POSSUM、P-POSSUM和Cr-POSSUM及E-PASS评分系统对结直肠癌患者术后死亡风险的预测价值
刘婷婷,张 骜,胡 芳
·论著·
·专题研究·
POSSUM、P-POSSUM和Cr-POSSUM及E-PASS评分系统对结直肠癌患者术后死亡风险的预测价值
刘婷婷,张 骜,胡 芳*
目的探讨POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统对结直肠癌患者术后死亡风险的预测价值。方法回顾性分析2010—2015年天津医科大学总医院收治的550例结直肠癌患者的临床资料。按照POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统及研究需要,收集相关指标,并分别使用POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统预测结直肠癌患者术后30 d病死率。应用受试者工作特征(ROC)曲线和实际发生率/预测发生率(O/E)评价各评分系统对术后病死率的预测价值。结果POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统预测结直肠癌患者术后死亡的最佳截断值分别为54.29%、55.39%、31.68%、56.31%,灵敏度分别为83.3%、83.3%、33.3%、83.3%,特异度分别为29.0%、27.9%、1.6%、27.0%,ROC曲线下面积分别为0.733〔95%CI(0.500,0.966)〕、0.713〔95%CI(0.479,0.948)〕、0.751〔95%CI(0.570,0.932)〕、0.781〔95%CI(0.607,0.955)〕,O/E分别为0.128、0.414、0.248、0.712。结论POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统均存在高估结直肠癌患者术后病死率的情况,E-PASS评分系统预测结直肠癌患者术后病死率与实际病死率一致性较好。
结直肠肿瘤;死亡率;预测
刘婷婷,张骜,胡芳.POSSUM、P-POSSUM和Cr-POSSUM及E-PASS评分系统对结直肠癌患者术后死亡风险的预测价值[J].中国全科医学,2017,20(27):3368-3371.[www.chinagp.net]
LIU T T,ZHANG A,HU F.Value of POSSUM,P-POSSUM,Cr-POSSUM and E-PASS scoring system in predicting postoperative mortality department of general surgery risk of colorectal cancer patients[J].Chinese General Practice,2017,20(27):3368-3371.
结直肠癌是常见的消化道恶性肿瘤之一,目前手术治疗仍是其主要治疗手段。手术带来的应激反应极大地超过了患者本身的储备能力,从而导致其呼吸、血液循环、代谢、免疫系统功能紊乱,引发很多并发症,甚至出现死亡。如何于患者术前有效预测手术风险并给予干预,减少术后并发症、降低病死率,是外科医生临床决策的重要内容[1]。国外相继推出许多评估患者术后病死率和并发症发生率的预测系统,包含Physiological and Operative Severity Score for Enumeration of Mortality and morbidity(POSSUM)[2]及其改良版本Portsmouth(P-POSSUM)[3]和Colorectal POSSUM(Cr-POSSUM)[4]评分系统。HAGA等[5]提出的Estimation of physiologic ability and surgical stress(E-PASS)评分系统在其后续报道中应用于包括结直肠癌手术的各种外科手术,显示了良好的预测患者术后死亡风险的能力[6]。本研究将以上4种评分系统对国内结直肠癌患者术后死亡风险的预测价值进行比较,现报道如下。
1 资料与方法
1.1 数据收集 于天津医科大学总医院病案室查阅2010—2015年收入的结直肠癌患者住院病历,纳入标准:结肠癌或直肠癌患者〔按照国际疾病分类(ICD-10)(结肠癌ICD-10C18,直肠癌ICD-10C20)〕[7],行手术治疗,且术后病理证实为结肠癌或直肠癌;有POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统所需完整资料。排除标准:病历资料不完整。研究的死亡病例为结直肠癌术后30 d内死亡的患者,术前情况选择离手术日期最近的资料。本研究共纳入550例患者,其中有6例于术后30 d内死亡。
1.2 研究方法 按照POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统及研究需要,收集相关指标。
根据POSSUM、P-POSSUM、Cr-POSSUM评分系统,收集生理学评分指标和手术侵袭度评分指标:(1)术前情况:年龄、心功能、肺功能、收缩压、心电图、脉搏、血红蛋白、白细胞计数、尿素、血清钠、血清钾、Glasgow评分。(2)术中情况:手术创伤程度、1个月内手术次数、失血量、腹腔污染情况、手术类型。(3)术后情况:肿瘤恶性程度、肿瘤分期。
E-PASS评分系统包括术前风险评分(PRS)和手术应激评分(SSS)两部分共9项指标,应用PRS和SSS计算综合风险分数(CRS)。PRS包括6项指标即年龄、是否合并严重心脏疾病、是否合并严重肺部疾病、是否合并糖尿病、体能状态指数和美国麻醉医师协会(ASA)分级,SSS包括3项指标即术中失血体重比、手术持续时间和切口类型。
1.3 统计学方法 应用Microsoft office 2010和SPSS 20.0统计软件进行数据整理和统计学分析。根据各评分系统计算公式[2-5]结合相应参数进行计算,得出相应评分。应用受试者工作特征(ROC)曲线评价POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统预测结直肠癌患者术后病死率的价值,并使用实际发生率/预测发生率(O/E)比较各评分系统预测术后病死率与实际病死率的差距。检验水准为双侧α=0.05。
2 结果
2.1 一般资料 本研究共纳入550例患者,其中男281例(51.1%),女269例(48.9%);年龄27~95岁,中位年龄65岁;结肠癌375例(68.2%),直肠癌175例(31.8%);择期手术510例(92.7%),急诊手术40例(7.3%);开腹手术397例(72.2%),腹腔镜手术153例(27.8%);根治性切除489例(88.9%),非根治性切除61例(11.1%);TNM分期为Ⅰ期59例(10.7%),Ⅱ期235例(42.7%),Ⅲ期187例(34.1%),Ⅳ期69例(12.5%)。术后30 d内死亡6例,实际病死率为1.1%。其中2例死于肺感染,2例死于吻合口瘘,1例死于胰瘘,1例死于腹腔内出血(见表1)。
2.2 POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统预测结直肠癌患者术后死亡风险能力 POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统预测结直肠癌患者术后病死率分别为8.5%、2.6%、4.4%、1.5%。POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统预测结直肠癌患者术后病死率均高于实际病死率,O/E分别为0.128、0.414、0.248、0.712。E-PASS评分系统预测结直肠癌患者术后病死率与实际病死率最接近。各评分系统预测结直肠癌患者术后死亡的最佳截断值、灵敏度和特异度见表2。
POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统预测结直肠癌患者术后死亡的ROC曲线下面积分别为0.733〔95%CI(0.500,0.966)〕、0.713〔95%CI(0.479,0.948)〕、0.751〔95%CI(0.570,0.932)〕、0.781〔95%CI(0.607,0.955)〕(见图1)。

表1 不同患者术后30 d病死率

图1 POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统预测结直肠癌患者术后死亡的ROC曲线
Figure1 ROCs of POSSUM,P-POSSUM,Cr-POSSUMand E-PASS scoring systems in predicting postoperative mortality of colorectal cancer patients
表2 各评分系统预测结直肠癌患者术后死亡的最佳截断值、灵敏度、特异度
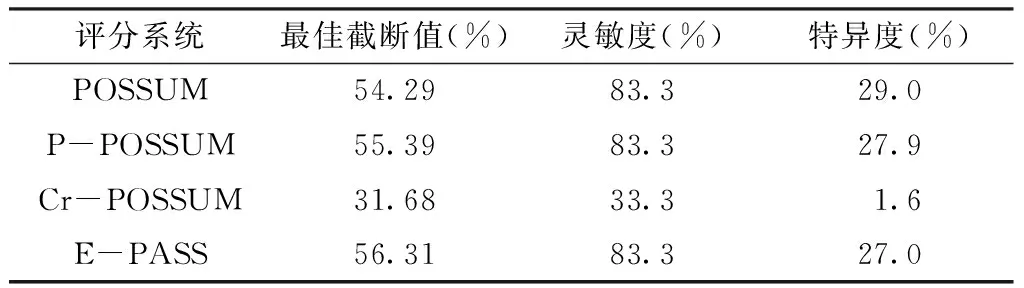
Table 2 Cutoff values,sensitivityand specificity of each scoring systems
3 讨论
目前手术治疗仍是结直肠癌最主要治疗方式。作为一种创伤性过程,结直肠癌手术存在一定风险。外科医生在临床决策过程中需要考虑如何有效降低术后病死率和并发症发生率。在临床工作中,外科医生习惯于依据经验制订临床决策以减少手术相关的不良后果。研究者们在分析大量病历的基础上发现了影响外科手术风险的各种因素,从而建立了一系列评分系统,以便更加客观地预测手术风险[7]。
COPELAND等[2]对1 440例手术患者进行回顾性研究,于1991年推出POSSUM评分系统,使用12种术前生理指标和6种手术侵袭度指标作为预测因素预测患者术后30 d病死率,广泛应用于外科手术风险预测,并在结直肠癌手术中得到推广。有研究报道,POSSUM评分系统会高估结直肠癌患者术后病死率[8-9]。针对高估低危组病死率的情况,PRYTHERCH等[3]通过修改预测方程式提出了新的评分系统P-POSSUM,预测指标与POSSUM相同,但对术后病死率的预测能力却得到提高[10]。为了更加针对性地对结直肠癌手术进行预测,TEKKIS等[4]通过改进原POSSUM评分系统,提出了以结直肠癌手术患者为数据库来源的评分系统Cr-POSSUM,同时将POSSUM中预测指标简化为6个术前生理指标和4个手术侵袭度指标,较POSSUM与P-POSSUM使用更方便,预测正确率更高[11]。E-PASS评分系统由HAGA等[5]建立,最初针对手术创伤与机体反应之间关系进行评估,包括6个术前风险指标和3个手术应激指标,预测正确率较高[12-13]。
本研究结果显示,POSSUM、P-POSSUM、Cr-POSSUM评分系统预测结直肠癌患者术后死亡的ROC曲线下面积均处于0.700~0.800,显示3种评分系统对结直肠癌患者术后病死率的预测具有一定价值。但是,各评分系统预测结直肠癌患者术后的总体病死率均高于实际病死率(1.1%),与国内有些研究结果相似[14]。其中,POSSUM评分系统预测结直肠癌患者术后病死率约为实际病死率的8倍。在4种评分系统中,E-PASS评分系统预测结直肠癌患者术后死亡的ROC曲线下面积为0.781,O/E最接近于1,说明其预测结直肠癌患者术后死亡风险与实际病死率的一致性较好。
POSSUM、P-POSSUM、Cr-POSSUM评分系统的预测结果偏高,可能与其评分指标主要依据白种人、发达国家的患者建立,但是亚洲国家结直肠癌围术期病死率低于英美国家有关[15-16]。E-PASS评分系统预测结果与实际结果近似,可能是由于其是在分析902例行胃肠手术的亚洲国家患者病历资料上建立的,更适合中国患者应用。国内已有应用E-PASSA评分系统预测手术风险的研究,刘宁波等[17]运用E-PASS评分系统预测胃癌患者术后病死率,显示预测病死率与实际病死率有较好的一致性,并且E-PASS评分系统在预测结肠癌患者术后早期并发症发生风险中也显示出较好的评估效果[1]。与POSSUM相关评分系统相比,E-PASS评分系统中手术应激指标包括ASA分级,由于不同麻醉医师对ASA分级的判定结果不同,可能会导致数据偏倚。本研究由于死亡人数较少,也会对结果造成一定影响。
总体而言,POSSUM、P-POSSUM、Cr-POSSUM、E-PASS评分系统在国内结直肠癌患者手术风险预测中具有一定应用价值,E-PASS评分系统预测结直肠癌患者术后病死率与实际病死率一致性较好。由于目前的评分系统数据库均为开腹手术患者,腹腔镜技术应用越来越广泛,其与开腹手术差别较大[7],各评分系统是否需要对原有参数、方程式做进一步调整,以适应预测腹腔镜手术风险,还需要进一步前瞻性研究予以证实。
作者贡献:刘婷婷进行文章的构思与设计,文章的可行性分析;刘婷婷、张骜进行资料收集、整理,撰写论文;胡芳进行论文的修订,质量控制及审校。
本文无利益冲突。
[1]高强,汪晓东,唐之韵,等.生理能力与手术侵袭度评分系统评估结肠癌手术风险的临床价值[J].中华消化外科杂志,2010,9(6):415-417.DOI:10.3760/cma.j.issn.1673-9752.2010.06.006. GAO Q,WANG X D,TANG Z Y,et al.Estimation of physiologic ability and surgical stress as a prediction scoring system for colonic surgery[J].Chinese Journal of Digestive Surgery,2010,9(6):415-417.DOI:10.3760/cma.j.issn.1673-9752.2010.06.006.
[2]COPELAND G P,JONES D,WALTERS M.POSSUM:a scoring system for surgical audit[J].Br J Surg,1991,78(3):355-360.
[3]PRYTHERCH D R,WHITELEY M S,HIGGINS B,et al.POSSUM and Portsmouth POSSUM for predicting mortality.Physiological and operative severity score for the enumeration of mortality and morbidity[J].Br J Surg,1998,85(9):1217-1220.DOI:10.1046/j.1365-2168.1998.00840.x.
[4]TEKKIS P P,PRYTHERCH D R,KOCHER H M,et al.Development of a dedicated risk-adjustment scoring system for colorectal surgery(colorectal POSSUM)[J].Br J Surg,2004,91(9):1174-1182.DOI:10.1002/bjs.4430.
[5]HAGA Y,IKEI S,OGAWA M.Estimation of Physiologic Ability and Surgical Stress(E-PASS) as a new prediction scoring system for postoperative morbidity and mortality following gastrointestinal surgery[J].Surg Today,1999,29(3):219-225.DOI:10.1007/BF02483010.
[6]HAGA Y,MIYAMOTO A,WADA Y,et al.Value of E-PASS models for predicting postoperative morbidity and mortality in resection of perihilar cholangiocarcinoma and gallbladder carcinoma[J].HPB(Oxford),2016,18(3):271-278.DOI:10.1016/j.hpb.2015.09.001.
[7]董景五.疾病和有关健康问题的国际统计分类[M].北京:人民卫生出版社,2008:145-155.
[8]李爽,魏正强.四种评分系统在结直肠癌手术风险预测中的运用现状[J].检验医学与临床,2013,10(17):2321-2322,2352.DOI:10.3969/j.issn.1672-9455.2013.17.058. LI S,WEI Z Q.Application of four scoring systems in predicting the risk of colorectal cancer surgery [J].Laboratory Medicine and Clinic,2013,10(17):2321-2322,2352.DOI:10.3969/j.issn.1672-9455.2013.17.058.
[9]路忠志,李丽,杨宏伟,等.POSSUM及P-POSSUM对胃肠外科手术风险度的评价[J].中国普通外科杂志,2010,19(4):409-413. LU Z Z,LI L,YANG H W,et al.An evaluation of PQSSUM and P-POSSUM on surgical risk scoring in general surgery[J].Chinese Journal of General Surgery,2010,19(4):409-413.
[10]YAN J,WANG Y X,LI Z P.Predictive value of the POSSUM,P-POSSUM,Cr-POSSUM,APACHE Ⅱ and ACPGBI scoring systems in colorectal cancer resection[J].J Int Med Res,2011,39(4):1464-1473.DOI:10.1177/147323001103900435.
[11]WIJESINGHE L D,MAHMOOD T,SCOTT D J,et al.Comparison of POSSUM and the Portsmouth predictor equation for predicting death following vascular surgery[J].Br J Surg,1998,85(2):209-212.DOI:10.1046/j.1365-2168.1998.00709.x.
[12]LEUNG E,FERJANI A M,STELLARD N,et al.Predicting post-operative mortality in patients undergoing colorectal surgery using P-POSSUM and Cr-POSSUM scores:a prospective study[J].Int J Colorectal Dis,2009,24(12):1459-1464.DOI:10.1007/s00384-009-0781-4.
[13]TANG T,WALSH S R,FANSHAWE T R,et al.Estimation of physiologic ability and surgical stress(E-PASS) as a predictor of immediate outcome after elective abdominal aortic aneurysm surgery[J].Am J Surg,2007,194(2):176-182.DOI:10.1016/j.amjsurg.2006.10.032.
[14]HIROSE J,MIZUTA H,IDE J,et al.Evaluation of estimation of physiologic ability and surgical stress(E-PASS) to predict the postoperative risk for hip fracture in elder patients[J].Arch Orthop Trauma Surg,2008,128(12):1447-1452.DOI:10.1007/s00402-007-0551-0.
[15]任立焕,傅卫,王亮,等.POSSUM、P-POSSUM和Cr-POSSUM对结直肠癌患者住院期间病死率预测能力的比较[J].中华普通外科杂志,2008,23(4):241-244.DOI:10.3760/j.issn:1007-631X.2008.04.001. REN L H,FU W,WANG L,et al.In-hospital morbidity and mortality for patients of colorectal cancer evaluated by three different POSSUM models[J].Chinese Journal of General Surgery,2008,23(4):241-244.DOI:10.3760/j.issn:1007-631X.2008.04.001.
[16]张春,傅卫,任立涣,等.五种结直肠癌评分系统对中国患者的预测价值[J].中华普通外科杂志,2013,28(1):16-19.DOI:10.3760/cma.j.issn.1007-631X.2013.01.005.
[17]刘宁波,崔建功,张增强,等.生理能力与手术应激评分系统和改良的生理能力与手术应激评分系统在预测胃癌术后死亡率和手术风险中的价值[J].中华肿瘤杂志,2015,37(10):753-758.DOI:10.3760/cma.j.issn.0253-3766.2015.10.008.
(本文编辑:崔莎)
ValueofPOSSUM,P-POSSUM,Cr-POSSUMandE-PASSScoringSysteminPredictingPostoperativeMortalityRiskofColorectalCancerPatients
LIUTing-ting,ZHANGAo,HUFang*
DepartmentofGeneralSurgery,TianjinMedicalUniversityGeneralHospital,Tianjin300052,China
*Correspondingauthor:HUFang,Associatechiefsuperintendentnurse;E-mail:hxc5286@sina.com
ObjectiveTo evaluate the value of POSSUM,P-POSSUM,Cr-POSSUM and E-PASS scoring systems in predicting postoperative mortality risk of colorectal cancer patients.MethodsThe clinical data of 550 patients with colorectal cancer treated in Tianjin Medical University General Hospital from 2010 to 2015 were retrospectively analyzed.The relevant indicators were collected according to Physiological and Operative Severity Score for Enumeration of Mortality and morbidity(POSSUM),Portsmouth-POSSUM(P-POSSUM),Colorectal POSSUM(Cr-POSSUM)and Estimation of physiologic ability and surgical stress(E-PASS)scoring systems andresearchneeds.The POSSUM,P-POSSUM,Cr-POSSUM and E-PASS scoring systems were used to predict the postoperative mortality rate of 30 days in patients with colorectal cancer.The predictive value of the scoring system was evaluated by receiver operating characteristic(ROC) curve and observed to expected ratio(O/E).ResultsThe best cutoff value of POSSUM,P-POSSUM,Cr-POSSUM and E-PASSscoring systems were 54.29%,55.39%,31.68% and 56.31%,respectively.The sensitivity of POSSUM,P-POSSUM,Cr-POSSUM and E-PASS scoring systems were 83.3%,83.3%,33.3% and 83.3%,respectively.The specificity of POSSUM,P-POSSUM,Cr-POSSUM and E-PASSscoring systems were 29.0%,27.9%,1.6% and 27.0%,respectively.The area under ROC curve of POSSUM,P-POSSUM,Cr-POSSUM and E-PASS scoring systems were 0.733〔95%CI(0.500,0.966)〕,0.713〔95%CI(0.479,0.948)〕,0.751〔95%CI(0.570,0.932)〕,and 0.781〔95%CI(0.607,0.955)〕,respectively.The O/E were 0.128,0.414,0.248,0.712,respectively.ConclusionPOSSUM,P-POSSUM,Cr-POSSUM and E-PASS scoring systems all have an overestimation of the postoperative mortality of colorectal cancer.E-PASS scoring system has a good consistency in the predicting postoperative mortality and actual mortality.
Colorectal neoplasm;Mortality;Forecasting
R 735.34
A
10.3969/j.issn.1007-9572.2017.07.y14
2017-02-15;
2017-05-24)
300052天津市,天津医科大学总医院普外科
*通信作者:胡芳,副主任护师;E-mail:hxc5286@sina.com

