不同频率肺复张术在单肺通气患者中应用效果的对比研究
戴 方,唐 斌
·论著·
不同频率肺复张术在单肺通气患者中应用效果的对比研究
戴 方1,唐 斌2
目的比较不同频率肺复张术(RM)在单肺通气(OLV)患者中的应用效果。方法选取2014年8月—2015年8月鄂东医疗集团市中医医院收治的拟行开胸手术及OLV的患者88例,根据RM频率分为A、B、C、D组,每组22例。OLV期间,A、B、C组患者RM频率分别为30 min/次、60 min/次、120 min/次,D组患者仅在关胸前行1次RM。比较4组患者手术相关指标(包括OLV时间、手术时间、补液量、失血量),OLV开始时(T1)、OLV 30 min(T2)、OLV 1 h(T3)、OLV 2 h(T4)、OLV结束时(T5)、恢复双肺通气30 min(T6)氧合指数(OI)和肺内分流量(Qsp),T1、T3、T6、术后2 h(T7)、术后24 h(T8)血清肿瘤坏死因子α(TNF-α)和白介素6(IL-6)水平。结果(1)4组患者OLV时间、补液量、失血量比较,差异无统计学意义(P>0.05);B组患者手术时间短于A、C、D组(P<0.05)。(2)时间与方法在OI和Qsp上存在交互作用(P<0.05);时间在OI和Qsp上主效应显著(P<0.05);方法在OI和Qsp上主效应显著(P<0.05)。T2时,B、C、D组患者OI低于A组(P<0.05);T3时,B组患者OI高于A、C、D组,C、D组患者OI低于A组(P<0.05);T4时,B组患者OI高于A、C、D组,C、D组患者OI低于A组,D组患者OI低于C组(P<0.05);T5、T6时,B组患者OI高于A、C、D组,C组患者OI高于A、D组,D组患者OI低于A组(P<0.05)。T2时,B、C、D组患者Qsp高于A组(P<0.05);T3时,B、C、D组患者Qsp高于A组,B组患者Qsp低于C、D组(P<0.05);T4、T5时,B组患者Qsp低于A、C、D组,C、D组患者Qsp高于A组,D组患者Qsp高于C组(P<0.05);T6时,B组患者Qsp低于A、C、D组,C组患者Qsp低于A、D组,D组患者Qsp高于A组(P<0.05)。(3)时间与方法在血清TNF-α和IL-6水平上存在交互作用(P<0.05);时间在血清TNF-α和IL-6水平上主效应显著(P<0.05);方法在血清TNF-α和IL-6水平上主效应显著(P<0.05)。T3时,B、C、D组患者血清TNF-α水平低于A组,B组患者血清TNF-α水平高于C、D组(P<0.05);T6、T7、T8时,B、C、D组患者血清TNF-α水平低于A组,B组患者血清TNF-α水平低于C、D组,D组患者血清TNF-α水平高于C组(P<0.05)。T3时,B、C、D组患者血清IL-6水平低于A组,B组患者IL-6水平高于C、D组(P<0.05);T6、T7、T8时,B、C组患者血清IL-6水平低于A组,B组患者IL-6水平低于C、D组,D组患者血清IL-6水平高于C组(P<0.05)。结论OLV期间每60 min行1次RM可有效改善OLV患者肺氧合功能,降低Qsp并减轻炎性反应,应用效果较佳。
单肺通气;肺复张术;疗效比较研究
戴方,唐斌.不同频率肺复张术在单肺通气患者中应用效果的对比研究[J].实用心脑肺血管病杂志,2017,25(9):37-41.[www.syxnf.net]
DAI F,TANG B.Comparative study for application effect of different frequencies of recruitment maneuver on one-lung ventilation[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2017,25(9):37-41.
单肺通气(one lung ventilation,OLV)的主要目的是提供良好的手术视野,防止健侧肺污染,常见并发症为低氧血症。临床常采用机械通气技术预防和治疗低氧血症,但由于患者自身排痰能力差、肺部感染等易引发肺不张,进而导致肺动静脉分流率增加、氧合能力降低,严重者甚至威胁到患者的生命安全[1]。近年研究表明,肺复张术(recruitment maneuver,RM)可有效修复塌陷的肺泡,使其较快重新开放,进而改善患者呼吸力学及氧合能力[2],但RM的不合理使用可诱发炎性反应,加重肺损伤。既往研究显示,RM对肺功能的双重作用与其复张频率有关,但目前OLV期间最佳复张频率尚不能确定[3-4]。本研究旨在比较不同频率RM在OLV患者中的应用效果,现报道如下。
1 资料与方法
1.1 一般资料 选取2014年8月—2015年8月鄂东医疗集团市中医医院收治的行OLV的患者88例,均拟行开胸手术。纳入标准:(1)术前2周内未吸烟;(2)无内分泌系统疾病史;(3)用力肺活量(FVC)>80%,第1秒用力呼气容积与用力肺活量比值(FEV1/FVC)>70%;(4)无放化疗史。排除标准:(1)合并心、肝、肾等重要脏器疾病者;(2)合并慢性呼吸系统疾病者。根据RM频率将所有患者分为A、B、C、D组,每组22例。4组患者性别、年龄、体质量及FEV1/FVC比较,差异无统计学意义(P>0.05,见表1),具有可比性。本研究经鄂东医疗集团市中医医院医学伦理委员会审核批准,所有患者自愿参加本研究并签署知情同意书。
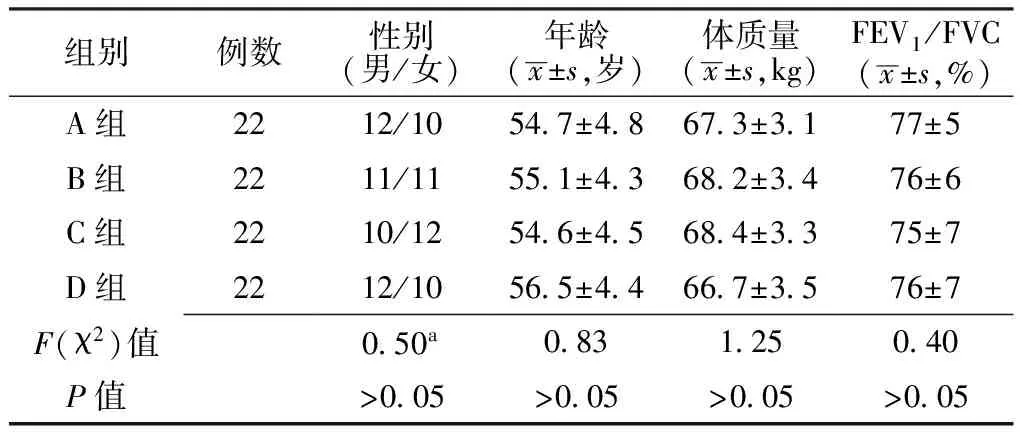
表1 4组患者一般资料比较
注:FEV1/FVC=第1秒用力呼气容积与用力肺活量比值;a为χ2值
1.2 治疗方法 各组患者均于进入手术室后给予乳酸钠林液(山东齐都药业有限公司生产,国药准字H20143278)10 ml/kg静脉滴注,采用MP50型多功能监测仪(德国Philips公司生产)监测患者心率、血氧饱和度(SpO2)及心电图(ECG)。依次给予异丙酚1.5 mg/kg、咪达唑仑0.04 mg/kg静脉注射麻醉患者,经口置入双腔支气管导管,依据双侧肺部听诊与纤维支气管镜定位后,连接德国德尔格Fabius Plus型麻醉机行机械通气,参数设置:氧流量为1.8 L/min,吸入氧浓度(FiO2)为100%,呼吸比为1.0∶1.5,潮气量(VT)为10 ml/kg,呼吸频率(RR)为10~12次/min;OLV开始,VT为5 ml/kg,RR为13~15次/min,呼气末正压(PEEP)为5 cm H2O(1 cm H2O=0.098 kPa),气道峰压(PAP)<34 cm H2O,其他参数不变。经右颈内静脉行中心静脉穿刺置管,麻醉维持:吸入2%七氟烷,静脉泵注异丙酚0.8 μg·kg-1·min-1,脑电双频指数(BIS)值维持45~55。其中A、B、C组患者RM频率分别为30 min/次、60 min/次、120 min/次,D组患者仅在关胸前行1次RM。RM具体方法:清理双肺支气管内分泌物后行双肺通气,麻醉机限压阀压力调为40 mm Hg(1 mm Hg=0.133 kPa),手控通气,持续挤压呼吸气囊,同时观察患者进气峰压数值,峰压上升到40 mm Hg时保持15 s,复张萎陷肺叶。
1.3 观察指标 (1)记录4组患者手术相关指标,包括OLV时间、手术时间、补液量及失血量。(2)分别于OLV开始时(T1)、OLV 30 min(T2)、OLV 1 h(T3)、OLV 2 h(T4)、OLV结束时(T5)、恢复双肺通气30 min(T6)采集4组患者桡动脉血1.5 ml行动脉血气分析,仪器为美国i-STAT型血气分析仪,计算氧合指数(OI)和肺内分流量(Qsp),其中OI=动脉血氧分压(PaO2)/FiO2、Qsp=〔肺泡-动脉氧分压差(PA-aDO2)×0.033 1〕/PA-aDO2×0.033 1+〔动脉血氧含量(CaO2)-混合静脉血氧含量(CvO2)〕 。(3)分别于T1、T3、T6、术后2 h(T7)及术后24 h(T8)采集4组患者静脉血5 ml置于10 ml离心管中,4 ℃环境下3 000/min离心10 min,置于-20 ℃环境下保存待测,采用酶联免疫吸附试验(ELISA)检测血清肿瘤坏死因子α(TNF-α)水平,仪器为TECAN SUNRISE全自动酶标仪;采用双抗夹心法检测血清白介素6(IL-6)水平,仪器为NEPHSTAR PLUS三通道特定蛋白分析仪,均严格按照试剂盒说明书进行操作。
2 结果
2.1 4组患者手术相关指标比较 4组患者OLV时间、补液量、失血量比较,差异无统计学意义(P>0.05);4组患者手术时间比较,差异有统计学意义(P<0.05),其中B组患者手术时间短于A、C、D组,差异有统计学意义(P<0.05,见表2)。

表2 4组患者手术相关指标比较
注:OLV=单肺通气;与B组比较,aP<0.05
2.2 4组患者不同时间点OI和Qsp比较 时间与方法在OI和Qsp上存在交互作用(P<0.05);时间在OI和Qsp上主效应显著(P<0.05);方法在OI和Qsp上主效应显著(P<0.05)。T2时,B、C、D组患者OI低于A组,差异有统计学意义(P<0.05);T3时,B组患者OI高于A、C、D组,C、D组患者OI低于A组,差异有统计学意义(P<0.05);T4时,B组患者OI高于A、C、D组,C、D组患者OI低于A组,D组患者OI低于C组,差异有统计学意义(P<0.05);T5、T6时,B组患者OI高于A、C、D组,C组患者OI高于A、D组,D组患者OI低于A组,差异有统计学意义(P<0.05)。T2时,B、C、D组患者Qsp高于A组,差异有统计学意义(P<0.05);T3时,B、C、D组患者Qsp高于A组,B组患者Qsp低于C、D组,差异有统计学意义(P<0.05);T4、T5时,B组患者Qsp低于A、C、D组,C、D组患者Qsp高于A组,D组患者Qsp高于C组,差异有统计学意义(P<0.05);T6时,B组患者Qsp低于A、C、D组,C组患者Qsp低于A、D组,D组患者Qsp高于A组,差异有统计学意义(P<0.05,见表3)。
2.3 4组患者不同时间点血清IL-6和TNF-α水平比较 时间与方法在血清TNF-α和IL-6水平上存在交互作用(P<0.05);时间在血清TNF-α和IL-6水平上主效应显著(P<0.05);方法在血清TNF-α和IL-6水平上主效应显著(P<0.05)。T3时,B、C、D 组患者血清TNF-α水平低于A组,B患者血清TNF-α水平高于C、D组,差异有统计学意义(P<0.05);T6、T7、T8时,B、C、D组患者血清TNF-α水平低于A组,B组患者血清TNF-α水平低于C、D组,D组患者血清TNF-α水平高于C组,差异有统计学意义(P<0.05)。T3时,B、C、D组患者血清IL-6水平低于A组,B组患者IL-6水平高于C、D组,差异有统计学意义(P<0.05);T6、T7、T8时,B、C组患者血清IL-6水平低于A组,B组患者IL-6水平低于C、D组,D组患者血清IL-6水平高于C组,差异有统计学意义(P<0.05,见表4)。
3 讨论
OLV可隔离正常肺,为手术创造较佳的操作视野,故其在开胸手术过程中应用广泛;但OLV会导致肺内分流、通气/血流比例失调等,进而影响肺氧合功能[5]。目前,在OLV过程中采取间断RM可以扩张萎陷肺泡,增加残气量及OI,进而缓解肺损伤。临床研究显示,开胸手术OLV过程中,RM能使塌陷的肺泡有效扩张,进而改善肺呼吸力学与氧合功能[6];但RM可诱发炎性反应,加重肺损伤,而RM对肺功能的双重作用与其频率有关[7]。

表3 4组患者不同时间点OI和Qsp比较
注:OI=氧合指数,Qsp=肺内分流量;1 mm Hg=0.133 kPa;与A组比较,aP<0.05;与B组比较,bP<0.05;与C组比较,cP<0.05
表4 4组患者不同时间点血清TNF-α和IL-6水平比较
注:TNF-α=肿瘤坏死因子α,IL-6=白介素6;与A组比较,aP<0.05;与B组比较,bP<0.05;与C组比较,cP<0.05
本研究结果显示,4组患者OLV时间、补液量、失血量间无差异,但B组患者手术时间短于A、C、D组,提示每60 min行1次RM可有效缩短OLV患者手术时间。临床研究显示,OLV期间Qsp增加、OI降低可启动缺氧性肺血管收缩机制,进而纠正通气/血流比例失调[8]。本研究结果显示,T2时,B、C、D组患者OI低于A组;T3时,B组患者OI高于A、C、D组,C、D组患者OI低于A组;T4时,B组患者OI高于A、C、D组,C、D组患者OI低于A组,D组患者OI低于C组;T5、T6时,B组患者OI高于A、C、D组,C组患者OI高于A、D组,D组患者OI低于A组;提示RM可改善OLV患者肺氧合功能,与其他复张频率相比,每60 min行1次RM可更有效地改善OLV患者肺氧合功能,分析其原因可能为OLV期间非通气侧肺泡萎陷处于缺氧状态,且伴有低氧肺血管收缩,不同频率RM可使萎陷肺泡复张,肺功能缓慢复张后肺细胞出现明显机械牵张,进而增加OI,但不同频率RM对肺氧合功能的影响不同[9-10]。此外,本研究结果还显示,T2时,B、C、D组患者Qsp高于A组;T3时,B、C、D组患者Qsp高于A组,B组患者Qsp低于C、D组;T4、T5时,B组患者Qsp低于A、C、D组,C、D组患者Qsp高于A组,D组患者Qsp高于C组;T6时,B组患者Qsp低于A、C、D组,C组患者Qsp低于A、D组,D组患者Qsp高于A组;提示RM可降低OLV患者Qsp,与其他复张频率相比,每60 min行1次RM可更有效地降低OLV患者Qsp。
既往研究显示,开胸手术OLV过程中机体可释放多种炎性细胞因子,进而导致全身炎症反应。TNF-α作为启动因子,是急性肺损伤发生过程中最早出现的炎性反应指标,其主要来源于激活的巨噬细胞,能反映细胞组织初期损伤情况[11]。IL-6是一种多功能促炎性细胞因子,血清IL-6水平升高可作为急性期炎性反应的判定依据,其与肺损伤程度有关[12]。TNF-α和IL-6均参与肺部非特异性炎性反应,且具有重要指示作用[13]。本研究结果显示,T3时,B、C、D 组患者血清TNF-α水平低于A组,B组患者血清TNF-α水平高于C、D组;T6、T7、T8时,B、C、D组患者血清TNF-α水平低于A组,B组患者血清TNF-α水平低于C、D组,D组患者血清TNF-α水平高于C组;T3时,B、C、D组患者血清IL-6水平低于A组,B组患者IL-6水平高于C、D组;T6、T7、T8时,B、C组患者血清IL-6水平低于A组,B组患者IL-6水平低于C、D组,D组患者血清IL-6水平高于C组;提示RM可导致炎性反应,与其他复张频率相比,每60 min行1次RM的OLV患者炎性反应轻微,分析其原因可能为RM在修复肺功能的同时还可导致应激反应,引起肺细胞释放炎性细胞因子,频繁行RM可诱使大量氧分子进入肺细胞而导致氧化应激增加,进一步加重炎性反应[14]。
综上所述,OLV过程中每60 min行1次RM可有效改善患者肺氧合能力,降低Qsp并减轻炎性反应,是较为合适的RM频率。
作者贡献: 戴方进行文章的构思与设计,结果分析与解释,撰写论文,负责文章的质量控制及审校,对文章整体负责,监督管理;唐斌进行研究的实施与可行性分析;戴方、唐斌进行数据收集、整理、分析。
本文无利益冲突。
[1]田珺,李岩,孟瑞霞,等.单肺通气术后肺部感染发生率及危险因素分析[J].中华医院感染学杂志,2014,24(8):1987-1989.DOI:10.11816/cn.ni.2014-135497.
[2]ZUO H,ZENG L,GUO G,et al.High-frequency oscillatory ventilation combined with partial liquid ventilation in experimental lung injury:effects on lung cell apoptosis[J].Wien Klin Wochenschr,2015,127(15):606-611.
[3]刘敏肖,刘立永,于海龙,等.胸科手术单肺通气期间间断性肺复张对肺损伤的影响[J].重庆医学,2014,43(15):1878-1880,1883.DOI:10.3969/j.issn.1671-8348.2014.15.019.
[4]陈敏,金良凤.两种不同肺复张策略在急性呼吸窘迫综合征治疗中的应用效果比较[J].武汉大学学报(医学版),2014,35(6):903-906.
[5]张援,廖婧华.不同单肺通气方式在全腔镜食管癌根治术中的应用[J].福建医科大学学报,2015,57(5):313-316.
[6]王琼娅,马雁,李莞婷,等.仰卧位或俯卧位肺复张治疗老年重症肺炎患者的疗效比较[J].中国老年学杂志,2015,35(23):6804-6806.DOI:10.3969/j.issn.1005-9202.2015.23.070.
[7]何明枫,陈宇.允许性高碳酸血症对单肺通气后肺功能及萎陷侧肺炎症反应的影响[J].临床麻醉学杂志,2015,31(12):1172-1175.
[8]徐悦利,李汝泓,李玲,等.肺保护性通气策略联合反复肺复张在食管癌切除术中的应用[J].山东医药,2016,56(38):47-49.DOI:10.3969/j.issn.1002-266X.2016.38.016.
[9]房晓薇,吴利东.压力控制法肺复张预防老年患者腹部术后肺部并发症的作用[J].中国老年学杂志,2015,35(6):1552-1553.DOI:10.3969/j.issn.1005-9202.2015.06.055.
[10]ACHAR S K,CHAUDHURI S,KRISHNA H,et al.Re-expansion pulmonary oedema-differential lung ventilation comes to the rescue[J].Indian J Anaesth,2014,58(3):330-333.DOI:10.4103/0019-5049.135051.
[11]邓友明,殷国平,张维峰,等.小潮气量快频率间歇正压通气在患儿胸腔镜手术中的应用[J].临床麻醉学杂志,2016,32(1):86-88.
[12]刘娜,徐悦利,路艳,等.不同补液方案对开胸手术单肺通气患者血管外肺水的影响[J].重庆医学,2016,45(24):3381-3384.DOI:10.3969/j.issn.1671-8348.2016.24.023.
[13]洪庆雄,张文璇,钟敏,等.腹腔镜手术中不同通气模式对肺功能的影响[J].临床麻醉学杂志,2015,31(7):658-660.
[14]刘晶,廖信芳,黄伟坚,等.胸腔镜辅助下婴儿先天性肺囊腺瘤围术期的呼吸管理[J].广东医学,2015,53(2):249-251.
ComparativeStudyforApplicationEffectofDifferentFrequenciesofRecruitmentManeuveronOne-lungVentilation
DAIFang1,TANGBin2
1.MunicipalTraditionalChineseMedicineHospitalofEdongMedicalGroup,Huangshi435000,China2.MaternalandChildCareServiceCenterofHuangshi,EdongMedicalGroup,Huangshi435000,China
TANGBin,E-mail:3074308987@qq.com
ObjectiveTo compare the application effect of different frequencies of recruitment maneuver on one-lung ventilation(OLV).MethodsA total of 88 patients prepared for thoracotomy and OLV were selected in the Municipal Traditional Chinese Medicine Hospital of Edong Medical Group from August 2014 to August 2015,and they were divided into A group(
recruitment maneuver with interval of 30 minutes per time),B group(received recruitment maneuver with interval of 60 minutes per time),C group(received recruitment maneuver with interval of 120 minutes per time)and D group(received recruitment before closing thoracic cavity only)according to the recruitment maneuver frequency during OLV,each of 22 cases.Surgical indicators(including duration of OLV,duration of surgery,volume of fluid input and blood loss volume),oxygenation index(OI)and intrapulmonary shunt volume(Qsp)at the begin of OLV(T1),after 30 minutes of OLV(T2),after 1 hours of OLV(T3),after 2 hours of OLV(T4),at the end of OLV(T5)and after 30 minutes of restoring dual lung ventilation(T6),serum levels of TNF-α and IL-6 at T1,T3 and T6,after 2 hours of surgery(T7),after 24 hours of surgery(T8).Results(1)No statistically significant differences of duration of OLV,volume of fluid input or blood loss volume was found among the four groups(P>0.05),while duration of surgery of B group was statistically significantly shorter than that of A group,C group and D group,respectively(P<0.05).(2)There was interaction in OI and Qsp between time and method(P<0.05);main effects of time and method were significant in OI and Qsp(P<0.05).At T2,OI of B group,C group and D group was statistically significantly lower than that of A group,respectively(P<0.05);at T3,OI of B group was statistically significantly higher than that of A group,C group and D group,respectively,meanwhile OI of C group and D group was statistically significantly lower than that of A group,respectively(P<0.05);at T4,OI of B group was statistically significantly higher than that of A group,C group and C group,respectively,meanwhile OI of C group and D group was statistically significantly lower than that of A group,respectively,OI of D group was statistically significantly lower than that of C group(P<0.05);at T5 and T6,OI of B group was statistically significantly higher than that of A group,C group and D group,respectively,meanwhile OI of C group was statistically significantly higher than that of A group and D group,OI of D group was statistically significantly lower than that of A group(P<0.05).At T2,Qsp of B group,C group and D group was statistically significantly higher than that of A group,respectively(P<0.05);at T3,Qsp of B group,C group and D group was statistically significantly higher than that of A group,respectively,meanwhile Qsp of B group was statistically significantly lower than that of C group and D group,respectively(P<0.05);at T4 and T5,Qsp of B group was statistically significantly lower than that of A group,C group and D group,respectively,meanwhile Qsp of C group and D group was statistically significantly higher than that of A group,respectively,Qsp of D group was statistically significantly higher than that of C group(P<0.05);at T6,Qsp of B group was statistically significantly lower than that of A group,C group and D group,respectively,Qsp of C group was statistically significantly lower than that of A group and D group,respectively,Qsp of D group was statistically significantly higher than that of A group(P<0.05).(3)There was interaction in serum levels of TNF-α and IL-6 between time and method(P<0.05);main effects of time and method were significant in serum levels of TNF-α and IL-6(P<0.05).At T3,serum TNF-α level of B group,C group and D group was statistically significantly lower than that of A group,respectively,meanwhile serum TNF-α level of B group was statistically significantly higher than that of C,D group(P<0.05);at T6,T7 and T8,serum TNF-α level of B group,C group and D group was statistically significantly lower than that of A group,respectively,meanwhile serum TNF-α level of B group was statistically significantly lower than that of C,D group,respectively,serum TNF-α level of D group was statistically significantly higher than that of C group(P<0.05).At T3,serum IL-6 level of B group,C group and D group was statistically significantly lower than that of A group,respectively,meanwhile serum IL-6 level of B group was statistically significantly higher than that of C,D group,respectively(P<0.05);at T6,T7 and T8,serum IL-6 level of B group and C group was statistically significantly lower than that of A group,respectively,meanwhile serum IL-6 level of B group was statistically significantly lower than that of C group and D group,respectively,serum IL-6 level of D group was statistically significantly higher than that of C group(P<0.05).ConclusionRecruitment maneuver with interval of 60 minutes per time during OLV has better application effect in patients undergoing thoracotomy,can effectively improve the pulmonary oxygenation function,reduce the Qsp and relievethe inflammatory reaction.
One lung ventilation;Recruitment maneuver;Comparative effectiveness research
1.435000湖北省黄石市,鄂东医疗集团市中医医院
2.435000湖北省黄石市,鄂东医疗集团黄石市妇幼保健院
唐斌,E-mail:3074308987@qq.com
R 332
A
10.3969/j.issn.1008-5971.2017.09.009
2017-04-26;
2017-08-20)
(本文编辑:谢武英)

