History of recurrent miscarriage in traditional Chinese medicine literature
Li-Lin Yng , Jie Go , Hi-Wng Wu , Song-Ping Luo ,*
aFirst School of Clinical Medicine, Guangzhou University of Chinese Medicine, Guangzhou, China. bDepartment of Gynecology, First Affiliated Hospital, Guangzhou University of Chinese Medicine, Guangzhou, China.
Background
Recent guidelines define recurrent miscarriage (RM) as a fertility defect in which two or more consecutive pregnancy losses occur before 20 weeks of gestation.Approximately 1-2% of women of reproductive age have this abnormality [1-3]. RM induces physical and psychological disorders in female patients, and it can even destabilize marriage and family, making it a considerable challenge for gynecologists. Therefore,studies on the prevention and treatment of RM have vital clinical and social importance. Traditional Chinese medicine (TCM) has been practiced in China for thousands of years. Recently, the treatment of diseases such as RM, leukemia, and malaria with TCM as a complementary therapy is getting more attention [4-12].Although a wider clinical application of TCM is limited because of the lack of quantitative studies and systematic analyses, successful reports such as the discovery of arteannuin, the active ingredient of Qinghao (Herba Artemisiae Annuae), suggest that TCM remains a rich source of new therapeutic targets [8]. In this study, we summarized the information on RM in the TCM literature in chronological order to increase the understanding among conventional medicine practitioners.
Historical records in the TCM literature
The TCM theory was first described in the Chinese medicine classic book Huangdineijing. This book was a combined effort of many unknown authors from the Warring States period to the Han Dynasty of China (475 B.C. – 220 A.D.). This book contains two parts, Suwen and Lingshu. The book did not refer to RM as a disease but laid a solid foundation for the understanding of reproduction by correlating RM to the function of the kidneys. This concept is essential for all RM treatments in TCM. Chapter 1 of Suwen describes the strong association between the kidneys and reproduction during seven 7-year cycles, from childhood to the postmenopausal period (Table 1).
Despite its simplicity, this book is a comprehensive overview of the female reproductive cycle considering the time it was written. Moreover, chapter 47 of Suwen stressed that “the meridian of the uterus is linked to the kidney” [13].
The first cases of RM as a fertility abnormality were reported in Chanjing, written during the Nanbei Dynasty of China (420 A.D. – 589 A.D.). Thereafter, RM was formally established as a disease by TCM practitioners and was studied more extensively in China. In Chanjing,RM was defined as multiple natural miscarriages, and Damaidoushi Decoction was recommended as a treatment,although this treatment was never prescribed in modern medicine. Chanjing acknowledged the importance of RM.
Another significant breakthrough in the treatment of RM was reported in the Zhubingyuanhoulun by Chao Yuanfang during the Sui Dynasty of China (581 A.D. –618 A.D.), and this treatise was the first to describe the etiology and pathogenesis of RM. Miscarriage was discussed in detail in the chapter“Pregnancy with miscarriage”. It was suggested that deficiency of Qi and blood, in addition to kidney deficiency, led to the underdevelopment of the fetus and eventually miscarriage.The major reason for this pathogenesis is that the kidney controls the meridian of the uterus, and pregnant women with severe lumbago are at a high risk for natural miscarriage [14]. These views agreed with those proposed in Huangdineijing and established the primary etiology of RM.
The knowledge of gynecology and obstetrics in TCM was further popularized for the general public without a medical background in another classic book, Nükebaiwen,written by Qi Zhongfu in question and answer form during the Beisong Dynasty of China (960 A.D. – 1127 A.D.). Question 58 indicated that the occurrence of miscarriage usually at the same time of pregnancy was a key clinical feature of RM [15]. TCM practitioners during this period started to realize that it was essential to raise awareness in the general public about the early diagnosis,treatment, and prevention of RM. In this same period,Chen Ziming systematically summarized the medications contraindicated during pregnancy in Furendaquanliangfang as a form of RM prevention [16]. The information still serves as an important guidance in modern medicine for clinical use in pregnancy because of its comprehensiveness.
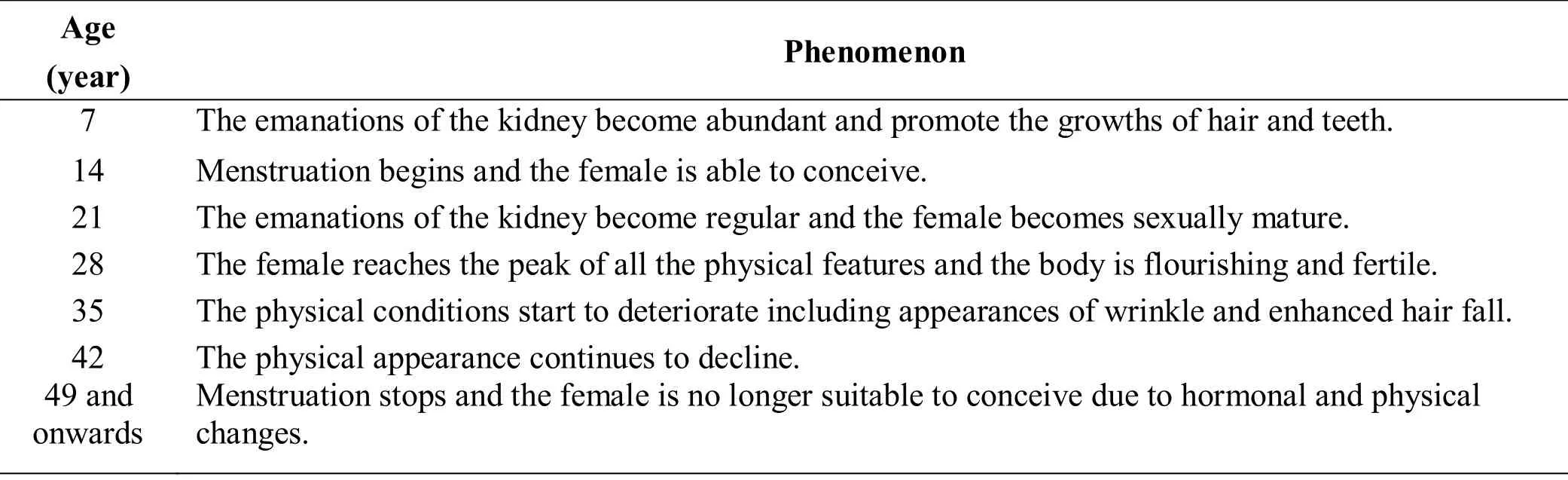
Table 1 7 cycles of female reproduction described in Huangdineijing
During the Ming Dynasty (A.D. 1368 – A.D. 1644) and the Qing Dynasty of China (A.D. 1644 – A.D. 1912),there was a greater understanding of the etiology,pathogenesis, treatment, and prevention of RM. In the Ming Dynasty of China (1368 A.D. – 1644 A.D.), Zhang Jingyue, a well-known TCM expert, published his lifetime experience in Jingyuequanshu, which contained 64 volumes [17]. It was a comprehensive publication in clinical practice, and part of the book was devoted to discussing the etiology, syndrome, pulse, therapeutic principle, and treatment of major gynecologic diseases.RM was described in detail in chapter 26, volume 38.Zhang presented the etiology and pathogenesis of RM in detail and observed that the underlying causes of RM were the deficiency of Qi, weak pulse, old age, emotional instability, lechery, falls, and improper diet. Second,Zhang proposed that RM should be treated with preventive therapy. This proposal agrees with current clinical practice where the body is recuperating before pregnancy. Of note, Zhang developed two famous prescriptions for RM: Taiyuan Decoction and Taishanpanshi Powder (Table 2). These TCM prescriptions are the most common, have significant clinical efficacy, and are prescribed by TCM practitioners to date [18, 19]. Wan Quan, another famous physician during the Ming Dynasty of China (1368 A.D. – 1644 A.D.) also explained the etiology of RM in his publication, Guangsijiyao. He suggested that women who had RM tended to be emotionally unstable and consumed food that elicited strong responses from the body, leading to the damage of the Chong and Ren meridians [20].These interpretations incorporate the concept of holism from the TCM theory, which regards the human body as a unity and postulates that body integrity is affected by many factors, including mood, diet, body shape, and the environment, all of which will eventually contribute to the disease state.
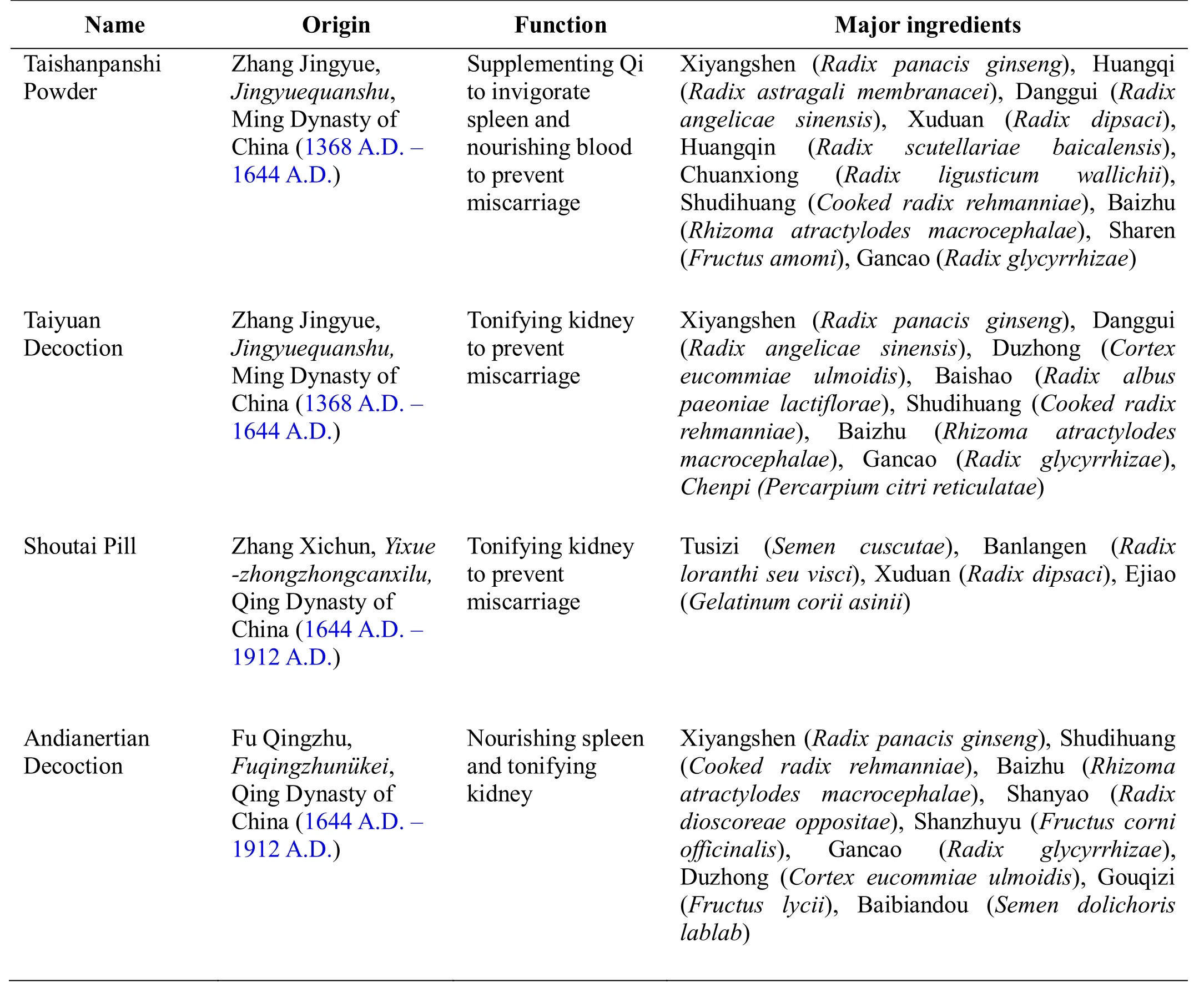
Table 2 Classic prescriptions treating recurrent miscarriage
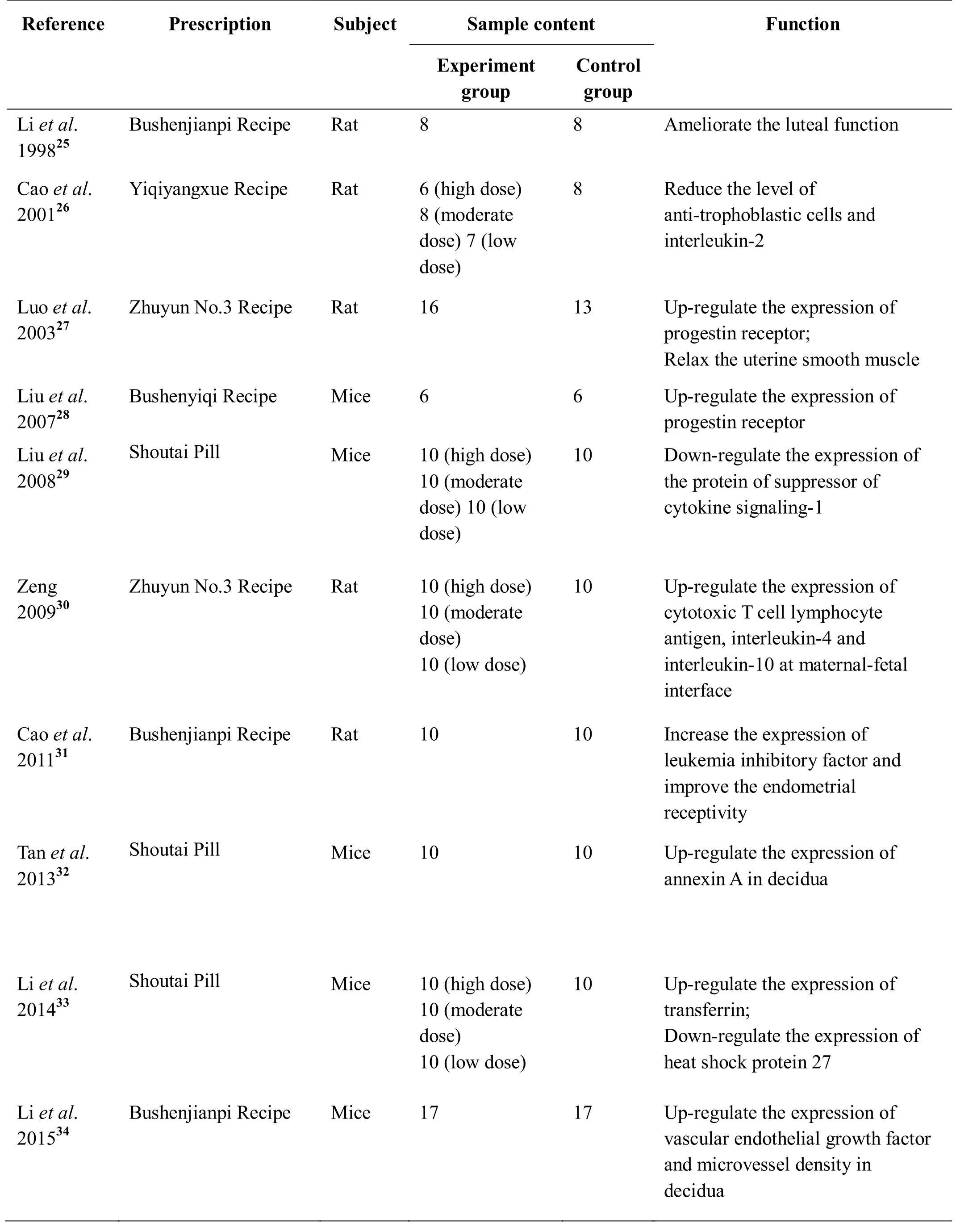
Table 3 Modern prescriptions for recurrent miscarriage
During the Qing Dynasty of China (1644 A.D. – 1912 A.D.), Huatai, the terminology of RM in TCM, was first described in two books, Yizongjingjian by Wu Qian and Yeshinükezhengzhi by Ye Tianshi [21, 22]. Huatai is widely accepted by TCM practitioners and is found in contemporary textbooks [23]. Zhang Xichun, a renowned physician during the Qing Dynasty of China (1644 A.D. –1912 A.D.), was the first to combine TCM and conventional medicine. He described a standard prescription for RM, Shoutai Pill, in his representative work, Yixuezhongzhongcanxilu. This prescription is considered highly effective and is still widely used in clinical practice [24] (Table 2). Modern pharmacological studies on animal models identified mechanisms that could explain the effect of this therapy on RM [25-34](Table 3). The ingredients of the Shoutai Pill include Tusizi (Semen cuscutae), Banlangen (Radix loranthi seu visci), Xuduan (Radix dipsaci), and Ejiao (Gelatinum corii asinii). In another book from the same period,Fuqingzhunüke, the author Fu Qingzhu emphasized the importance of organs essential for metabolism, including the liver, spleen, and kidney, in the pathogenesis of gynecologic diseases [35]. The recommended prescription for RM was the Andianertian Decoction (Table 2). The theoretical basis of this therapy was related to the function of the kidney and spleen in TCM theory.According to TCM, the kidney governs the congenital constitution whereas the spleen governs the acquired constitution. If the congenital and acquired constitutions are stable, the fetus will develop normally and vice versa.Another pioneering anatomist and TCM practitioner during the Qing Dynasty of China (1644 A.D. – 1912 A.D.), Wang Qingren, correlated RM to blood circulation.He proposed the theory of “Blood Stasis Causing Disease” and developed standard prescriptions for improving blood circulation and reducing stasis [36]. The prescription was discussed in his major work, Yilingaicuo.Wang suggested that RM was caused by blood stasis, and treatment should be based on the improvement of blood circulation.
With the introduction of conventional medicine in China in the twentieth century, both the understanding and treatment of RM have made considerable progress. In 1982, Luo Yuankai, an eminent expert in gynecology in TCM, defined the female reproductive axis that governs female reproduction in the context of TCM, which is similar to the hypothalamic-pituitary-ovarian axis in conventional medicine. The female reproductive axis is an improvement of the TCM theory in gynecology and serves as an important guideline for the treatment of RM and other gynecologic diseases. Furthermore, the concept of combining traditional and western medicine has been gradually accepted by many physicians in both TCM and conventional medicine [37-39]. The development of modern medical diagnosis promotes the standardization of TCM [40]. In addition, pharmaceutical companies have developed TCM patent prescriptions, including Zishenyutai Pill by Baiyunshan Zhongyi Pharmaceutical Company of Guangzhou and Gushenantai Pill by Boran Pharmaceutical Company of Beijing. The TCM patent prescriptions are manufactured in the form of pills and syrup to allow easy preparation and consumption.
Modern researches on RM
Nowadays, the mainstream therapeutic strategy for RM in TCM is divided into two stages: treatment before pregnancy and tocolysis after pregnancy. Treatment before pregnancy lasts for 3 to 6 months depending on the TCM practitioners’ judgement. According to the concept of differential diagnosis in TCM, treatment before pregnancy aims at improving the function of the kidney and spleen, followed by detoxification and improvement of blood circulation. After fertilization, tocolysis is performed for the control of the Chong and Ren meridians and is the key to successful therapy. In addition,modern TCM practitioners employ new medical tools and biomarkers, including ultrasonography and human chorionic gonadotropin, for the regular monitoring of fetal development.
In the last two decades, modern pharmacological studies on Chinese herbs for RM have been conducted using single ingredients and whole plants [25-34].Modern medical research usually focuses on a single drug to avoid confounding factors. However, many active ingredients have synergistic effects when used in combination. Therefore, it is essential to assess the pharmacology, safety, and efficacy of these products considering the entire prescription. These studies have identified the following mechanisms that could explain the therapeutic effects on RM: (1) improvement of the quality of follicles and endometrial receptivity [31], (2)amelioration of luteal function [25], (3) regulation of immune responses [30], (4) improvement of the prethrombotic state [41], (5) upregulation of the expression of the progestin receptor in the maternal-fetal interface [27-28], and (6) control of hysteromyoma and endometriosis [42-43]. Table 3 lists the major studies(searched from January 1996 to December 2015 in the China National Knowledge Infrastructure database) that have investigated the mechanisms of TCM drugs for RM[25-34]. In addition, some clinical trials evaluated the therapeutic effect of TCM on RM. Yang and colleagues conducted a systematic review of Chinese herbal medicines and found that the administration of medicines such as Shoutai Pill and Antai Decoction increased the live birth rates and improved the embryonic development in women with RM [44]. However, the methodologies on randomization, baseline definition, and sampling were not comprehensive in most of the studies [44, 45].
Conclusion
Because of the complexity and diversity of the herbs used in TCM prescriptions and the lack of quantitative studies,more evidence from properly controlled studies is needed.We believe that this review may trigger future interest in evaluating the pathogenesis and treatment of RM in the context of TCM and may allow the development of systematic pharmacological and clinical studies and a better evaluation of the therapeutic effects of TCM on RM.
1. American College of Obstetricians and Gynecologists. ACOG practice bulletin. Management of recurrent pregnancy loss. Number 24, February 2001. (Replaces Technical Bulletin Number 212,September 1995). American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet 2002, 78:179-190.
2. Pandey MK, Rani R, Agrawal S. An update in recurrent spontaneous abortion. Arch Gynecol Obstet 2005, 272: 95-108.
3. Diejomaoh MF. Recurrent spontaneous miscarriage is still a challenging diagnostic and therapeutic quagmire. Med Princ Pract 2015, 24 Suppl 1: 38-55.
4. Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril 2012, 98: 1103-1111.
5. Liu GC, Gao BL, Yang HQ, et al. The clinical absolute and relative scoring system-a quantitative scale measuring myasthenia gravis severity and outcome used in the traditional Chinese medicine.Complement Ther Med 2014, 22: 877-886.
6. Hsiao YL, Chang PC, Huang HJ, et al. Treatment of acute lymphoblastic leukemia from traditional Chinese medicine. Evid Based Complement Alternat Med 2014, 2014: 601064.
7. Kajimoto S, Takanashi N, Kajimoto T, et al.Sophoranone, extracted from a traditional Chinese medicine Shan Dou Gen, induces apoptosis in human leukemia U937 cells via formation of reactive oxygen species and opening of mitochondrial permeability transition pores. Int J Cancer 2002, 99:879-890.
8. Tu Y. The discovery of artemisinin (qinghaosu) and gifts from Chinese medicine. Nat Med 2011, 17:1217-1220.
9. Tu Y. The development of the antimalarial drugs with new type of chemical structure--qinghaosu and dihydroqinghaosu. Southeast Asian J Trop Med Public Health 2004, 35: 250-251.
10. Wei L. Xiaojin Bolus’s anti-tumor acitivity and molecular biological mechanism. Fuzhou: Fujian University of Chinese Medicine, 2006.
11. Song R. The mechanism study of Dahuang Zhechong Pill on liver cancer. Ji’nan: Shandong University of Chinese Medicine, 2008.
12. Liu L. Clinical and experimental study on chronic myeloid leukemia-chronic phase by adding flavored sting rhubarb worm pills. Shandong Unive Chin Med,2009.
13. Emperor Y. Huang Di Nei Jing•Su Wen. Beijing,China: People’s Medical Publishing House, 1963.
14. Chao YF. General treatise on the causes and symptoms of diseases. Beijing, China: People’s Medical Publishing House, 1956.
15. Qi ZF. One hundred question for gynecology and obstetrics. Shanghai: Shanghai Classics Publishing House, 1983.
16. Chen ZM. Complete effective prescriptions for women’s diseases. Beijing: People’s Medical Publishing House, 1984.
17. Zhang JB. Complete works of Jingyue. Shanghai:Shanghai Medical Publishing House, 1958.
18. Li Y. The effect on 40 cases of recurrent miscarriage treated with Taishan Panshi Powder. Guide Chin Med 2013, 11: 598-599.
19. Jin D, Bai Z. The effect of modified Taiyuan Decoction on recurrent miscarriage. J Jilin Tradit Chin Med 1991, 3: 23.
20. Wan Q. The key of fertility handed down from the older generation of Wan’s family. Wuhan: Hubei Science and Technology Press, 1986.
21. Wu Q (Qing Dynasty). Yi Zong Jin Jian. Beijing:People’s Medical Publishing House, 1956.
22. Ye G (Qing Dynasty). Ye Shi Nü Ke Zheng Zhi.Beijing: China Press of Traditional Chinese Medicine,2015.
23. Zhang Y. Gyencology of Traditional Chinese Medicine. Beijing: China Press of Traditional Chinese Medicine, 2007.
24. Gao J, Luo S. Clinical observation of Shoutai Pills for treatment of early threatened abortion. J New Chin Med 2011, 43: 81-83.
25. Li XQ. The effect of Tonifying Kidney and Strengthening Spleen Recipe for the progestin and progetin receptor of pregnant rats. J Guangzhou Univ TCM 1998, 15: 49-51.
26. Cao LX, Han B, Li TX, et al. Experimental study of Tonifying Qi and Nourishing Blood Recipe for deficiency kidney abortion immunologic factors.Tianjin J Tradit Chin Med 2001, 18: 35-37.
27. Luo SP, Liang GZ, Zhang YZ, et al. Study on mechanism of No.3 Aiding Pregnancy Recipe for preventing and treating spontaneous abortion. Chin J Integr Tradit West Med 2003, 23: 522-525.
28. Liu YJ, Huang GY, Yang MW, et al. Effects of Bushenyiqi Recipe on endometrial morphology and PR during implantation in dysfunction mice. J Zhejiang Univ TCM 2007, 31: 690-692.
29. Liu HP, You ZL, Lu FG, et al. The Effect of Longevity Pill on the expression of the protein-SOCSI at the decidua tissues of mice with recurrent spontaneous abortion. Guiding J Tradit Chin Med Pharm 2008, 14: 6-8.
30. Zeng C. Research on expression of CD80/CD86 of decidua tissue in abortion rats model with kidney deficiency and Th2-type immunity deviation in abortion rats induced by TCM. Guangzhou:Guangzhou University of Chinese Medicine, 2008.
31. Cao L, Luo SP, Ou RQ. Influence of kidney-tonifying and spleen-invigorating herbs on endometrial receptivity of kidney deficiency model rats. Chin J Tradit Chin Med Pharm 2011, 26: 1057-1061.
32. Tan ZW, Lei L, Li HF, et al. Influence of Longevity Fetal Pill on expression of annexin A2 in decidual tissues in mice with recurrent abortion. J Beijing Univ TCM 2013, 36: 680-683.
33. Li HF, Lei L, Tan ZW, et al. Effect of Longevity Pill on the expression of uterus decidual HSP27 and Tf in recurrent spontaneous abortion model mice. Chin J Tradit Chin Med Pharm 2014, 29: 745-748.
34. Li WL, Xiong CQ. Influence of Tonifying Kidney and Strengthening Spleen Recipe on expression of VEGF and MVD in decidual tissues in mice with recurrent abortion. Anhui Med Pharm J 2015, 19:27-30.
35. Fu S. Qingzhu Fu’s gynecology and obstetrics.Shanghai: Shanghai science and Technology Press,1959.
36. Wang QR (Qing Dynasty). Yi Lin Gai Cuo. Shanghai:Shanghai Medical Publishing House, 1956.
37. Luo Y. The association between gynecology and kidney energy, Tiangui, Chongren. Shanghai J Tredi Chin Med 1983, 1: 11-13.
38. Liu M. The female reproductive axis theory of Yuankai Luo. Beijing: China News of Traditional Chinese Medicine 2014.
39. Lv A, Liu M, Zhang C, et al. The 30-year review of combining Traditional and Western Medicine. Chin J Integrated Tradit Chin Western Med 2011, 31:1445-1458.
40. Wang J, Guo Y, Li GL. Current status of standardization of traditional Chinese medicine in China. Evid Based Complement Alternat Med 2016,2016: 9123103.
41. Li Y, Wang J, Liu Y, et al. The clinical observation of promoting blood circulation on recurrent miscarriage with prethrombotic state. J Guangzhou Univ Tradit Chin Med 2015, 32: 1000-1004.
42. Chen N. The systematic review of the effect of Chinese medicine on hysteromyoma. Beijing: Beijing University of Chinese Medicine, 2015.
43. Li X, Wan G. The research progress of mechanism of Chinese medicine on endometriosis. Modern J Integr Tradi Chin Western Med 2015, 24: 210-213.
44. Yang GY, Luo H, Liao X, et al. Chinese herbal medicine for the treatment of recurrent miscarriage: a systematic review of randomized clinical trials. BMC Complement Altern Med 2013, 13: 320.
45. Luo H, Liu JP, Li Q. Methodological issues and suggestions for improvement in randomized controlled trials of Chinese herbal medicine for recurrent miscarriage. J Chin Integr Med 2012, 10:604-614.
 Traditional Medicine Research2018年2期
Traditional Medicine Research2018年2期
- Traditional Medicine Research的其它文章
- Clinical evidence and potential mechanisms of Chinese medicines for the treatment of diabetic retinopathy
- A systematic summary of natural compounds in Radix Glycyrrhizae
- Pharmacological intervention of traditional Chinese medicine for the quality of life in patients with colorectal cancer: a systematic review and meta-analysis
- Meta-analysis of neostigmine injections given at the Zusanli (ST 36) acupoint in the treatment of postpartum urinary retention
