儿童阻塞性睡眠呼吸暂停低通气综合征血压变异性和血清中炎性因子表达水平及临床意义
王宇光,刘 佳,白云飞
儿童阻塞性睡眠呼吸暂停低通气综合征血压变异性和血清中炎性因子表达水平及临床意义
王宇光,刘 佳,白云飞
目的 探讨儿童阻塞性睡眠呼吸暂停低通气综合征(obstructive sleep apnea-hypopnea syndrome, OSAHS)血压变异性和血清中炎性因子表达水平及临床意义。方法 选取2014年6月—2016年6月内蒙古医科大学第二附属医院收治的诉有睡眠打鼾及白天嗜睡等症状且符合儿童OSAHS诊断标准65例作为儿童OSAHS组,无上述症状常规体检正常儿童22例作为正常对照组,两组均进行夜间多导睡眠监测(polysomnography, PSG)。按疾病不同程度将65例儿童OSAHS分为轻度OSAHS组(27例)、中度OSAHS组(23例)和重度OSAHS组(15例)3组。观察比较正常对照组和儿童OSAHS组一般资料,正常对照组与不同程度儿童OSAHS 3组各血压参数、心率、血氧饱和度和血清炎性因子水平,并对儿童OSAHS严重程度与血压变异性及其他各危险因素的相关性进行分析。结果 正常对照组与儿童OSAHS组体重指数及OSAHS家族史比较差异有统计学意义(P<0.05)。正常对照组与不同程度儿童OSAHS 3组24 h平均血压、白天平均血压、夜间平均血压、夜间血压下降率、非勺型血压率、血氧饱和度及血清肿瘤坏死因子(TNF)-α、白细胞介素(IL)-4、IL-6及IL-8水平总体比较差异均有统计学意义(P<0.05)。不同程度儿童OSAHS 3组24 h平均血压、白天平均血压、夜间平均血压、非勺型血压率及血清TNF-α、IL-4、IL-6、IL-8水平均高于对照组,差异有统计学意义(P<0.05);且儿童OSAHS越严重24 h平均血压、白天平均血压、夜间平均血压、非勺型血压率及血清TNF-α、IL-4、IL-6、IL-8水平越高,不同程度儿童OSAHS 3组间同一指标两两比较差异均有统计学意义(P<0.05)。夜间血压下降率不同程度儿童OSAHS 3组均明显低于正常对照组,差异有统计学意义(P<0.05);且儿童OSAHS越严重夜间血压下降率越低,不同程度儿童OSAHS 3组间两两比较差异均有统计学意义(P<0.05)。血氧饱和度重度儿童OSAHS组明显低于正常对照组、轻度儿童OSAHS组和中度儿童OSAHS组,差异均具有统计学意义(P<0.05)。协方差分析显示夜间平均血压、非勺型血压率与儿童OSAHS严重程度呈正相关(P<0.05),而夜间血压下降率与儿童OSAHS严重程度呈负相关(P<0.05)。Pearson相关分层分析显示,体重指数及血清TNF-α、IL-4、IL-6、IL-8水平与儿童OSAHS严重程度呈正相关(P<0.05)。结论 儿童OSAHS和高血压、血清炎性因子水平密切相关,夜间平均血压、非勺型血压率、体重指数及血清TNF-α、IL-4、IL-6、IL-8水平与儿童OSAHS严重程度呈正相关,而夜间血压下降率与儿童OSAHS严重程度呈负相关。
睡眠呼吸暂停,阻塞性;儿童;高血压;炎性因子
儿童阻塞性睡眠呼吸暂停低通气综合征(obstructive sleep apnea-hypopnea syndrome, OSAHS)是一种临床常见疾病,临床主要表现为睡眠打鼾及张口呼吸等,严重扰乱儿童正常通气、睡眠结构和面部发育[1]。儿童OSAHS最常见病因是腺样体肥大,肥大增生的腺样体易反复发生炎症,从而引起一系列细胞因子及炎性介质水平改变[2]。有研究表明OSAHS是引起高血压的独立危险因素,高达50%的OSAHS患者合并高血压病[3]。值得注意的是,目前临床上儿童OSAHS与高血压关系的研究较少,且现有结论仍有争议[4-6]。本研究通过比较儿童OSAHS患儿和正常儿童24 h血压变异性及血清炎性因子肿瘤坏死因子(tumor necrosis factor, TNF)-α、白细胞介素(IL)-4、IL-6、IL-8、C反应蛋白(CRP)水平,探讨儿童OSAHS血压变异性和血清中炎性因子表达水平及临床意义。
1 对象与方法
1.1 研究对象 选取2014年6月—2016年6月内蒙古医科大学第二附属医院收治的诉有睡眠打鼾及白天嗜睡等症状且符合儿童OSAHS诊断标准[7]65例作为儿童OSAHS组,无上述症状且常规体检正常儿童22例作为正常对照组,两组均进行夜间多导睡眠监测(polysomnography, PSG)。排除1周内有上呼吸道感染及过敏等患儿以及有先天性心肺疾病患儿。按疾病不同程度将65例儿童OSAHS分为轻度OSAHS组(27例)、中度OSAHS组(23例)和重度OSAHS组(15例)3组。
1.2 观察指标 观察比较正常对照组和儿童OSAHS组一般资料,正常对照组与不同程度儿童OSAHS 3组各血压参数、心率、血氧饱和度和血清炎性因子水平,并对儿童OSAHS严重程度与血压变异性及其他各危险因素的相关性进行分析。
1.3 方法
1.3.1 PSG监测:所有儿童均采用美国德邦PSG系统进行整夜7 h连续PSG监测,记录呼吸暂停低通气指数(AHI)及血氧饱和度。AHI≥5及最低血氧饱和度<0.92时诊断为OSAHS[7]。根据AHI确定儿童OSAHS严重程度[7]:AHI 5~20为轻度,AHI 20~40为中度,AHI≥40为重度。
1.3.2 血压监测:所有儿童均采用多功能监护仪进行血压监测,24 h内每30 min测定1次血压,包括收缩压(SBP)、舒张压(DBP)及脉压,测量期间避免剧烈运动。24 h平均血压、白天平均血压、夜间平均血压=血压值之和/测量次数;夜间血压下降率=(白天平均血压-夜间平均血压)/白天平均血压×100%,其值≥10%为血压昼夜节律正常(即勺型血压),而<10%为血压昼夜节律减弱或消失(即非勺型血压)。
1.3.3 TNF-α、IL-4、IL-6、IL-8及CRP测定:所有儿童均晨起抽取空腹静脉血5 ml,置于离心管中2000 r/min离心15 min,取上层血清。采用酶联免疫吸附试验(ELISA)法测定血清中TNF-α、IL-4、IL-6、IL-8、CRP水平,ELISA试剂盒购自南京森倍加生物公司,严格按照试剂盒说明书进行操作。

2 结果
2.1 正常对照组和儿童OSAHS组一般资料比较 正常对照组与儿童OSAHS组性别、年龄、身高和肥胖率比较差异无统计学意义(P>0.05);而体重指数及OSAHS家族史比较差异有统计学意义(P<0.05),见表1。

表1 正常对照组与儿童OSAHS组一般资料比较,例(%)]
注:OSAHS 为阻塞性睡眠呼吸暂停低通气综合征
2.2 正常对照组与不同程度儿童OSAHS 3组血压、心率及血氧饱和度比较 正常对照组与不同程度儿童OSAHS 3组24 h平均血压、白天平均血压、夜间平均血压、夜间血压下降率、非勺型血压率及血氧饱和度总体比较差异均有统计学意义(P<0.05)。不同程度儿童OSAHS 3组24 h平均血压、白天平均血压、夜间平均血压、非勺型血压率均明显高于正常对照组,差异有统计学意义(P<0.05);且儿童OSAHS越严重24 h平均血压、白天平均血压、夜间平均血压、非勺型血压率越高,不同程度儿童OSAHS 3组间同一指标两两比较差异均有统计学意义(P<0.05)。夜间血压下降率不同程度儿童OSAHS 3组均明显小于正常对照组,差异有统计学意义(P<0.05);且儿童OSAHS越严重夜间血压下降率越低,不同程度儿童OSAHS 3组间两两比较差异均有统计学意义(P<0.05)。血氧饱和度重度儿童OSAHS组明显低于正常对照组、轻度儿童OSAHS组和中度儿童OSAHS组,差异均具有统计学意义(P<0.05);正常对照组、轻度儿童OSAHS组和中度儿童OSAHS组3组间两两比较差异均无统计学意义(P>0.05)。 见表2。

表2 正常对照组与不同程度儿童OSAHS 3组血压、心率及血氧饱和度比较±s,例(%)]
注:OSAHS为阻塞性睡眠呼吸暂停低通气综合征;与正常对照组比较,aP<0.05;与轻度儿童OSAHS组比较,cP<0.05;与中度儿童OSAHS组比较,eP<0.05
2.3 正常对照组与不同程度儿童OSAHS 3组血清炎性因子水平比较 正常对照组与不同程度儿童OSAHS 3组血清TNF-α、IL-4、IL-6及IL-8水平总体比较差异均有统计学意义(P<0.05)。不同程度儿童OSAHS 3组血清TNF-α、IL-4、IL-6及IL-8水平均明显高于正常对照组,差异有统计学意义(P<0.05);且儿童OSAHS越严重血清TNF-α、IL-4、IL-6及IL-8水平越高,不同程度儿童OSAHS 3组间同一指标两两比较差异均有统计学意义(P<0.05)。见表3。

表3 正常对照组与不同程度儿童OSAHS 3组血清炎性因子水平比较±s)
注:OSAHS 为阻塞性睡眠呼吸暂停低通气综合征;与正常对照组比较,aP<0.05;与轻度儿童OSAHS组比较,cP<0.05;与中度儿童OSAHS组比较,eP<0.05
2.4 儿童OSAHS严重程度与血压变异性及其他各危险因素的相关性分析 协方差分析显示夜间平均血压、非勺型血压率与儿童OSAHS严重程度呈正相关(P<0.05),而夜间血压下降率与儿童OSAHS严重程度呈负相关(P<0.05),见表4。Pearson相关分层分析显示,体重指数及血清TNF-α、IL-4、IL-6、IL-8水平与儿童OSAHS严重程度呈正相关(P<0.05),见表5。
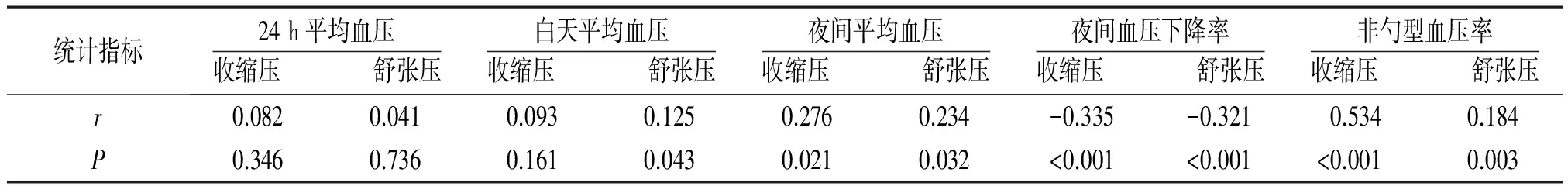
表4 儿童OSAHS严重程度与血压变异性的相关性分析
注:OSAHS 为阻塞性睡眠呼吸暂停低通气综合征
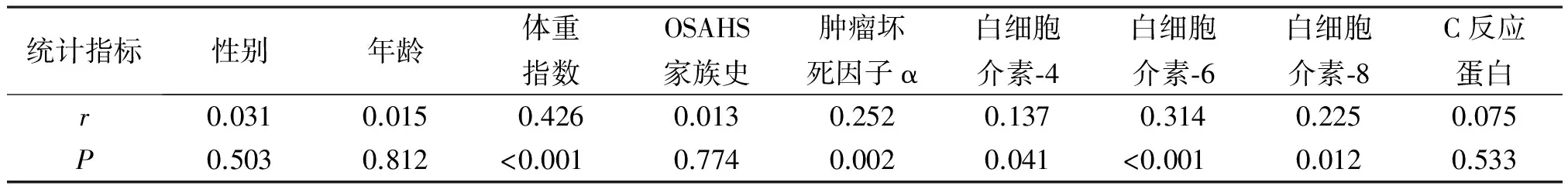
表5 儿童OSAHS严重程度与其他各危险因素的相关性分析
注:OSAHS 为阻塞性睡眠呼吸暂停低通气综合征
3 讨论
OSAHS是一种以反复高碳酸血症和低氧血症为病理改变并造成多个系统功能损害的临床综合征。OSAHS在儿童中发病率为1.2%~5.7%,严重影响儿童身心发展[8-10]。
正常人群因受生理活动和睡眠影响,24 h内血压值并非一成不变,而是日间高夜间低,夜间血压较日间约下降10%~15%,呈典型的勺状分布,这种血压变异模式对维持正常生理活动有重要的作用[11]。Garcia Rio等[12]发现OSAHS患者慢性缺氧和二氧化碳潴留状态可引起肺动脉高压、交感神经兴奋,从而导致高血压。Feres等[13]发现OSAHS患者血、尿儿茶酚胺含量无论在白天还是夜间均显著高于正常者,证实了OSAHS通过兴奋交感神经致高血压;后期进一步通过24 h动态血压监测发现,OSAHS患者早期主要表现为夜间动脉血压升高,重度OSAHS患者则全天血压增高。Weiss等[14]明确指出OSAHS患者24 h血压呈浅勺型模式,甚至昼夜变化节律消失。本研究发现儿童OSAHS血压变异性类似于成人OSAHS,夜间血压变异率减小或消失,呈非勺型血压,且与儿童OSAHS严重程度呈负相关。另外,本研究发现儿童OSAHS舒张压非勺型发生率较收缩压高,这与Lee和Jeong[15]发现OSAHS患者舒张期高血压的结果一致。非勺型高血压与普通高血压相比具有隐匿性,不宜早期发现,当OSAHS患者出现日间高血压时疾病大多已发展至重度。另外,有研究显示非勺型高血压较普通高血压对心脏功能影响更大,Ermis等[16]发现非勺型高血压患者病死率是勺型高血压患者的4~5倍。因此,儿童OSAHS治疗对儿童高血压和血压夜间变异改善有着重要意义。既往也有研究表明口腔矫正器对儿童OSAHS疗效显著[17]。
儿童OSAHS最常见的病因是腺样体肥大,腺样体是咽部淋巴环(Waldeyer环)的重要组成部分,具有阻挡致病菌并释放炎性因子的免疫功能,有研究表明缺氧状态刺激腺样体产生炎性因子[18]。本研究结果显示,正常对照组与不同程度儿童OSAHS 3组血清TNF-α、IL-4、IL-6及IL-8水平总体比较差异均有统计学意义,而血清CRP水平总体比较差异无统计学意义;不同程度儿童OSAHS 3组血清TNF-α、IL-4、IL-6及IL-8水平均明显高于正常对照组,且儿童OSAHS越严重血清TNF-α、IL-4、IL-6及IL-8水平越高;Pearson相关分层分析显示,体重指数及血清TNF-α、IL-4、IL-6、IL-8水平与儿童OSAHS严重程度呈正相关,而血清CRP水平与儿童OSAHS严重程度无相关性。分析其可能的原因是CRP是一种急性期炎性指标,对如OSAHS之类的慢性炎症不敏感。TNF-α是一种具有多种生物学功能的细胞因子,参与辅助性T淋巴细胞(Th)1细胞免疫反应,激活NF-κB,诱导细胞凋亡。Zhong等[19]研究发现中重度儿童腺样体肥大组血清TNF-α水平较健康对照组明显增加。而IL-4则是主要参与Th2细胞免疫反应的炎性因子,且IL-4促进B细胞增殖参与体液免疫。Anderson等[20]发现儿童OSAHS患儿血清IL-4水平较高。IL-6促进T细胞和炎性细胞释放多种促炎细胞因子,加重局部炎症反应。Martinez等[21]研究发现与正常对照患者相比OSAHS患者血清IL-6升高。IL-8的主要功能是趋化炎性细胞向损伤部位聚集,有学者发现OSAHS患者血清IL-8水平也升高[22]。既往研究和本研究结果说明炎性因子参与OSAHS患者一系列病理生理改变,血清炎性因子测定可以辅助判断儿童OSAHS病情严重程度[23]。
综上所述,本研究证实儿童OSAHS和高血压、血清炎性因子水平密切相关,夜间平均血压、非勺型血压率、体重指数及血清TNF-α、IL-4、IL-6、IL-8水平与儿童OSAHS严重程度呈正相关,而夜间血压下降率与儿童OSAHS严重程度呈负相关。提示血压变异性和血清炎性因子水平可作为判断儿童OSAHS治疗效果的重要指标。
[1] Marcus C L, Brooks L J, Draper K A,etal. Diagnosis and management of childhood obstructive sleep apnea syndrome[J].Pediatrics, 2012,130(3):714-755
[2] Musiatowiwcz M, Koda M, Sulkowski S. The TIMP-1 expression in germinal centers of hypertrophied adenoids in children[J].Int J Pediatr Otorhinolaryngol, 2013,77(3):384-388.
[3] Wang Y, Yang Q, Feng J,etal. The prevalence and clinical features of hypertension in patients with obstructive sleep apnea hypopnea syndrome and related nursing strategies[J].J Nurs Res, 2016,24(1): 41-47.
[4] 王燕,姜艳蕊,孙莞绮,等.儿童阻塞性睡眠呼吸暂停低通气综合征与血压相关性研究[J].中国循证儿科杂志,2014,9(3):161-166.
[5] Archbold K H, Vasquez M M, Goodwin J L,etal. Effects of sleep patterns and obesity on increases in blood pressure in a 5-year period: report from the Tucson Children's Assessment of Sleep Apnea Study[J].J Pediatr, 2012,161(1):26- 30.
[6] Zintzaras E, Kaditis A G. Sleep-disordered breathing and blood pressure in children: a meta-analysis[J].Arch Pediatr Adolesc Med, 2007,161(2):172-178.
[7] 作者不详.儿童阻塞性睡眠呼吸暂停低通气综合征诊疗指南草案(乌鲁木齐)[J].中华耳鼻咽喉头颈外科杂志,2007,42(2):83-84.
[8] Hunter S J, Gozal D, Smith D L,etal. Effect of sleep-disordered breathing severity on cognitive performance measures in a large community cohort of young school-aged children[J].Am J Respir Crit Care Med, 2016,194(6):739-747.
[9] Bixler E O, Fernandez Mendoza J, Liao D,etal. Natural history of sleep disordered breathing in prepubertal children transitioning to adolescence[J].Eur Respir J, 2016,47(5):1402-1409.
[10]Li A M, So H K, Au C T,etal. Epidemiology of obstructive sleep apnoea syndrome in Chinese children: a two-phase community study[J].Thorax, 2010,65(11): 991- 997.
[11]李慧妍,刘越.血压变异性与靶器官损害关系的研究进展[J].中国急救医学,2016,36(8):758-762.
[12]Garcia Rio F, Racionero M A, Pino J M,etal. Sleep apnea and hypertension[J].Chest, 2000,117(5):1417-1425.
[13]Feres M C, Cintra F D, Rizzi C F,etal. Evaluation and validation of a method for determining platelet catecholamine in patients withobstructive sleep apnea and arterial hypertension[J].PLoS One, 2014,9(6):98407.
[14]Weiss J W, Tamisier R, Liu Y. Sympathoexcitation and arterial hypertension associated with obstructive sleep apnea and cyclic intermittent hypoxia[J].J Appl Physiol (1985), 2015,119(12):1449-1454.
[15]Lee Y J, Jeong D U. Obstructive sleep apnea syndrome is associated with higher diastolic blood pressure in men but not in women[J].Am J Hypertens, 2014,27(3):325-330.
[16]Ermis N, Otlu Y O, Afsin A,etal. Comparison of left atrial volume and function in non-dipper versus dipper hypertensives: A real-time three-dimensional echocardiography study[J].Anatol J Cardiol, 2016,16(6):428-433.
[17]Lettieri C J, Paolino N, Eliasson A H,etal. Comparison of adjustable and fixed oral appliances for the treatment of obstructive sleep apnea[J].J Clin Sleep Medici, 2011,7(5):439-445.
[18]Ryan S, Taylor C T, McNicholas W T. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea sydrome[J].Circulation, 2005,112(7):2660-2667.
[19]Zhong A, Xiong X, Xu H,etal. An updated meta-analysis of the association between tumor necrosis factor-α -308G/Apolymorphism and obstructive sleep apnea-hypopnea syndrome[J].Plos One, 2014,9(9):106270.
[20]Anderson M E Jr, Buchwald Z S, Ko J,etal. Patients with pediatric obstructive sleep apnea show altered T-Cell populations with a dominant TH17 profile[J].Otolaryngol Head Neck Surg, 2014,150(5):880-886.
[21]Martinez Ceron E, Barquiel B, Bezos A M,etal. Effect of continuous positive airway pressure on glycemic control in patients with obstructive sleep apnea and type 2 diabetes a randomized clinical trial[J].Am J Respir Crit Care Med, 2016,194(4):476-485.
[22]Zychowski K E, Sanchez B, Pedrosa R P,etal. Serum from obstructive sleep apnea patients induces inflammatory responses in coronary artery endothelial cells[J].Atherosclerosis, 2016,254:59-66.
[23]de Lima F F, Mazzotti D R, Tufik S,etal. The role inflammatory response genes in obstructive sleep apnea syndrome: a review[J].Sleep Breath, 2016,20(1):331-338.
Blood Pressure Variability and Expressions and Clinical Significances of Serum Inflammatory Factors in Children with Obstructive Sleep Apnea Hypopnea Syndrome
WANG Yu-guang1, LIU Jia2a, BAI Yun-fei2b
(1. Department of Medical Imaging, the Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010030, China; a. Department of Stomatology, b. Department of Otolaryngology, 2. Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010050, China)
Objective To investigate blood pressure variability and expressions and clinical significances of serum inflammatory factors in children with obstructive sleep apnea hypopnea syndrome (OSAHS). Methods A total of 65 OSAHS children with symptoms of snoring during sleeping and daytime sleepiness admitted during June 2014 and June 2016 were selected as OSAHS group, and other 22 healthy children without above symptoms were selected as control group, and children in both groups were monitored by overnight polysomnography (PSG). The 65 children with OSAHS were divided into mild OSAHS subgroup (n=27), moderate OSAHS subgroup (n=23) and severe OSAHS subgroup (n=15) according to OSAHS grades. General informations between OSAHS group and control group, and parameters of blood pressure, heart rate, blood oxygen saturation and serum inflammatory factor levels between control group and 3 OSAHS subgroups were observed and compared, and then correlations between grade of OSAHS severity with blood pressure variability and other risk factors were analyzed. Results There were significant differences in body mass index (BMI) and family history of OSAHS between OSAHS and control groups (P<0.05). There were significant differences in 24 h mean blood pressure, daytime average blood pressure, nighttime average blood pressure, descent rate of nighttime blood pressure, non dipper blood pressure rate, blood oxygen saturation, serum tumor necrosis factor-α (TNF-α), Interleukin-4 (IL-4), IL-6 and IL-8 between control group with 3 OSAHS subgroups (P<0.05). Values of 24h mean blood pressure, daytime average blood pressure, nighttime average blood pressure, non dipper blood pressure rate, serum TNF-α, IL-4, IL-6 and IL-8 levels in 3 OSAHS subgroups were significantly higher than those in control group (P<0.05), and the more severity of OSAHS in children, the higher values of 24h mean blood pressure, daytime average blood pressure, nighttime average blood pressure, non dipper blood pressure rate, serum TNF-α, IL-4, IL-6 and IL-8 levels they had, and the differences in the same index between each two groups among the 3 OSAHS subgroups were statistically significant (P<0.05). Descent rates of nighttime blood pressure in 3 OSAHS subgroups were significantly lower than that in control group (P<0.05), and the more severity of OSAHS in children, the lower descent rate of nighttime blood pressure the children had, and the differences in the rate between each two groups among 3 OSAHS subgroups were statistically significant (P<0.05). Level of blood oxygen saturation in severe OSAHS subgroup was significantly lower than those in control group, the mild OSAHS subgroup and moderate OSAHS subgroup (P<0.05). Covariance analysis showed that nighttime average blood pressure and non dipper blood pressure rate were positively correlated with OSAHS severity (P<0.05), while nocturnal blood pressure decreased rate was negatively correlated with OSAHS severity in children(P<0.05). Pearson correlation hierarchical analysis showed that BMI and serum levels of TNF-α, IL-4, IL-6 and IL-8 were positively correlated with OSAHS severity in children (P<0.05). Conclusion OSAHS in children is closely related with hypertension and serum inflammatory factors levels, and nighttime average blood pressure, non dipper blood pressure rate, BMI and serum TNF-α, IL-4, IL-6 and IL-8 are positively correlated with OSAHS severity, while nocturnal blood pressure decreased rate is negatively correlated with OSAHS severity.
Sleep apnea, obstructive; Children; Hypertension; Inflammatory factors
内蒙古自治区卫生和计划生育委员会科研项目(201303049)
010030 呼和浩特,内蒙古医科大学第二附属医院影像科(王宇光);010050 呼和浩特,内蒙古医科大学附属医院口腔科(刘佳),耳鼻喉科(白云飞)
刘佳,电话:13674835551;E-mail:liujiababy@aliyun.com
R563.8
A
1002-3429(2017)08-0070-06
10.3969/j.issn.1002-3429.2017.08.022
2017-06-05 修回时间:2017-07-02)

