could reduce the recurrence rate and delay the proliferation of blood vessels more than oral calcium dobesilate alone [49].
FXT Capsule could play a role in the treatment of DR by decreasing pericyte loss and reducing acellular capillaries [45]. Its mechanism might involve reducing oxidative stress [50]; inhibition of the hyperexpression of VEGF [45, 50, 51], intercellular adhesion molecule-1(ICAM-1), and ET-1; reversal of the hyperactivation of aldose reductase; or upregulation of the hypoexpression of pigment epithelium-derived factor (PEDF) and occludin [45, 51]. Animal studies showed that the antioxidative and antihypoxic effects of FXT Capsule on diabetic retinas might be mediated by ameliorating the state of ischemia and hypoxia, downregulating the expression of hypoxia-inducible factor 1 alpha, enhancing the activity of superoxide dismutase, and upregulating the expression of CuZn superoxide dismutase [52]. In addition, FXT Capsule could attenuate whole blood viscosity, plasma viscosity, and erythrocyte aggregation.However, FXT Capsule had no effect on body weight gain and blood glucose level [51].
Fufang Danshen Dripping Pill.Fufang Danshen Dripping Pill, also known as compound Danshen Dripping Pill (CDDP), is a well-established formulation as the first new drug through the American FDA II clinical trials, which is used to treat cardiovascular diseases [53]. CDDP is a Chinese formula that consists of Danshen (Radix Salviae Miltiorrhizae), Sanqi (Radix Notoginseng), and Bingpian (Borneol). It has the effect of promoting blood circulation to remove blood stasis,regulating Qi, and relieving pain. Danshen (Radix Salviae Miltiorrhizae) is a common TCM often used to treat many medical conditions, especially blood stasis. CDDP is still appropriate for treatment of DR with blood stasis syndrome [7]. According to Chinese Pharmacopoeia records, CDDP, through a water extraction process,contains water-soluble tanshinol (Danshensu), salvianolic acid B, protocatechuic aldehyde, notoginseng saponins,and other major components [54].
CDDP could improve visual acuity, control microhemorrhage and microaneurysm of fundus, and affect visual functional recovery in DR [55]. Lian and colleagues reported that CDDP had definite efficacy and safety for treating NPDR. In their controlled clinical trial involving 223 patients with NPDR, the ratio of“Excellent” and “Effective” in the high-dose (30 pills three times per day) and mid-dose (20 pills three times per day) CDDP groups was significantly greater than that in the placebo group after a 24-week treatment, as assessed by fluorescence fundus angiography and fundoscopic examination. No adverse events with clinical significance occurred [56]. In another randomized,double-dummy, double-blind study, after 3-month treatment, there was no statistical difference in each index(including the best corrected visual acuity, visual field,hemorrhage area of the fundus, microaneurysm number,fluorescent leakage area, and capillary nonperfusion area)between the treated group (CDDP) and the control group(calcium dobesilate). The results showed that CDDP showed a similar improvement of NPDR and safety profile as calcium dobesilate. CDDP might be considered the auxiliary drug for DR [57].
Studies have shown that CDDP, through anti-inflammatory and vascular endothelium-protective effects, plays a therapeutic role in DR [58]. DR is a chronic, low-grade inflammatory disease [59] and impaired endothelial function is a common denominator of pathogenesis in DR [60]. Yang and colleagues found that, after CDDP treatment of early DR patients, the endothelium-dependent flow-mediated dilatation could be greatly improved, and ET-1 and ICAM-1 production could be inhibited, thereby reducing blood vessel contraction and spasm to improve vascular endothelial function [58]. This indicated that CDDP could effectively reduce early DR in patients by improving inflammatory response and vascular endothelial function [60].
Ginkgo biloba.Yinxing (Ginkgo biloba, GB) is an ancient medicinal tree species that has been in existence for millennia without undergoing changes due to its resistance to environmental stresses [61]; it has been used in TCM for approximately 5000 years [62]. As early as the Shennongbencaojing, GB has been recorded to have medicinal properties, such as moistening the lung and acting as an anti-asthmatic and antitussive agent [63]. The extracts from the leaves of GB have been used as a standardized preparation Egb 761 [64]. Yinxingye(Folium Ginkgo, GBL) has the function of curing diseases of the lung and asthma, promoting blood circulation, and relieving pain. The chemical constituents responsible for the bioactivities of GBL have been identified as biflavones, terpene trilactones (ginkgolides A, B, C, J, P and Q, and bilobalides), flavonol glycosides(quercetin, catechin), and proanthocyanidins [65, 66].Ginkgo biloba extract (GBE) has been found to be useful in the treatment of cerebral infarction, Alzheimer’s disease, hypertension, coronary heart disease, DM and its complications, chronic glomerulonephritis, and especially chronic diseases [67]. GBE has pharmacological functions, including antioxidant, free radical-scavenging,and anti-platelet activating factor activities, as well as regulation of vascular activity, augmentation of blood flow, and neuroprotection [62, 63]. Early studies indicated a potential role in age-related macular degeneration [68] and some types of glaucoma [69].
GBE has also shown a beneficial effect in DR. In a preliminary clinical study, Huang and colleagues concluded that 3 months of oral administration of Egb 761 for type 2 diabetic patients with retinopathy could reduce fibrinogen levels, plasma viscosity, and malondialdehyde content of erythrocyte membranes (i.e.,reduce lipid peroxidation stress), as well as increase erythrocyte deformability. This improves blood viscosity and viscoelasticity, further increasing blood flow velocity and the oxygen transport efficiency value of the blood.These factors could all contribute to improving or lowering peripheral circulation disorders among diabetic patients. The data indicated that providing Egb 761 to type 2 DM patients can result in a meaningful impact on their blood circulation and reduction in retinopathy occurrence [70]. Zhu and associates explored the clinical efficacy of GBE with 80 patients (150 eyes) with mild or moderate NPDR. After 6 months of treatment, the total effective rate in the treatment group (enteric-coated aspirin tablets plus GBE, 75.6%) was significantly higher than that in the control group (enteric-coated aspirin tablets, 58.7%); this showed that GBE could reduce retinal hemorrhage and exudation, improve visual acuity and visual field, and reduce retinal vascular endothelial cell damage [71]. Therefore, we believe that GBE has a definite effect on the prevention and treatment of DR.
A previous study demonstrated that GBE affects retinal VEGF protein levels and retinal cell apoptosis. The expression of diabetic retinal VEGF could be reduced and retinal ganglion cell apoptosis could be attenuated by GBE in non-obese diabetic mice with diabetes [72].However, the molecular mechanisms underlying these actions should be further elucidated, and more clinical trials are required to explore the effect of GBL on DR.
Qishenyiqi Dropping Pill. Qishenyiqi (QSYQ) Dropping Pill is a Chinese medicine prescription approved by the State Food and Drug Administration of China [73]. The QSYQ Dropping Pill is composed of Huangqi (Radix Astragali seu Hedysari), Danshen (Radix Salviae Miltiorrhizae), Sanqi (Radix Notoginseng), and Jiangxiang (Dalbergia odorifera), and has the effect of tonifying Qi, promoting blood circulation, and relieving pain. Hence, it has been widely used to treat cardiovascular diseases with Qi deficiency and blood stasis syndrome [74, 75], including myocardial infarction,angina, myocarditis, myocardial fibrosis, and heart failure[76-78]. Twelve compounds are the main components of QSYQ, including astragaloside IV, calycosin, and formononetin from Huangqi (Radix Astragali seu Hedysari); Danshensu, protocatechuic aldehyde, and rosmarinic acid from Danshen (Radix Salviae Miltiorrhizae); ginsenoside Rg1, ginsenoside Rb1, and notoginsenoside R1 from Sanqi (Radix Notoginseng); and trans-nerolidol, (3S,6S,7R)-3,7,11-trimethyl-3,6-epoxy-1,10-dodecadien-7-ol, and (3S, 6R,7R)-3,7,11-trimethyl-3,6-epoxy-1,10-dodecadien-7-ol from Jiangxiang (Dalbergia odorifera). These compounds are absorbed into the blood and distributed into the tissues after oral administration [79].
Recently, it was reported that QSYQ Dropping Pill could delay the progression of DR in animal studies. The mechanism of QSYQ may occur by decreasing the expression of retinal AGEs, ICAM-1, and VEGF;reducing the mRNA expression of the receptor for AGEs,ICAM-1, and VEGF; increasing the expression of retinal PEDF and PEDF mRNA; promoting the expression of retinal glutamate-aspartate transporters and glutamine synthetase; and reducing the effect of high concentrations of glutamate on excitotoxicity [80-83]. All of these studies also provide an experimental basis for the clinical application of Chinese patent medicine to prevent and cure DR.
Ancient processed drugs
Liuweidihuang Pill (Decoction).Liuweidihuang Pill(LDP) was initially created by Qian Yi in 1119 B.C., who was the famous doctor of TCM in the Song Dynasty of China. It was originally used to treat dysplasia in children[84]. LDP was derived from the Jinguiyaolue written by Zhang Zhongjing. The herbal formula of LDP consists of Shudihuang (Rehmanniae Radix Praeparata), Shanzhuyu(Fructus Corni), Mudanpi (Cortex Moutan), Shanyao(Rhizoma Dioscoreae), Fuling (Poria), and Zexie(Rhizoma Alismatis), with the effects of enriching Yin and tonifying the kidney. Three of the six ingredients in the formula are nutrients, while the other three facilitate drainage. Because of its unique composition and affirmed therapeutic effect, the main indications of the efficacy of this formula have been expanded. It was widely applied in the treatment of different diseases in internal medicine,surgery, gynecology, pediatrics, and other diseases, for syndromes differentiated as kidney Yin deficiency, liver and kidney Yin deficiency, and hyperactivity of deficient fire. Modern pharmacological research indicated that it has obvious effects of strengthening immunization,anti-aging, anti-fatigue, anti-low temperature, hypoxia tolerance, decreasing blood fat, blood pressure and blood sugar reduction, and improving renal function, among other activities. LDP has a long history in treating diabetes. Pharmacology research indicated that it is effective in improving insulin resistance, inhibiting apoptosis, and reducing oxidative stress [85]. Adding LDP to Western medicine could improve treatment outcomes of diabetes [86].
In a randomized, double-blind and placebo-controlled clinical trial of 140 outpatients with type 2 diabetes, after 36 months of treatment, the urinary creatinine ratio(Umalb/cr), diabetic nephropathy prevalence, and DR prevalence in the treatment group (LDP and Ginkgo leaf Tablet (GLT) were all significantly lower than those of the control group (Placebo) [87]. An analogous clinical trial was reported by An XF, et al [88]; it showed that the incidence rate of DR was significantly lower in the treatment group (LDP and GLT) than in the control group(Placebo). These results indicate that LDP and GLT are beneficial to DR and will prevent and treat the development of DR.
Naoxintong Capsule.Naoxintong (NXT) is an empirical formula based on the principle of TCM by Professor Zhao Buchang, based on Wang Qingren’s “Buyang-huanwu Soup” from the Qing Dynasty of China (1644 B.C.-1912B.C.), with the functions of replenishing Qi and promoting blood circulation to remove blood stasis [89].NXT has been approved by the China Food and Drug Administration (Z20025001) [90] and has been recognized as a treatment for coronary heart disease, Qi deficiency, blood stasis syndrome, and cerebrovascular diseases in clinical trials [91]; it has good clinical effect and is cost-effective [92]. NXT contains sixteen types of TCM, including Huangqi (Radix Astragali seu Hedysari),Chishao (Radix Paeoniae Rubra), Danshen (Radix Salviae Miltiorrhizae), Danggui (Radix Angelicae Sinensis), Honghua (Flos Carthami), Chuanxiong(Ligusticum chuanxiong Hort), Taoren (Semen persicae),Niuxi (Radix et Rhizome Achyranthes), Jixueteng (Caulis Spatholobi), Sangzhi (Mulberry Twig), Guizhi (Ramulus Cinnamomi), Ruxiang (Olibanum), Moyao (Myrrh), and animal medicines, including Shuizhi (Hirudo), Quanxie(Scorpion), and Dilong (Lumbricus). Modern pharmacological studies have demonstrated that [93],Huangqi (Radix Astragali seu Hedysari) has hypolipidemic and antioxidant effects; Quanxie (Scorpion)can reduce the content and activity of thrombin plasminogen activator and has antithrombotic effects;Dilong (Lumbricus) and Quanxie (Scorpion) contain a large number of hydrolytic proteases with thrombolytic factors, and can reduce cholesterol, atherosclerotic plaques, and dissolve thrombi; Danshen (Radix Salviae Miltiorrhizae) can reduce the blood content of low-density lipoprotein and triacylglycerol; Danggui(Radix Angelicae Sinensis) and Chuanxiong (Ligusticum chuanxiong Hort) have antithrombotic and hypolipidemic effects; and Honghua (Flos Carthami) and Chuanxiong(Ligusticum chuanxiong Hort) have inhibitory effects on platelet aggregation and disaggregation.
The formation of DR is associated with pathological progression of the microvascular system. Therefore, we surmise that NXT can reduce the development of DR. A recent study by Liu MY, et al. evaluated the effect of NXT in a mouse model of DR [94]. In this study, NXT decreased fasting blood glucose levels, inhibited diabetes-induced retinal vascular abnormalities, and inhibited diabetes-induced expression of caspase-3,matrix metalloproteinase-2, matrix metalloproteinase-9,and tumor necrosis factor α in the retina. This research indicated that NXT inhibits the development of DR in mice, which implies an important and potential application of NXT for treatment of diabetic retinopathy in the clinic.
Conclusion
Chinese medicines are being currently explored to find safer alternative treatments for DR. Despite heterogeneity in clinical trials, they have shown positive results in alleviating the hyperglycemia-induced pathological conditions. Some objective limitations should be considered based on existing research. A well-designed randomized controlled trial and a better understanding of the mechanisms of Chinese herbs should be elaborated in future studies. Chinese medicines are a complex system,even with guidance from TCM. The compounds contained in one herb, even in an extract of one herb, are very complicated. Therefore, the side effects of herbs and their drug interactions should be explored and taken into account. Chinese medicine needs to continue development, based on the theory of TCM, to show the characteristics of TCM. Hopefully, Chinese medicine will have a broader usage to treat or prevent DR as an alternative or as a combination therapy.
1. Chistiakov DA. Diabetic retinopathy: pathogenic mechanisms and current treatments. Diabetes Metab Syndr 2011, 5: 165-172.
2. Behl T, Kotwani A. Chinese herbal drugs for the treatment of diabetic retinopathy. J Pharm Pharmacol 2017, 69: 223-235.
3. Dedania VS, Bakri SJ. Novel pharmacotherapies in diabetic retinopathy. Middle East Afr J Ophthalmol 2015, 22: 164-173.
4. Li GZ, Liu Y. Traditional Chinese medicine treatment of diabetic retinopathy. J Pract Tradit Chin Intern Med 2014, 28: 178-179.
5. Zheng XY. Guiding principles of clinical research on new drug of traditional Chinese medicine. Beijing:China Medical Science Press 2002.
6. Wang LL, Wang N, Feng YB, et al. Clinical and basic research advances of traditional Chinese medical on diabetic retinopathy. J Tradit Chin Ophthalmol 2014,24: 227-232.
7. Duan JG, Jin M, Jie CH, et al. Standard of TCM diagnosis and treatment of diabetic retinal lesions.World J Integr Tradit West Med 2011, 6: 632-637.
8. Wang L, Wang N, Tan HY, et al. Protective effect of a Chinese medicine formula He-Ying-Qing-Re Formula on diabetic retinopathy. J Ethnopharmacol 2015, 169: 295-304.
9. Ye CF, Zhang YJ. Clinical observation of harmonlzing Ying and clearing heat therapy on diabetic retinopathy in non-proliferative stage. Hebei J Tradit Chin Med 2012, 34: 1204-1274.
10. Zhang YJ, Su J, Li H. Combination of ‘Heying Prescription’ and laser therapy for diabetic retiopathy.Shanghai J Tradit Chin Med 2012, 46: 50-52.
11. Wang QR (Qing Dynasty). Yi Lin Gai Cuo. Beijing:People's Military Medical Press 2007.
12. Li JH, Liu AJ, Li HQ, et al. Buyang Huanwu Decoction for healthcare: evidence-based theoretical interpretations of treating different diseases with the same method and target of vascularity. Evid Based Complement Alternat Med 2014, 2014: 506783.
13. Li WZ, Wang WX, Zhang LL. Meta analysis of Buyang Huanwu Decoction for the treatment of Qi deficiency and blood stasis type of angina pectoris.Global Tradit Chin Med 2012, 5: 813-818.
14. Zhang W, Gao K, Liu J, et al. A review of the pharmacological mechanism of traditional Chinese medicine in the intervention of coronary heart disease and stroke. Afr J Tradit Complement Altern Med 2013, 10: 532-537.
15. Zhang ZQ, Tang T, Luo JK, et al. Effect of qi-tonifying and stasis-eliminating therapy on expression of vascular endothelial growth factor and its receptors Flt-1, Flk-1 in the brain of intracerebral hemorrhagic rats. Chin J Integr Med 2007, 13:285-290.
16. Chen HH, Fu JJ. Advances in research on diabetic complications treated by Buyang Huanwu Decoction.Chin Foreign Med Res 2012, 10:152-153.
17. Liu GH, Liu A, Zheng YZ. Influence of Jiawei Buyang Huanwu Tang on apoptosis of retinal microvessel pericytes in rats with diabetes mellitus. J Beijing Univ Tradit Chin Med 2013, 36: 178-182.
18. Tang AH, Li LY, Zhou WH. Influence of Buyanghuanwu Decoction on hemorheology in patients with simple diabetic retinopathy. Hebei J Tradit Chin Med 2007, 29: 929-931.
19. Y. Chen, Yang GH. The treatment of diabetic retinopathy with the combination of double frequency laser and buyang huanwu decoction.Central Plains Med J 2008, 35: 21-23.
20. Jin WE, Liu A. Clinical research of Jiawei buyang huanwu decoction on treatment of nonproliferative diabetic retinopathy. J Tradit Chin Ophthalmol 2008,18: 270-272.
21. Lu MJ, Zhang T. Clinical treatment of Zhenwu Decoction in recent years. Liaoning J Tradit Chin Med 2015, 42: 1145-1146.
22. Xiao CY. Clinical application and pharmacological study of Zhenwu Decoction. Hubei College Traditional Chinese Medicine 2007.
23. Wei GJ, Gao P. Clinical observation on Zhenwu decoction for treatment of elderly type 2 diabetic retinopathy. Chin J Exp Tradit Med Formulae 2012,18: 311-313.
24. Zhu KJ, Du FZ, Chang R. Treatment effect observation of Zhenwu decoction in the treatment of elderly type 2 diabetic retinopathy. China Health Stand Manag 2014, 15: 3-4.
25. Li HC, Xu YY. Clinical efficacy review and economic evaluation of Qiming Granule for diabetic retinopathy. Drugs Clinic 2014, 11: 33-39.
26. Duan JG, Liao LZ, Wu L, et al. Randomized controlled double-blind multicentric clinical trail on non-proliferative diabetic retinopathy treated by Qi-ming Granule. J Chengdu Univ Tradit Chin Med 2006, 29: 1-5.
27. Zhang LL. Study on preparation technology and quality standard of QM Granule [Dissertation, thesis].School of Pharmacy, Zhejiang University 2008.
28. Li L. Pharmacological study on rehmannia in treatment of diabetes. J Changchun Univ Tradit Chin Med 2011, 27: 670-672.
29. Hu ZF, Wang XP, Chen JZ. Determination of monosaccharide content in different processed radix rehmannia praeparata by HPLC-ELSD. Chin J Exp Tradit Med Formulae 2013, 19: 72-74.
30. Chen XG. Determination of catalpol in radix rehmanniae from different sources by HPLC. Anhui Med Pharm J 2012, 16: 910-911.
31. Shang WQ, He QH, Zhang JJ. Study on the changes of Verbascoside in the process of Radix Rehmanniae.J New Chin Med 2014, 46: 209-211.
32. Zhang WM, Jia YR, Fu JN, et al. RP-HPLC simultaneous determination of five nucleosides in Radix Rehmanniae Preparata. Chin J Pharm Anal 2013, 33: 94-97.
33. Luo XX, Duan JG, Liao PZ, et al. Effect of Qiming Granule on retinal blood circulation of diabetic retinopathy: aa multicenter clinical trial. Chin J Integr Med 2009, 15: 384-388.
34. Huang J, Wang LB, Liu LL. Effect of calcium dobesilate combined with Qiming granule therapy on choroid as well as serum branched chain amino acids and cytokines in patients with non-proliferative diabetic retinopathy. J Hainan Med Univ 2016, 22:2202-2208.
35. Feng HJ, Zhou HD, Song WH. Clinical study on non-proliferative diabetic retinopathy patients treated with Qiming Granule combining with Xueshuantong Capsule. Chin J Tradit Med Sci Techol 2015, 22:255-256.
36. Dong RJ, F. Chen, Zhao X, et al. Clinical observation of pan-rephotocoagulation combined with drug treatment for diabetic retinopathy. Chin J Chin Ophthalmol 2015, 25: 114-117.
37. Ye HJ, Duan JG, Liao PZ. Effects of Qiming Granule on the polyol pathway tissue of diabetic rats. J Chin Ophthalmol Otorhinolaryngol 2011, 1: 24-26.
38. Liu AQ, Liao PZ, Zheng YL, et al. Effect of qiming granule on antioxidatizing reaction in the retinal tissue of diabetic rats. J Traditi Chin Ophthalmol 2003, 13: 128-130.
39. Ye XM, Wu BL. Effect observation and changes of VEGF and IGF-1 detection by Qiming Granule in elderly patients with non-proliferative diabetic retinopathy. Chin Mod Dr 2013, 51: 99-112.
40. Liu LH, Liao PZ, Duan JG. Effect of Qiming on retinal IGF -1 in experimental diabetic rats. The 7th National Symposium on TCM Diabetes 2003:239-242.
41. Li KJ, Zhao ZH, Fan F, et al. Effect of Qi Ming Granule on the choroidal circulation in diabetic patients. Int Eye Sci 2016, 16: 499-501.
42. Sheng S, Wang J, Wang L, et al. Network pharmacology analyses of the antithrombotic pharmacological mechanism of Fufang Xueshuantong Capsule with experimental support using disseminated intravascular coagulation rats. J Ethnopharmacol 2014, 154: 735-744.
43. Pang HH, Li MY, Wang Y, et al. Effect of compatible herbs on the pharmacokinetics of effective components of Panax notoginseng in Fufang Xueshuantong Capsule. J Zhejiang Univ Sci B 2017,18: 343-352.
44. Jiao H. Intervention of compound Xueshuantong Capsule on diabetic retinopathy in hemorrhage period.Chin J Tradit Chin Med Pharm 2010, 25: 1535-1536.
45. Jian W, Yu S, Tang M, et al. A combination of the main constituents of Fufang Xueshuantong Capsules shows protective effects against streptozotocininduced retinal lesions in rats. J Ethnopharmacol 2016, 182: 50-56.
46. Cheng YX. Clinical effect observation of compound Xueshuantong Capsule in the treatment of diabetic retinopathy. Guide Chin Med 2013, 11: 215-216.
47. Wang YY, Liu YX, Mai SY, et al. Retinal hemodynamic influence of compound xueshuantong capsule on nonproliferative diabetic retinopathy after laser photocoagulation. Int Eye Sci 2014, 14:1327-1328.
48. Zhu YX, Li J, Ying J. Efficacy of compound Xueshuantong capsules in the treatment of non-proliferative diabetic retinopathy. Mod Chin Dr 2016, 54: 60-66.
49. Pei R, Gao H. Clinical effects and hs-CRP, VEGF and IGF-1 levels of Xueshuangtong capsule combined with Calclum Dobesllate in treatment of early diabetic retinopathy. Mod J Integr Tradit Chin West Med 2015, 24: 3896-3907.
50. Xing YW, Zou JJ, Shi YQ, et al. Protection of Fufang Xueshuantong Capsule against retinal oxidative damage of diabetic rats. J Med Res 2016, 45: 40- 43.
51. Duan H, Huang J, Li W, et al. Protective effects of fufang xueshuantong on diabetic retinopathy in rats.Evid Based Complement Alternat Med 2013, 2013:408268.
52. Zhou L, Yu Q, Chen X, et al. Anti-hypoxia and anti-oxidation effect of Fufang Xueshuantong capsule on the retina of diabetic rats. Chin J Optom Ophthalmol Vis Sci 2012, 14: 41-46.
53. Luo J, Xu H, Chen K. Systematic review of compound danshen dropping pill: a chinese patent medicine for acute myocardial infarction. Evid Based Complement Alternat Med 2013, 2013: 808076.
54. Han LN, Li YM, Xie B. Research progress of compound Danshen Dropping Pill in the treatment of non-proliferative diabetic retinopathy. Chin Tradit Patent Med 2015, 37: 382-384.
55. Qi CX, Tan XH, Li QG, et al. Clinical study of diabetic retinopathy treated by compound danshen dripping pills. Zhong Yao Cai 2007, 30: 375-377.
56. Lian FM, Wu L, Tian JX, et al. The effectiveness and safety of a danshen-containing Chinese herbal medicine for diabetic retinopathy: a randomized,double-blind, placebo-controlled multicenter clinical trial. J Ethnopharmacol 2015, 164: 71-77.
57. Luo D, Qin Y, Yuan W, et al. Compound Danshen Dripping Pill for treating early diabetic retinopathy: a randomized, double-dummy, double-blind study.Evid Based Complement Alternat Med 2015, 2015:539185
58. Yang PJ, Yang SM, Lv YP, et al. Effect of compound Danshen Droppills on vascular endothelial function in early diabetic retinopathy patients. Chin J Exp Tradit Med Formulae 2013, 19: 340-343.
59. Kern TS. Contributions of inflammatory processes to the development of the early stages of diabetic retinopathy. Exp Diabetes Res 2007: 95-103.
60. Malecki MT, Osmenda G, Walus-Miarka M, et al.Retinopathy in type2 diabetes mellitus is associated with increased intima-media thickness and endothelial dysfunction. Eur J Clin Invest 2008, 38:925-930.
61. Isah T. Rethinking Ginkgo biloba L: Medicinal uses and conservation. Pharmacogn Rev 2015, 9: 140-148.
62. Dubey AK, Shankar PR, Upadhyaya D, et al. Ginkgo biloba- an appraisal. Kathmandu Univ Med J 2003, 2:225-229.
63. Liu W, Li H. Pharmacological functions of Ginkgo biloba extract and its clinical research progress in eye diseases. Int J Ophthalmol 2008, 8: 1647-1649.
64. Biber A. Pharmacokinetics of Ginkgo biloba extracts.Pharmacopsychiatry 2003, 36 Suppl 1: S32-S37.
65. Xia XH, Zhang Y, Xi YB. Advances in studies on chemical constituents and bioactivites actions of Ginkgo biloba L. Chin J Exp Tradit Med Formulae 2009, 15:100-104.
66. Brondino N, De Silvestri A, Re S, et al. A systematic review and meta-analysis of Ginkgo biloba in neuropsychiatric disorders: from ancient tradition to modern-day medicine. Evid Based Complement Alternat Med 2013, 2013: 915691.
67. Mo L. Clinical research progress of the Ginkgo biloba extract. Global Tradit Chin Med 2010, 3:237-240.
68. Evans JR. Ginkgo biloba extract for age-related macular degeneration. Cochrane Database Syst Rev 2000: CD001775.
69. Hirooka K, Tokuda M, Miyamoto O, et al. The Ginkgo biloba extract (EGb 761) provides a neuroprotective effect on retinal ganglion cells in a rat model of chronic glaucoma. Curr Eye Res 2004,28: 153-157.
70. Huang SY, Jeng C, Kao SC, et al. Improved haemorrheological properties by Ginkgo biloba extract (Egb 761) in type 2 diabetes mellitus complicated with retinopathy. Clin Nutr 2004, 23:615-621.
71. Zhu CY, Yi Q, Ma JL, et al. Clinical evaluation of Ginkgo biloba extract for diabetic retinopathy. Int Eye Sci 2016, 16: 361-364.
72. Li CR, Sun SG, Jiang DY, et al. Effects of Ginkgo biloba extract on diabetic retinopathy. Chin J Ophthalmol Tradit Chin Med 2006, 16: 153-156.
73. Li X, Wu LH, Liu W, et al. A network pharmacology study of Chinese medicine QiShenYiQi to reveal its underlying multi-compound, multi-target, multipathway mode of action. PLoS One 2014, 9: e95004.
74. Ge YB, Mao JY. Study on the distribution characteristics of the TCM syndromes of 7512 coronary artery disease patients. Shandong J Tradit Chin Med 2011, 4: 227-229.
75. Hou YZ, Wang S, Zhao ZQ, et al. Clinical assessment of complementary treatment with Qishen Yiqi dripping pills on ischemic heart failure: study protocol for a randomized, double-blind, multicenter,placebo-controlled trial (CACT-IHF). Trials 2013, 14,138.
76. Zhang L, Wang Y, Yu LY, et al. QI-SHEN-YI-QI accelerates angiogenesis after myocardial infarction in rats. Int J Cardiol 2010, 143: 105-109.
77. Li YF, Qu HB, Cheng YY. Identification of major constituents in the traditional Chinese medicine‘QI-SHEN-YI-QI’dropping pill by high-performance liquid chromatography coupled with diode array detection electrospray ionization tandem mass spectrometry. J Pharm Biomed Anal 2008, 47:407-412.
78. Li Y, Wang Y, Qu H, et al. Simultaneous determination of seven bioactive compounds in Chinese medicine ‘QI-SHEN-YI-QI’dropping pill by LC-UV and LC-ELSD. Chromatographia 2008, 67:293-297.
79. Zhang Y, Shi P, Yao H, et al. Metabolite profiling and pharmacokinetics of herbal compounds following oral administration of a cardiovascular multi-herb medicine (Qishen Yiqi Pills) in rats. Curr Drug Metab 2012, 13: 510-523.
80. Yuan W, Jin M, Deng H. Influence of Qishen Yiqi Gutta Pills on expression of AGEs and RAGE mRNA in rats with diabetic retinopathy. Chin J Chin Ophthalmol 2012, 22: 14-17.
81. Yuan W, Jin M, Pan L, et al. Influence of Qishenyiqi Gutta Pills on expression of ICAM-1 in rats with diabetic retinopathy. J Beijing Univ Tradit Chin Med 2010, 33: 262-265.
82. Yuan W, Jin M, Deng H. Influence of Qishenyiqi Gutta Pills on expression of vascular endothelial growth factor and pigment epithelium derived factor in retina of diabetic rats. J China-Japan Friendship Hosp 2013, 27: 25-29.
83. Deng H, Jin M, Yuan W. Effect of Qishenyiqi Pills on expression of glutamate-aspartate transporters and glutamine synthetase in diabetic rat’s retina. China J Chin Ophthalmol 2011, 21: 197-200.
84. Fang L, Fan YP, Wang L. Study on the clinical application of Liuwei Dihuang Pill (Decoction). J Tradit Chin Med 2013, 28: 2181-2184.
85. Xie Q. Research on the effect of Liuwei Dihuang pills on treating type 2 diabetes. Clin J Chin Med 2013, 5: 116-118.
86. Pu R, Geng XN, Yu F, et al. Liuwei Dihuang pills Enhance the effect of western medicine in treating type 2 diabetes: a meta-analysis of randomized controlled trials. Chin J Integr Med 2013, 19:783-791.
87. Zhao Y, Yu J, Liu J, et al. The role of Liuwei Dihuang Pills and Ginkgo Leaf Tablets in treating diabetic complications. Evid Based Complement Alternat Med 2016, 2016: 2931314.
88. An XF, Zhao Y, Yu JY. Treatment of early diabetic retinopathy by Liuwei Dihuang Pill combined Ginkgo Leaf Tablet. Chin J Int Tradit West Med 2016,36: 674-677.
89. Zhao BC, Wu HQ, Zhao T, et al. Literature review of Naoxintong Capsules’statins characteristic effect.China Med Herald 2016, 13: 49-53.
90. Xu H, Jin J, Chen L, et al. Naoxintong/PPARalpha signaling inhibits H9c2 cell apoptosis and autophagy in response to oxidative stress. Evid Based Complement Alternat Med 2016, 2016: 1-10.
91. Lv P, Tong X, Peng Q, et al. Treatment with the herbal medicine, naoxintong improves the protective effect of high-density lipoproteins on endothelial function in patients with type 2 diabetes. Mol Med Rep 2016, 13: 2007-2016.
92. Wang Y, Zhang Y, Wang XY, et al. Pharmacoeconomic analysis of Naoxintong capsule based on meta-analysis. Chin J Evid Based Cardiovasc Med 2016, 8: 1379-1385.
93. Wei MX, Du LY. Traditional Chinese medicine.Nanjing: Southeast University press 2004.
94. Liu MY, Pan Q, Chen YL, et al. NaoXinTong inhibits the development of diabetic retinopathy in db/db mice. Evid Based Complement Alternat Med 2015,2015: 242517.
 Traditional Medicine Research2018年2期
Traditional Medicine Research2018年2期
- Traditional Medicine Research的其它文章
- History of recurrent miscarriage in traditional Chinese medicine literature
- A systematic summary of natural compounds in Radix Glycyrrhizae
- Pharmacological intervention of traditional Chinese medicine for the quality of life in patients with colorectal cancer: a systematic review and meta-analysis
- Meta-analysis of neostigmine injections given at the Zusanli (ST 36) acupoint in the treatment of postpartum urinary retention
