氧化槐定碱通过Akt/Nrf2/HO-1和Akt/GSK3β信号通路对急性肾损伤的保护作用
王文文,张 敏
(1浙江大学医学院附属妇产科医院病理科,杭州 310006;2浙江中医药大学附属第一医院病理科;*通讯作者,E-mail:bzwangwenwen@126.com)
氧化槐定碱通过Akt/Nrf2/HO-1和Akt/GSK3β信号通路对急性肾损伤的保护作用
王文文1*,张 敏2
(1浙江大学医学院附属妇产科医院病理科,杭州 310006;2浙江中医药大学附属第一医院病理科;*通讯作者,E-mail:bzwangwenwen@126.com)
目的 探讨氧化槐定碱(oxysophoridine,OSR)对小鼠肾缺血再灌注(ischemia/reperfusion,I/R)诱导的急性肾损伤的保护作用及其机制。 方法 C57/BL6小鼠30只随机分为假手术组(sham组)、模型组(I/R组)和给药组(I/R+OSR组)。I/R+OSR组预给药5 d[250 mg/(kg·d),腹腔注射],sham组和I/R组给予相同体积的生理盐水。第5天给药后1 h开始利用左侧肾切除、右侧肾蒂缺血30 min再灌注24 h的方法构建缺血再灌注损伤模型。下腔静脉取血并离心取血清,用自动生化仪检测肌酐和尿素氮,试剂盒检测丙二醛的生成及超氧化物歧化酶(superoxide dismutase,SOD)和过氧化氢酶(catalase,CAT)的活性,ELISA法检测肿瘤坏死因子-α(TNF-α)和白细胞介素-1β(IL-1β),HE染色法检测肾脏组织形态学,Western blot 法检测蛋白激酶B(Akt)、磷酸化Akt(p-Akt)、细胞内核因子E2 相关因子2(Nrf2)、血红素加氧酶(HO-1)、糖原合酶激酶-3β(GSK3β)、磷酸化GSK3β(p-GSK3β)、半胱天冬酶-3(pro-caspase-3)、活化的半胱天冬酶-3(cleaved caspase-3)、B淋巴细胞瘤-2(Bcl-2)的表达。 结果 与sham组比较,I/R组小鼠肌酐、尿素氮、丙二醛、TNF-α和IL-1β显著升高(P<0.05),SOD、CAT的活性显著降低(P<0.05),p-Akt、Nrf2、HO-1、p-GSK3β、Bcl-2、pro-caspase-3蛋白表达显著降低(P<0.05),而促凋亡蛋白cleaved caspase-3表达显著升高(P<0.05)。与I/R组比较,OSR组小鼠肌酐、尿素氮、丙二醛、TNF-α和IL-1β显著降低(P<0.05),SOD、CAT的活性显著增加(P<0.05),p-Akt、Nrf2、HO-1、p-GSK3β、Bcl-2、pro-caspase-3蛋白表达显著升高(P<0.05),促凋亡蛋白cleaved caspase-3表达显著降低(P<0.05)。与sham组比较,HE染色结果显示I/R组肾损伤显著加重,而给药后可显著改善急性肾损伤。 结论 OSR通过Akt/Nrf2/HO-1和Akt/GSK3β信号通路及抗炎和抗凋亡相关信号通路机制对肾缺血再灌注诱导的急性肾损伤起到保护作用。
氧化槐定碱; 肾缺血再灌注; 细胞内核因子E2相关因子2; 血红素加氧酶; 糖原合酶激酶-3β
急性肾损伤(acute kidney injury,AKI)是一种以肾功能突然下降为特征的综合征[1, 2],它会导致体内肌酐、尿素氮和其他生化废物的蓄积及电解质和酸碱稳态和含氮废物保留的失衡[3, 4]。对于住院病人来说,AKI是一种常见的和严重的并发症[5, 6],有研究报道,普通住院患者中AKI的发病率约为5%,并且在世界范围内每年约200万人死于此疾病[7, 8]。关于AKI的机制研究报道已有很多,但是目前还没有很好的方法来预防或治疗AKI[9],AKI的信号分子机制目前尚不完全清楚,进一步探究AKI的病理生理机制是至关重要的。
肾缺血/再灌注(ischemia reperfusion,I/R)损伤是AKI的一种常见原因。肾缺血再灌注损伤机制复杂,目前文献报道的包括ATP缺失、细胞内Ca2+堆积、ROS、促炎细胞因子、细胞凋亡信号通路等导致的内皮功能障碍和肾小管细胞损伤[10, 11]。缺血再灌注产生的大量ROS,进而导致肾小管上皮细胞的损伤和凋亡,是造成肾损伤及病理反应的主要原因[12, 13]。氧化槐定碱(oxysophoridine,OSR)是从宁夏特色豆科槐属植物苦豆子中提取的主要生物碱之一,其化学结构式是由两个哌啶环组成。一些文献报道氧化槐定碱具有抗氧化应激、抗炎、抗凋亡和神经保护作用[14-17],然而在肾缺血再灌注损伤中的保护作用以及作用机制尚未有研究报道。本实验通过单侧肾缺血再灌注模型建立小鼠急性肾损伤模型,探讨氧化槐定碱对肾缺血再灌注损伤的保护作用及其机制。
1 材料和方法
1.1 实验动物
12周龄SPF级健康雄性C57BL/6小鼠,体质量25-28 g,由浙江大学动物中心提供(订购与上海斯莱克实验动物有限责任公司,动物合格证号:SCXK(沪)2007-0005)。
1.2 主要试剂
氧化槐定碱(OSR),北京寰宇科创生物科技发展有限公司提供, 纯度98%,使用时用0.9%的生理盐水配成所需浓度。丙二醛(MDA)检测试剂盒、总过氧化物歧化酶(SOD)活性检测试剂盒、过氧化氢酶(CAT)检测试剂盒和BCA蛋白定量试剂盒购买于上海碧云天生物技术有限公司;小鼠肿瘤坏死因子α(TNF-α)和白细胞介素1β (IL-1β)ELISA试剂盒购买于美国R&D公司。抗体 p-Akt、Akt、p-GSK3β、GSK3β购买于CST抗体公司;Nrf2、HO-1、Pro-caspase-3、Cleaved caspase-3、Bcl-2、β-actin,购买于abcam抗体公司。
1.3 分组及给药
为了研究OSR对肾脏缺血再灌注诱导的急性肾损伤的保护作用及相关机制,本实验设计如下:先将C57BL/6小鼠30只随机分为3组(每组10只): sham组、I/R组、OSR组(250 mg/kg[15-17],腹腔注射给药)。OSR组造模前预防性腹腔注射给药5 d,每天1次,缺血前1 h再给药1次。sham组和I/R组给予相同体积的生理盐水。用自动生化仪检测血清中肌酐和尿素氮的变化,用试剂盒检测丙二醛含量变化、SOD和CAT的酶活性变化。用ELISA试剂盒检测组织中TNF-α 和IL-1β表达变化。用Wes-tern blot 方法检测Akt/Nrf2/HO-1和Akt/GSK3β信号通路相关蛋白指标的变化。
1.4 肾缺血再灌注损伤模型的制备

1.5 检测肌酐、尿素氮、丙二醛、SOD、CAT、TNF-α和IL-1β
小鼠颈椎脱臼处死前,经由下腔静脉取血,室温静置1-2 h,然后于3 000 r/min、4 ℃条件下离心15 min,取上清即为血清。利用自动生化仪检测血清中的肌酐和尿素氮。按照丙二醛检测试剂盒说明书操作检测血清中丙二醛的含量。
将肾组织匀浆,用BCA试剂盒进行蛋白定量,取出一部分匀浆液分别用总SOD活性检测试剂盒和CAT活性检测试剂盒检测组织中SOD和CAT含量。再取出一部分匀浆液分别用小鼠TNF-α 和小鼠IL-1β ELISA试剂盒检测组织中TNF-α 和IL-1β表达变化,剩余的部分用Western blot 法检测相关蛋白的变化。
1.6 苏木精-伊红(Hematoxylin-Eosin,HE)染色
处死小鼠取出肾脏,用4%的多聚甲醛溶液固定,用石蜡包埋,切成4 μm的肾切片然后按照HE染色的流程进行染色,并在显微镜下观察肾脏切片的形态学变化。
1.7 蛋白提取定量和蛋白印迹分析(Western blot)

将提取定量的蛋白样本用十二烷基磺酸钠-聚丙烯酰胺凝胶电泳(SDS-PAGE)分析,根据蛋白分子量大小选择10%-13.5%的分离胶进行电泳[20, 21]。简单来说,取等量蛋白样品进行电泳,然后转移至PVDF膜上,用5%的脱脂牛奶封闭后,根据抗体说明书按不同的比例稀释一抗抗体并放于4 ℃摇床过夜孵育。洗膜后加入1 ∶5 000稀释的二抗,将条带放于室温摇床孵育60 min,最后ECL化学发光法曝光并观察结果。以β-actin和LaminB1分别作为胞浆蛋白和核蛋白的内参蛋白,通过计算目标蛋白与内参蛋白的灰度比值进行半定量分析统计。
1.8 统计学分析

2 结果
2.1 OSR对肾缺血再灌注损伤后肾功能指标的影响
与sham组比较,I/R组和I/R+OSR组小鼠血清中肌酐和尿素氮显著升高(P<0.01);与I/R组比较,I/R+OSR组可明显降低血清中肌酐和尿素氮的含量(P<0.05,见表1)。


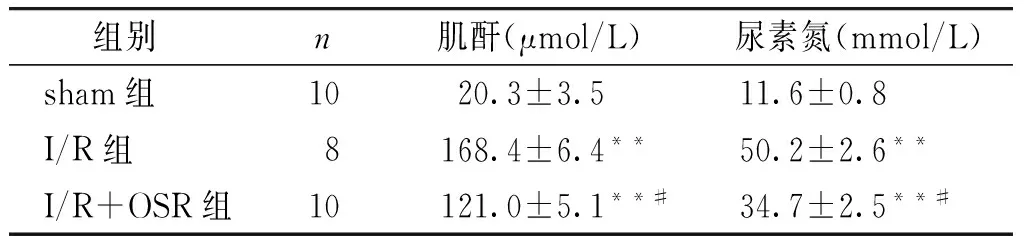
组别n肌酐(μmol/L)尿素氮(mmol/L)sham组10 20.3±3.5 11.6±0.8I/R组8 168.4±6.4** 50.2±2.6**I/R+OSR组10 121.0±5.1**# 34.7±2.5**#
与sham组比较,**P<0.01;与I/R组比较,#P<0.05
2.2 OSR对肾缺血再灌注损伤后脂质过氧化的影响
与sham组比较,I/R组小鼠血清中丙二醛含量显著增加(P<0.05);与I/R组比较,OSR组可明显减少丙二醛的增加(P<0.05,见图1)。
2.3 OSR对肾缺血再灌注损伤后SOD和CAT酶活性的影响
与sham组比较,I/R组肾组织中SOD和CAT显著降低(P<0.05);与I/R组比较,OSR组可部分逆转SOD和CAT的减少,并且有显著性差异(P<0.05,见图2)。
2.4 OSR对缺血再灌注后肾组织促炎性细胞因子表达的影响
ELISA结果表明,TNF-α和IL-1β蛋白的表达被OSR药物的干预所抑制,从而起到抗炎的作用。与sham组比较,I/R组小鼠肾组织中TNF-α 和IL-1β表达明显增加(P<0.05);与I/R组比较,OSR组可明显逆转TNF-α 和IL-1β表达的上调,且差异有统计学意义(P<0.05,见图3)。
2.5 OSR对I/R损伤后组织形态学的影响
sham组肾小管上皮细胞结构清晰,基底膜完整;I/R组在皮质区以及外髓质区出现不同程度的肾小管损伤,包括肾小管上皮细胞肿胀变性,出现核溶解、碎裂,细胞脱落,基底膜裸露或不完整以及较多的炎性细胞浸润;OSR可以明显减轻IR诱导的肾组织损伤(见图4)。

与sham组比较,*P<0.05;与I/R组比较,#P<0.05图2 肾缺血再灌注后SOD和CAT活性变化Figure 2 Changes of SOD and CAT activity after renal ischemia reperfusion and OSR treatment

与sham组比较,*P<0.05;与I/R组比较,#P<0.05图3 肾缺血再灌注后促炎因子TNF-α和IL-1β表达变化Figure 3 Changes of proinflammatory factor TNF-α and IL-1β expression in mice after renal ischemia reperfusion and OSR treatment

图4 小鼠肾缺血再灌注后肾脏组织形态学变化 (HE染色,×200)Figure 4 The morphological changes of renal tissue in mice after renal ischemia reperfusion (HE,×200)
2.6 OSR对I/R损伤后Akt/Nrf2/HO-1和Akt/GSK3β通路蛋白表达的影响
与sham组相比,肾缺血再灌注损伤显著降低了胞浆内p-Akt (见图5A和B)、 HO-1 (见图5E和F)、p-GSK3β (见图5G和H)以及核内Nrf-2 (见图5C和D)的表达。预给药OSR后可以部分逆转p-Akt、HO-1、p-GSK3β及Nrf2蛋白的下调。
2.7 OSR对肾缺血再灌注损伤后凋亡相关蛋白信号通路的影响
研究结果显示,与sham组比较,I/R损伤后Pro-caspase-3和Bcl-2明显下调,cleaved caspase-3明显上调,进而诱发了肾组织细胞凋亡。OSR可以明显降低cleaved caspase-3的激活,改善Pro-caspase-3和Bcl-2的下调(见图6),从而起到保护缺血再灌注诱导的急性肾损伤的作用。

左边一列为各蛋白的Western blot检测结果;右边一列为相应的蛋白Western blot结果的统计分析;与sham组比较,*P<0.05;与I/R组比较,#P<0.05图5 肾缺血再灌注后Akt/Nrf2/HO-1和Akt/GSK3β信号通路相关蛋白质表达变化Figure 5 Changes of protein expression of Akt/Nrf2/HO-1 and Akt/GSK3β signaling pathways after renal ischemia reperfusion

与sham组比较,*P<0.05;与I/R组比较,#P<0.05图6 肾缺血再灌注后凋亡相关蛋白质表达变化Figure 6 Changes of protein expression of apoptosis-related proteins after renal ischemia reperfusion
3 讨论
AKI疾病对病人有很高的致死率[22]。AKI的主要病因包括肾缺血、缺氧或肾毒性等[23, 24]。I/R损伤是AKI的一种常见原因。I/R损伤会引起肾脏ROS的过多生成和内源性抗氧化物的减少[25]。I/R损伤的病理生理机制包括内皮细胞功能障碍、ROS过多产生、促炎症细胞因子的释放、凋亡信号通路的激活等[26-28]。AKI的发病机制至今仍未被完全阐明,但是很多研究证明,减轻氧化应激、凋亡和炎性反应,对I/R损伤有着重要保护作用。有研究表明可以通过Nrf2/ARE/HO-1信号通路的激活,进而抵抗氧化应激,减少I/R损伤导致的肾小管凋亡,起到保护肾脏的作用[12, 29];也可以经由抗炎作用和抗凋亡信号通路起到保护肾脏的作用[29-31]。
本研究结果显示,I/R损伤后肾功能指标肌酐和尿素氮水平显著升高,而与IR组比较,OSR药物组可以明显改善肾脏功能指标。I/R损伤后肾组织SOD、CAT酶活性减弱,表明肾脏自身的自由基清除能力下降,从而导致氧化应激激活,氧化应激激活后一方面可以诱导脂质过氧化导致丙二醛在体内蓄积,另一方面也会诱导凋亡信号通路的激活,从而导致肾损伤。OSR给药明显改善了酶活性,减弱了氧化应激的激活,减轻了肾组织损伤。肾脏I/R损伤后促炎因子TNF-α和IL-β也大量释放,过多的炎症因子的释放也会诱发肾损伤,而OSR组可以减少促炎症因子的释放,改善肾损伤。HE染色形态学显示,I/R损伤后肾组织的小管损伤坏死增加,而OSR预给药减轻了肾小管的损伤和坏死。
细胞保护自身抵抗伤害性刺激的内源性防御机制对于细胞的存活尤为重要。显而易见, Keap1/Nrf2/HO-1信号通路在氧化应激的病理生理反应中是一个关键的调控因子,已经成为细胞抗氧化应激的主要防御机制[27, 32]。PI3K/Akt信号通路在调节细胞生长和存活中起着重要的作用,并且Akt的激活可以减轻I/R诱导的急性肾损伤[33, 34]。PI3K/Akt信号通路也可以调节Nrf2的活性,Akt的磷酸化可以增强下游Nrf2的活性,从而促进细胞的内源性抗氧化作用[35]。给药后Akt,p-Akt,Nrf2 和HO-1的蛋白表达证明OSR可以通过Akt/Nrf2/HO-1信号通路起到保护肾脏的作用。Akt通过抑制凋亡而促进细胞存活是经由磷酸化和失活它的一些靶标,其中包括GSK3β[36]。本研究结果显示I/R损伤后Akt的磷酸化下调,导致下游GSK3β磷酸化也下调,而OSR给药后可以逆转这种下调,表明OSR可以通过Akt/GSK3β信号通路起到保护肾脏的作用。
Pro-caspase-3的激活形式cleaved caspase-3是一种重要的促凋亡蛋白。Bcl-2家族蛋白通过诱导凋亡或抗凋亡调控着细胞的命运,Bcl-2被认为是一个重要的抗凋亡蛋白。研究结果显示I/R损伤后Bcl-2下调,cleaved caspase-3上调,凋亡增加,而OSR给药后可以下调cleaved caspase-3,上调Bcl-2,从而起到保护肾脏的作用。
总之,本研究初步证明药物OSR通过抗氧化应激、抗炎和抗凋亡起到保护肾脏的作用,其作用机制是通过Akt/Nrf2/HO-1和Akt/GSK3β信号通路起到改善肾功能的作用。生物体内抗氧化系统是一个复杂的分子网络,涉及到的信号通路不止有Akt/Nrf2/HO-1和Akt/GSK3β信号通路;Nrf2的上游调控分子也不止Akt一个,也有其他的上游调控蛋白如ERK1/2和MAPK等;PI3K/Akt通路下游亦不止这些,是否还有其他的分子参与OSR对急性肾损伤的保护作用有待进一步研究。目前临床上获批的能治疗AKI的药物几乎没有[10],本研究证实OSR对急性肾损伤有保护作用,或许OSR可以作为潜在治疗AKI的药物,这对治疗AKI药物的基础研发和临床研究都有着很好的指导意义。
[1] Abuelo JG. Normotensive ischemic acute renal failure[J]. N Engl J Med, 2007, 357(8):797-805.
[2] Hropot M, Juretschke HP, Langer KH,etal. S3226, a novel NHE3 inhibitor, attenuates ischemia-induced acute renal failure in rats[J]. Kidney Int, 2001,60(6):2283-2289.
[3] Bauerle JD, Grenz A, Kim JH,etal. Adenosine generation and signaling during acute kidney injury[J]. J Am Soc Nephrol, 2011, 22(1):14-20.
[4] Bellomo R, Kellum JA, Ronco C. Acute kidney injury[J]. Lancet, 2012, 380(9843):756-766.
[5] Stafford-Smith M, Li YJ, Mathew JP,etal. Genome-wide association study of acute kidney injury after coronary bypass graft surgery identifies susceptibility loci[J]. Kidney Int, 2015, 88(4):823-832.
[6] Kelly KJ, Molitoris BA. Acute renal failure in the new millennium: time to consider combination therapy[J]. Semin Nephrol, 2000, 20(1):4-19.
[7] Murugan R, Kellum JA. Acute kidney injury: what's the prognosis?[J]. Nat Rev Nephrol, 2011, 7(4):209-217.
[8] Uchino S, Bellomo R, Goldsmith D,etal. An assessment of the RIFLE criteria for acute renal failure in hospitalized patients[J]. Crit Care Med, 2006, 34(7):1913-1937.
[9] Jo SK, Rosner MH, Okusa MD. Pharmacologic treatment of acute kidney injury: why drugs haven't worked and what is on the horizon[J]. Clin J Am Soc Nephrol, 2007, 2(2):356-365.
[10] Bonventre JV, Zuk A. Ischemic acute renal failure: an inflammatory disease?[J]. Kidney Int, 2004, 66 (2):480-485.
[11] Wu D, Chen X, Ding R, Qiao X,etal. Ischemia/reperfusion induce renal tubule apoptosis by inositol 1,4,5-trisphosphate receptor and L-type Ca2+channel opening[J]. Am J Nephrol, 2008, 28(3):487-499.
[12] Nie H, Xue X, Liu G,etal. Nitro-oleic acid ameliorates oxygen and glucose deprivation/re-oxygenation triggered oxidative stress in renal tubular cells via activation of Nrf2 and suppression of NADPH oxidase[J]. Free Radic Res, 2016, 50(11):1200-1213.
[13] Zhang L, Zhu Z, Liu J,etal. Protective effect of N-acetylcysteine (NAC) on renal ischemia/reperfusion injury through Nrf2 signaling pathway[J]. J Recept Signal Transduct Res, 2014, 34(5):396-400.
[14] Wang TF, Lei Z, Li YX,etal. Oxysophoridine protects against focal cerebral ischemic injury by inhibiting oxidative stress and apoptosis in mice[J]. Neurochem Res, 2013, 38(11):2408-2417.
[15] Wang YS, Li YX, Zhao P,etal. Anti-inflammation effects of oxysophoridine on cerebral ischemia-reperfusion injury in mice[J]. Inflammation, 2015, 38(6):2259-2268.
[16] Rui C, Yuxiang L, Ning J,etal. Anti-apoptotic and neuroprotective effects of oxysophoridine on cerebral ischemia both in vivo and in vitro[J]. Planta Med, 2013, 79(11):916-923.
[17] Meng C, Liu C, Liu Y,etal. Oxysophoridine attenuates the injury caused by acute myocardial infarction in rats through anti-oxidative, anti-inflammatory and anti-apoptotic pathways[J]. Mol Med Rep, 2015, 11(1):527-532.
[18] Han F, Chen YX, Lu YM,etal. Regulation of the ischemia-induced autophagy-lysosome processes by nitrosative stress in endothelial cells[J]. J Pineal Res, 2011, 51(1):124-135.
[19] Tao RR, Huang JY, Shao XJ,etal. Ischemic injury promotes keap1 nitration and disturbance of antioxidative responses in endothelial cells: a potential vasoprotective effect of melatonin[J]. J Pineal Res, 2013, 54(3):271-281.
[20] Zhang GS, Tian Y, Huang JY,etal. The gamma-secretase blocker DAPT reduces the permeability of the blood-brain barrier by decreasing the ubiquitination and degradation of occludin during permanent brain ischemia[J]. CNS Neurosci Ther, 2013, 19(1):53-60.
[21] Zhang GS, Ye WF, Tao RR,etal. Expression profiling of Ca(2+)/calmodulin-dependent signaling molecules in the rat dorsal and ventral hippocampus after acute lead exposure[J]. Exp Toxicol Pathol, 2012, 64(6):619-624.
[22] Rewa O, Bagshaw SM. Acute kidney injury-epidemiology, outcomes and economics[J]. Nat Rev Nephrol,2014,10(4):193-207.
[23] Basile DP, Anderson MD, Sutton TA. Pathophysiology of acute kidney injury[J]. Compr Physiol, 2012, 2(2):1303-1353.
[24] Arakelyan K, Cantow K, Hentschel J,etal. Early effects of an x-ray contrast medium on renal T(2) */T(2) MRI as compared to short-term hyperoxia, hypoxia and aortic occlusion in rats[J]. Acta physiol (Oxf), 2013, 208(2):202-213.
[25] Palipoch S. A review of oxidative stress in acute kidney injury: protective role of medicinal plants-derived antioxidants[J]. Afr J Tradit Complement Altern Med, 2013, 10(4):88-93.
[26] Munshi R, Hsu C, Himmelfarb J. Advances in understanding ischemic acute kidney injury[J]. BMC Med, 2011, 9:11.
[27] Zhang G, Wang Q, Zhou Q,etal. Protective effect of tempol on acute kidney injury through PI3K/Akt/Nrf2 signaling pathway[J]. Kidney Blood Press Res, 2016, 41(2):129-138.
[28] Wei J, Song J, Jiang S,etal. Role of intratubular pressure during the ischemic phase in acute kidney injury[J]. Am J Physiol Renal Physiol, 2017, 312(6):F1158-F1165.
[29] Zhao L, Xu L, Tao X,etal. Protective effect of the total flavonoids from Rosa laevigata Michx fruit on renal ischemia-reperfusion injury through suppression of oxidative stress and inflammation[J]. Molecules, 2016, 21(7):952.
[30] Gao S, Zhu Y, Li H,etal. Remote ischemic postconditioning protects against renal ischemia/reperfusion injury by activation of T-LAK-cell-originated protein kinase (TOPK)/PTEN/Akt signaling pathway mediated anti-oxidation and anti-inflammation[J]. Int Immunopharmacol, 2016, 38:395-401.
[31] Liu FH, Ni WJ, Wang GK,etal. Protective role of curcumin on renal ischemia reperfusion injury via attenuating the inflammatory mediators and Caspase-3[J].Cell Mol Biol,2016,62(11):95-99.
[32] Shih AY, Johnson DA, Wong G,etal. Coordinate regulation of glutathione biosynthesis and release by Nrf2-expressing glia potently protects neurons from oxidative stress[J]. J Neurosci, 2003, 23(8): 3394-3406.
[33] Gu J, Sun P, Zhao H,etal. Dexmedetomidine provides renoprotection against ischemia-reperfusion injury in mice[J]. Crit Care, 2011, 15(3):R153.
[34] Satake A, Takaoka M, Nishikawa M,etal. Protective effect of 17beta-estradiol on ischemic acute renal failure through the PI3K/Akt/eNOS pathway[J]. Kidney Int, 2008, 73(3):308-317.
[35] Nakaso K, Yano H, Fukuhara Y,etal. PI3K is a key molecule in the Nrf2-mediated regulation of antioxidative proteins by hemin in human neuroblastoma cells[J]. FEBS Lett, 2003, 546(2-3):181-184.
[36] Wang L, Zhu Y, Wang L,etal. Effects of chronic alcohol exposure on ischemia-reperfusion-induced acute kidney injury in mice: the role of β-arrestin 2 and glycogen synthase kinase 3[J]. Exp Mol Med, 2017, 49(6):e347.
ProtectiveeffectofoxysophoridinefromacutekidneyinjurybyAkt/Nrf2/HO-1andAkt/GSK3βsignalingpathways
WANG Wenwen1*,ZHANG Min2
(1DepartmentofPathology,Women’sHospital,SchoolofMedicine,ZhejiangUniversity,Hangzhou310006,China;2DepartmentofPathology,FirstAffiliatedHospitalofZhejiangChineseMedicalUniversity;*Correspondingauthor,E-mail:bzwangwenwen@126.com)
ObjectiveTo investigate the protective effects of oxysophoridine(OSR) from renal ischemia reperfusion-induced acute kidney injury in mice and its possible mechanism.MethodsC57/BL6 mice were randomly divided into 3 groups: sham-operated group(sham group), model group(I/R group), OSR group(I/R+OSR). The mice in OSR group were pretreated with OSR for 5 d before inducing the I/R injury model(250 mg/kg, once a day, intraperitoneal injection). The mice in sham group and I/R group were given the same volume of physiological saline. One hour after the last administration, the right renal pedicle was clamped for 30 min and left nephrectomy was performed to produce I/R injury model in mice. Blood samples were collected from the inferior vena cava and centrifuged. Serum creatinine and blood urea nitrogen were measured by an automatic biochemical analyzer. Malondialdehyde concentration and enzymatic activity of superoxide dismutase(SOD) and catalase(CAT) were measured by Kits respectively. Tumor necrosis factor alpha(TNF-α) and interleukin-1 beta(IL-1β) were detected by ELISA Kits. The histological structure changes of renal tissues were observed under microscope. The expression levels of protein kinase B(Akt), phosphorylated Akt(p-Akt), nuclear factor erythroid 2-related factor 2(Nrf2), heme oxygenase(HO-1), glycogen synthase kinase 3 beta(GSK3β), phosphorylation GSK3β(p-GSK3β), pro-caspase-3, cleaved caspase-3, B-cell lymphoma-2(Bcl-2) were detected by Western blot.ResultsCompared with sham group, serum creatinine, blood urea nitrogen, malondialdehyde, TNF-α and IL-1β increased significantly in I/R group(P<0.05), SOD and CAT decreased significantly in I/R group(P<0.05), and the expression of p-Akt, Nrf2, HO-1, p-GSK3β, Bcl-2, pro-caspase-3 reduced and cleaved caspase-3 increased significantly in I/R group(P<0.05). Compared with model group, serum creatinine, blood urea nitrogen, malondialdehyde, TNF-α and IL-1β decreased significantly in OSR group(P<0.05), SOD and CAT increased significantly in OSR group(P<0.05), and the expression of p-Akt, Nrf2, HO-1, p-GSK3β, Bcl-2, pro-caspase-3 increased and cleaved caspase-3 decreased significantly in OSR group(P<0.05). Compared with sham group, HE staining results showed severe kidney injury in I/R group, but the kidney damage was improved in OSR group.ConclusionOSR has the protective effect from the renal ischemia-reperfusion injury in mice and may be involved in anti-oxidative stress, anti-inflammation, and anti-apoptosis.
oxysophoridine; renal ischemia reperfusion; Nrf2; heme oxygenase(HO); glycogen synthase kinase 3 beta
R363,R692
A
1007-6611(2017)10-0992-07
10.13753/j.issn.1007-6611.2017.10.004
王文文,女, 1986-10生,硕士,住院医师,E-mail:bzwangwenwen@126.com
2017-06-09

