显微镜下经腹膜后精索静脉高位结扎与显微镜下经外环口精索静脉结扎的临床效果观察
姜华龙 李萍 严跃龙 郑展图
【摘要】 目的:評价显微镜下经腹膜后精索静脉高位结扎术与显微镜下经外环口精索静脉结扎术治疗精索静脉曲张的临床效果。方法:纳入本院2012年6月-2017年1月收治的132例精索静脉曲张患者,根据手术治疗方式的不同分为观察组(n=89)与对照组(n=43),观察组患者的手术方式为显微镜下经腹膜后精索静脉高位结扎术,对照组患者的手术方式为显微镜下经外环口精索静脉结扎术,观察两组患者的并发症发生率、术中出血量、复发率、手术时间与精液质量改善状况。结果:观察组患者的手术时间明显短于对照组,差异有统计学意义(P<0.05)。两组患者的术中出血量比较,差异无统计学意义(P>0.05)。术后3个月复查精液,两组的精液质量比较,差异无统计学意义(P>0.05)。术后对两组患者进行为期6个月的随访,观察组患者的曲张复发率明显高于对照组,差异有统计学意义(P<0.05);两组的并发症发生率比较,差异无统计学意义(P>0.05)。结论:显微镜下经腹膜后精索静脉高位结扎术时间更短,显微镜下经外环口精索静脉结扎术复发率更低,两种方法近远期疗效均较好,安全性高,具备临床推广价值。
【关键词】 精索静脉曲张; 显微镜下经腹膜后精索静脉高位结扎术; 显微镜下经外环口精索静脉结扎术; 临床效果
Analysis the Clinical Efficacy of High Ligation of Retroperitoneal Spermatic Vein under Microscope and Ligation of External Spermatic Vein under Microscope/JIANG Hua-long,LI Ping,YAN Yue-long,et al.//Medical Innovation of China,2017,14(27):113-115
【Abstract】 Objective:To evaluate the clinical effect of high ligation of retroperitoneal spermatic vein under microscope and ligation of external spermatic vein under microscope in the treatment of varicocele.Method:A total of 132 patients with varicocele were enrolled in our hospital from June 2012 to January 2017,they were divided into observation group (n=89) and control group (n=43) according to the different surgical treatment methods,the operation mode of the observation group was high ligation of retroperitoneal spermatic vein under microscope,the operation of the control group was performed by ligation of the external spermatic vein under the microscope,the complication rate,blood loss,recurrence rate,operation time and semen quality improvement were observed in the two groups.Result:The operation time of the observation group was significantly shorter than that of the control group,the difference was statistically significant(P<0.05).There was no significant difference in intraoperative blood loss between the two groups(P>0.05).The semen was rechecked 3 months after operation,there was no significant difference in semen quality between the two groups(P>0.05).The patients in the two groups were followed up for 6 months after the operation,the recurrence rate of the observation group was higher than that of the control group,the difference was statistically significant(P<0.05);there was no significant difference in the incidence of complications between the two groups(P>0.05).Conclusion:Under the microscope by internal spermatic vein ligation in a shorter time,under the microscope through the outer ring ligation of varicocele recurrence rate is lower,short-term and long-term effects of the two methods are good, high safety,has clinical value.endprint
【Key words】 Cirsocele; High ligation of retroperitoneal spermatic vein under microscope; Ligation of external spermatic vein under microscope; Clinical effect
First-authors address:Donghua Hospital of Dongguan City,Dongguan 523000,China
doi:10.3969/j.issn.1674-4985.2017.27.032
精索靜脉曲张是指精索内静脉蔓状静脉丛的异常伸长、扩张和迂曲,原发性精索静脉曲张主要致病因素为精索静脉瓣膜缺如、发育不良或精索静脉肌层发育不良、薄弱[1-3]。重者可呈团块样堆积在阴囊内,引起阴囊坠胀不适。精索静脉曲张是导致男性阴囊坠胀、疼痛和不育的常见疾病,在普通人群中发病率为15%~20%,而在原发性不育中发生率可高达35%~40%,继发性不育中达75%,临床常见的手术治疗方法有腹膜后精索静脉高位结扎术、腹膜后精索高位结扎术(Palomo术)、腹腔镜下精索结扎术(腹腔镜Palomo术)、腹股沟管精索静脉结扎术、精索内静脉栓塞术(逆行、顺行)、显微镜下腹股沟管精索静脉结扎术、显微镜下外环下精索静脉结扎术、经阴囊精索静脉结扎术等,目前显微镜下外环下精索静脉高位结扎术被奉为治疗精索静脉曲张的“金标准”,但其手术时间较长,手术过程繁琐[4-5]。显微镜下腹膜后精索静脉结扎术鲜有报到,此术式手术部位较高,精索静脉血管汇聚,相对外环下手术,时间明显较短,将其疗效与金标准术式进行对比,评价推广价值,现报道如下。
1 资料与方法
1.1 一般资料 自2012年6月-2017年1月纳入本院收治的132例精索静脉曲张患者,根据手术治疗方式的不同分为观察组与对照组。观察组患者
89例,年龄26~36岁,平均(31.4±0.9)岁;对照组患者43例,年龄28~33岁,平均(30.5±0.6)岁。两组患者的一般资料比较,差异无统计学意义(P>0.05),具有可比性。告知患者此次研究的目的与方法,并自愿签署知情同意书。
1.2 方法
1.2.1 观察组 显微镜下经腹膜后精索静脉高位结扎的术,具体的手术方法:以腹股沟韧带中点上方2 cm处为起点平行于腹股沟韧带向外上方做长2~3 cm的切口,依次切开皮肤、皮下组织、腹外斜肌腱膜,钝性分开腹内斜肌和腹横肌,切开腹横筋膜,向内侧推开腹膜和肠管,于腹膜后显露精索,将精索从腹膜上分离下来,游离3~4 cm,使精索能无张力牵拉至切口处,利用Carl Zeiss Surgical GmbH显微镜在6~8倍视野下手术,先剪开精索筋膜,游离出睾丸动脉、所有精索内静脉,尽量减少淋巴管损伤。依次剪断静脉,并用1号丝线结扎精索静脉残端,查无静脉残留,动脉搏动良好后将精索复位到腹膜后,依次缝合切口。
1.2.2 对照组 显微镜下经外环口精索静脉结扎术,具体的手术方法:于患侧腹股沟外环下方1 cm处作横切口,长1.5~2 cm。依次切开皮肤、皮下,钝性分离至精索,分离并游离一段精索,将所游离精索牵出切口外。利用Carl Zeiss Surgical GmbH显微镜在6~8倍放大的显微镜下打开精索内筋膜,找到并注意保护睾丸动脉、输精管,找到并游离全部精索静脉,尽量保留淋巴管,游离全部精索静脉后,依次钳夹、剪断静脉,结扎残端,查无静脉残留、动脉搏动良好后将精索复位,依次缝合切口。
1.3 观察指标 观察两组患者的临床治疗指标,术后3个月复查精液质量。所有患者随访6个月,观察复发率与并发症发生率。
1.4 统计学处理 本次研究采用SPSS 13.0软件进行统计学处理,计量资料用(x±s)表示,比较采用t检验;计数资料以率(%)表示,比较采用 字2检验,P<0.05为差异有统计学意义。
2 结果
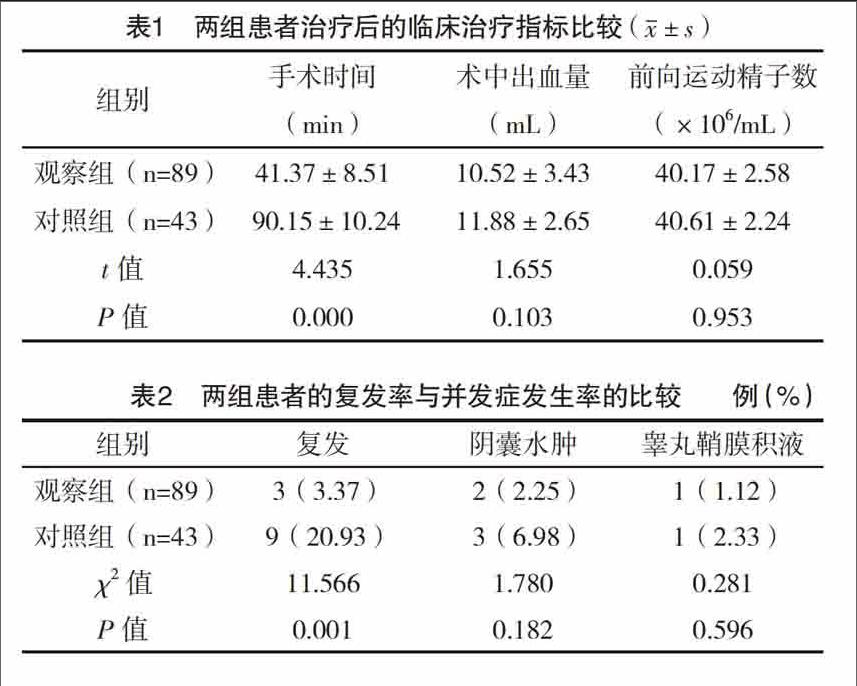
2.1 两组患者治疗后的临床治疗指标比较 治疗后,两组患者的术中出血量、精液分析比较,差异均无统计学意义(P>0.05);观察组患者的手术时间明显短于对照组,差异有统计学意义(P<0.05),见表1。
2.2 两组患者的复发率与并发症发生率比较 观察组患者的曲张复发率明显高于对照组,差异有统计学意义(P<0.05);两组患者的并发症发生率比较,差异无统计学意义(P>0.05),见表2。
3 讨论
显微镜下外环下精索静脉结扎术是当前手术治疗精索静脉曲张的金标准[6],结扎除睾丸引带静脉以外的全部静脉[7],理论上结扎静脉更多,术中结扎不止内静脉[8],还包括提睾肌静脉、输精管静脉等,结扎静脉彻底,术后复发率最低[9],但外环口处精索血管为蔓状静脉丛,需分离结扎血管达数十支,手术时间长[10],即使在显微镜下手术亦存在静脉残留引起复发的风险,且存在损伤输精管风险[11]。且对是否有必要结扎提睾肌静脉、输精管静脉等问题,很多学者有不同意见[12]。
显微镜下经腹膜后精索静脉高位结扎术经腹膜后入路,于精索高位手术[13],保留睾丸动脉、淋巴管[14],结扎全部精索内静脉,手术原理更合理。结扎静脉较少,手术时间明显减少,不存在损伤输精管风险[15]。经过临床观察、数据分析,笔者认为显微镜下经腹膜后精索静脉高位结扎术和显微镜下外环下精索静脉结扎术相比较,可有效的缩短手术时间[16],并发症无明显增加,手术效果相当,然而术后的复发率稍高[17],但经腹膜后手术难度稍高,有损伤腹膜和肠管风险,有误扎腹壁入血管风险,且不适用于肥胖患者。采取显微镜下经外环口精索静脉结扎的手术方法能够实现精准、彻底治疗[18],能够有效的降低曲张复发率,适用于所有精索静脉张患者,对于高位结扎术后复发者再次手术仍有效,因此可作为未来一段时间内治疗精索静脉曲张的首选方法[19-20]。但前者有明显的手术时间优势,手术原理更符合解剖,总体效果与后者相当,可能是更合理的手术方法,亦可进行广泛推广。由于本次研究样本容量有限,因而关于采取两种治疗方法所产生的远期影响仍需今后大样本随机进一步观察。endprint
参考文献
[1] Capece M,Imbimbo C.The varicocele:the proper therapy for the proper patient[J].Urologia,2014,81(3):165-168.
[2] Redmon J B,Carey P,Pryor J L.Varicocele-the most common cause of male factor infertility[J].Human Reproduction Update,2002,8(1):53-58.
[3] Franco G,Misuraca L,Ciletti M,et al.Surgery of male infertility:an update[J].Sexologies,2014,17(8):S16-S17.
[4] Diegidio P,Jhaveri J K,Ghannam S,et al.Review of current varicocelectomy techniques and their outcomes[J].Bju International,2011,108(7):1157-1172.
[5] Ficarra V,Crestani A,Novara G,et al.Varicocele repair for infertility:what is the evidence[J].Current Opinion in Urology,2012,22(6):489-494.
[6] Cho K S,Seo J T.Effect of Varicocelectomy on Male Infertility[J].Korean Journal of Urology,2014,55(11):703-709.
[7] Wong J,Chan S,Pagala M,et al.Lymphatic sparing microscopic retroperitoneal varicocelectomy:a preliminary experience[J].Journal of Urology,2009,182(5):2460-2463.
[8] Marte A,Pintozzi L,Cavaiuolo S,et al.Single-incision laparoscopic surgery and conventional laparoscopic treatment of varicocele in adolescents:Comparison between two techniques[J].African Journal of Paediatric Surgery,2014,11(3):201-205.
[9] Bansal D,Riachy E,Jr D W,et al.Pediatric varicocelectomy:a comparative study of conventional laparoscopic and laparoendoscopic single-site approaches[J].Journal of Endourology,2014,28(5):513-516.
[10] Hopps C V,Lemer M L,Schlegel P N,et al.Intraoperative varicocele anatomy:a microscopic study of the inguinal versus subinguinal approach[J].Journal of Urology,2003,170(6):2366-2370.
[11] Borruto F A,Impellizzeri P,Antonuccio P,et al.Laparoscopic vs open varicocelectomy in children and adolescents:review of the recent literature and meta-analysis[J].Journal of Pediatric Surgery,2010,45(12):2464-2469.
[12] Ding H,Tian J,Du W,et al.Open non-microsurgical,laparoscopic or open microsurgical varicocelectomy for male infertility:a meta-analysis of randomized controlled trials[J].Bju Interhational,2012,110(10):1536-1542.
[13]黄多斌,冼杰,王君勇,等.显微术式与腹膜后精索静脉高位结扎术式治疗精索静脉曲张的效果对比[J].中国当代医药,2017,24(7):85-87.
[14]邓广鹏.腹股沟外环下显微镜结扎手术治疗腹腔镜精索静脉高位结扎术后精索静脉曲张复发的临床效果[J].中国当代医药,2015,22(5):42-43.
[15]武小强,闫天中,张祥生,等.经外环口下精索静脉曲张结扎术疗效分析[J].河南医学高等专科学校学报,2014,26(4):386-387.
[16] Ozturk U,Ozdemir E,Buyukkagnici U,et al.Effect of spermatic vein ligation on seminal total antioxidant capacity in terms of varicocele grading[J].Andrologia,2012,44(Suppl 1):199-204.
[17] Najari B B,Li P S,Ramasamy R,et al.Microsurgical rat varicocele model[J].Journal of Urology,2014,191(2):548-553.
[18] Aldemir M,I??k E,Ozgün G,et al.Comparison of spermatic vein histology in patients with and without varicocele[J].Andrologia,2011,43(5):341-345.
[19] Mohseni M J,Nazari H,Amini E,et al.Shunt-type and stop-type varicocele in adolescents:prognostic value of these two different hemodynamic patterns[J].Fertility & Sterility,2011,96(5):1091-1096.
[20] Wong Y S,Chung K L,Lo K W,et al.Scrotal antegradesclerotherapy demonstrates anatomical variations on venous drainage in paediatric, adolescent and young adult varicoceles[J].Pediatric Surgery International,2014,30(1):107-111.
(收稿日期:2017-08-28) (本文編辑:张爽)endprint