自发性脑出血患者入院30 d内死亡的危险因素分析
石海英,张 强,王学静,郝林军
自发性脑出血患者入院30 d内死亡的危险因素分析
石海英,张 强,王学静,郝林军
目的 探讨自发性脑出血患者入院30 d内死亡的危险因素。方法 选择2011年1月—2016年1月内蒙古医科大学附属医院收治的自发性脑出血342例,根据患者入院30 d内是否死亡将其分为病死组(86例)和存活组(256例)两组。观察比较两组主要临床特征,采用受试者工作特征(ROC)曲线下面积分析年龄、格拉斯哥昏迷评分(GCS)和出血量预测自发性脑出血患者入院30 d内死亡的临床价值,采用单因素和多因素Logistic回归分析分析自发性脑出血患者入院30 d内死亡的危险因素。结果 与存活组比较,病死组GCS较低,出血量较大,基底节出血发生率较低,小脑出血发生率及合并脑室出血发生率较高,手术治疗率较低,两组比较差异均有统计学意义 (P<0.05)。经分析ROC曲线下面积发现GCS和出血量预测自发性脑出血患者入院30 d内死亡具有一定临床价值(均P<0.001)。单因素和多因素Logistic回归分析显示GCS、出血量和小脑出血是自发性脑出血患者入院30 d内死亡的独立危险因素。结论 GCS、出血量和小脑出血是自发性脑出血患者入院30 d内死亡的独立危险因素。
脑出血;死亡;危险因素
近年随着高血压病、糖尿病和高脂血症等人群增加,自发性脑出血发病率呈逐年增高趋势[1-2]。自发性脑出血致残率和病死率较高,严重影响中老年患者生活质量[3-4]。自发性脑出血患者死亡高峰主要集中在入院30 d内,Chan等[5]研究显示自发性脑出血患者入院后30 d内和1年内病死率分别为19.8%和29.6%,可见约2/3的自发性脑出血死亡患者死亡时间在入院后30 d内。因此,探讨自发性脑出血患者入院后30 d内死亡的危险因素具有重要临床意义。到目前为止,尽管已有较多研究显示格拉斯哥昏迷评分(glasgow coma scale, GCS)、出血部位、年龄和合并症等是导致自发性脑出血患者死亡的危险因素[6-7],但是现临床探讨自发性脑出血患者入院30内死亡的研究极为缺乏,尤其是国内,尚无相关系统研究。本研究探讨自发性脑出血患者入院30 d内死亡的危险因素,以识别这类高危患者,为临床加强对此类患者的监护与治疗提供依据,从而改善此类患者预后。
1 资料与方法
1.1 一般资料 选择2011年1月—2016年1月内蒙古医科大学附属医院收治的符合纳入及排除标准的自发性脑出血342例。342例中男172例,女170例;年龄(67.32±11.20)岁。GCS评分(9.21±3.66)分。296例合并高血压病,96例合并糖尿病,30例长期嗜酒,86例长期吸烟。158例为基底节出血,134例为脑小叶出血,36例为小脑出血,14例为脑干出血;198例合并脑室出血,32例合并蛛网膜下腔出血;出血量(62.91±59.22)ml。102例行微创或开颅手术进行止血或血肿清除,其余240例采用保守治疗。根据患者入院30 d内是否死亡,将342例分为病死组和存活组两组,病死组86例,存活组256例。本研究经我院伦理委员会批准。
1.2 纳入及排除标准 纳入标准:①自发性脑出血(均有影像学检查如CT或MRI辅助诊断);②临床资料齐全;③发病至入院时间<6 h。排除标准:①创伤性脑出血或其他继发性脑出血;②颅内肿瘤或其他恶性肿瘤;③颅内动静脉畸形;④入院时即死亡(无脑干反射);⑤放弃治疗或治疗期间转院;⑥不配合治疗。
1.3 研究方法和观察指标 观察比较两组主要临床特征,采用受试者工作特征(ROC)曲线下面积分析年龄、GCS和出血量预测自发性脑出血患者入院30 d内死亡的临床价值,采用单因素和多因素Logistic回归分析分析自发性脑出血患者入院30 d内死亡的危险因素。主要临床特征包括年龄、性别、GCS、既往史(高血压病、糖尿病、吸烟和嗜酒)、出血量、出血部位、合并脑室出血、合并蛛网膜下腔出血和手术治疗。

2 结果
2.1 主要临床特征比较 与存活组比较,病死组GCS较低,出血量较大,基底节出血发生率较低,小脑出血发生率及合并脑室出血发生率较高,手术治疗率较低,两组比较差异均有统计学意义 (P<0.05),见表1。

表1 入院30 d内病死和存活自发性脑出血两组主要临床特征比较±s,例(%)]
注:GCS为格拉斯哥昏迷评分
2.2 年龄、GCS和出血量预测自发性脑出血患者入院30 d内死亡的临床价值 年龄、GCS和出血量预测自发性脑出血患者入院30 d内死亡的ROC曲线下面积分别为0.563(0.490,0.636)、0.812(0.784,0.840)和0.821(0.772,0.870),经分析发现GCS和出血量预测自发性脑出血患者入院30 d内死亡具有一定临床价值(均P<0.001),年龄预测自发性脑出血患者入院30 d内死亡未发现临床价值(P=0.738)。
2.3 自发性脑出血患者入院30 d内死亡的危险因素分析 单因素和多因素Logistic回归分析显示GCS、出血量和小脑出血是自发性脑出血患者入院30 d内死亡的独立危险因素,见表2。
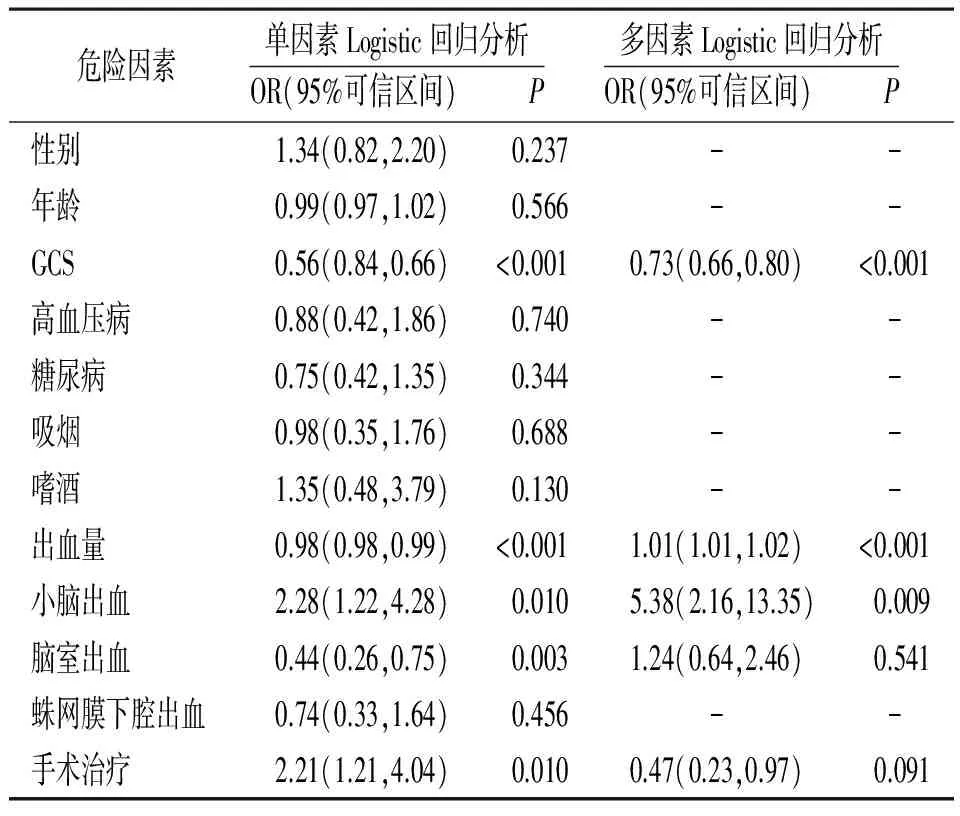
表2 自发性脑出血患者入院30 d内死亡的危险因素分析
注:GCS为格拉斯哥昏迷评分
3 讨论
自发性脑出血是一种常见的、致死性较高的中老年疾病,死亡的主要时间段为入院30 d内[5-8]。近年虽然手术等治疗方法不断改善,但自发性脑出血的临床病死率无明显下降[9-10]。早期识别自发性脑出血患者入院30 d内死亡的危险因素,对加强这类患者的救治具有重要临床意义。Bakhshayesh等[3]2014年对98例自发性脑出血院内死亡的危险因素进行研究,结果显示年龄增大、糖尿病、美国国立卫生研究院卒中量表(NIHSS)评分增加、大血肿和血肿周围水肿是自发性脑出血患者院内死亡的危险因素。2011年Stein等[8]研究显示脑室出血和脑积水分级在预测自发性脑出血患者入院30 d内死亡中具有较好的临床应用价值。本研究结果与Bakhshayesh等[3]和Stein等[8]的研究结果不同,本研究单因素和多因素Logistic回归分析显示GCS、出血量和小脑出血是自发性脑出血患者入院30 d内死亡的独立危险因素。另外,本研究还同时观察了年龄、GCS和出血量预测自发性脑出血患者30 d内死亡的临床价值,结果发现GCS和出血量在预测自发性脑出血患者30 d内死亡中具有良好价值。相比较其他相关研究,本研究观察指标更多、统计方法更全面,且目前国内尚无相关研究,因此具有一定临床价值和创新性。
GCS根据睁眼反应、语言反应和肢体运动等3个方面对患者进行评分,最高为15分,最低为0分,得分越低表明患者病情越严重[11]。有学者对脑创伤患者进行研究,结果显示随着GCS降低,患者病死率显著增高[12]。说明GCS可以较为客观地反映脑创伤患者临床情况,且评分相对简单、快捷,有利于临床应用。出血量是造成脑出血患者颅内压增高的主要因素,出血量越大,颅内压越高,而颅内压增高是导致脑出血患者死亡的主要原因[13-14]。Mac Laughlin等[15]和Yuan等[16]研究均显示监测患者颅内压,防止颅内压过高,有助于降低脑创伤患者院内病死率。小脑出血可表现为小脑占位性病变,大量出血时可导致颅内压增高,进而造成昏迷,最终可导致患者枕大孔疝而死亡,与基底节等部位出血比较,更容易致残和致死[17-18]。
综上所述,GCS、出血量和小脑出血是自发性脑出血患者入院30 d内死亡的独立危险因素。
[1] Hu P, Zhao X Q, Hu B,etal. Spontaneous intracerebral hemorrhage in a pediatric patient with nephrotic syndrome[J].J Clin Hypertens (Greenwich), 2014,16(3):236-237.
[2] Specogna A V, Patten S B, Turin T C,etal. Cost of spontaneous intracerebral hemorrhage in Canada during 1 decade[J].Stroke, 2014,45(1):284-286.
[3] Bakhshayesh B, Hosseininezhad M, Seyed Saadat S M,etal. Predicting in-hospital mortality in Iranian patients with spontaneous intracerebral hemorrhage[J].Iran J Neurol, 2014,13(4):231-236.
[4] Stein M, Hamann G F, Misselwitz B,etal. In-hospital mortality and complication rates in surgically and conservatively treated patients with spontaneous intracerebral hemorrhage in central europe: a population-based study[J].World Neurosurg, 2016,88(5):306-310.
[5] Chan C L, Ting H W, Huang H T. The incidence, hospital expenditure, and, 30 day and 1 year mortality rates of spontaneous intracerebral hemorrhage in Taiwan[J].J Clin Neurosci, 2014,21(1):91-94.
[6] Hu X, Fang Y, Ye F,etal. Effects of plasma D-dimer levels on early mortality and long-term functional outcome after spontaneous intracerebral hemorrhage[J].J Clin Neurosci, 2014,21(8):1364-1367.
[7] Ziai W C, Siddiqui A A, Ullman N,etal. Early therapy intensity level (til) predicts mortality in spontaneous intracerebral hemorrhage[J].Neurocrit Care, 2015,23(2):188-197.
[8] Stein M, Luecke M, Preuss M,etal. The prediction of 30-day mortality and functional outcome in spontaneous intracerebral hemorrhage with secondary ventricular hemorrhage: a score comparison[J].Acta Neurochir Suppl, 2011,112(34):9-11.
[9] 李艳成,黄流清,彭华,等.自发性脑出血急性期白细胞计数与近期预后的相关性分析[J].临床军医杂志,2010,38(2):243-245.
[10]蔚永运.栓塞术治疗儿童脑动静脉畸形1例报道[J].武警后勤学院学报·医学版,2014,23(1):58-59.
[11]Hong J, Rubino S, Lollis S S. Prehospital glasgow coma score predicts emergent intervention following helicopter transfer for spontaneous subarachnoid hemorrhage[J].World Neurosurg, 2016,87(12):422-430.
[12]Majdan M, Steyerberg E W, Nieboer D,etal. Glasgow coma scale motor score and pupillary reaction to predict six-month mortality in patients with traumatic brain injury: comparison of field and admission assessment[J].J Neurotrauma, 2015,32(2):101-108.
[13]Masquere P, Bonneville F, Geeraerts T. Optic nerve sheath diameter on initial brain CT, raised intracranial pressure and mortality after severe TBI: an interesting link needing confirmation[J].Crit Care, 2013,17(3):151.
[14]Dawes A J, Sacks G D, Cryer H G,etal. Intracranial pressure monitoring and inpatient mortality in severe traumatic brain injury: A propensity score-matched analysis[J].J Trauma Acute Care Surg, 2015,78(3):492-501.
[15]Mac Laughlin B W, Plurad D S, Sheppard W,etal. The impact of intracranial pressure monitoring on mortality after severe traumatic brain injury[J].Am J Surg, 2015,210(6):1082-1087.
[16]Yuan Q, Wu X, Sun Y,etal. Impact of intracranial pressure monitoring on mortality in patients with traumatic brain injury: a systematic review and meta-analysis[J].J Neurosurg, 2015,122(3):574-587.
[17]Chang C Y, Lin C Y, Chen L C,etal. The predictor of mortality within six-months in patients with spontaneous cerebellar hemorrhage: a retrospective study[J].PLoS One, 2015,10(7):123-129.
[18]Wu Y T, Li T Y, Chiang S L,etal. Predictors of first-week mortality in patients with acute spontaneous cerebellar hemorrhage[J].Cerebellum, 2013,12(2):165-170.
Analysis of Risk Factors of Death within 30 Days after Admission in Patients with Spontaneous Intracerebral Hemorrhage
SHI Hai-yinga, ZHANG Qianga, WANG Xue-jinga, HAO Lin-junb
(a. Medical Examination Center, b. Emergency Center, Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010050, China)
Objective To investigate risk factors of death within 30 days after admission in patients with spontaneous intracerebral hemorrhage. Methods A total of 342 patients with spontaneous intracerebral hemorrhage admitted during January 2011 and January 2016 were divided into death group (n=86) and survival group (n=256) according to whether or not death within 30 days after admission. Mainly clinical characteristics were observed in two groups. The age was analyzed using the area under the receiver operating characteristics (ROC) curve, and Glasgow coma scale (GCS) score and bleeding volume within 30 days after admission in patients with spontaneous intracerebral hemorrhage were used to predict death, and the risk factors of death within 30 days after admission in patients with spontaneous intracerebral hemorrhage were analyzed using single factor and multiple factors logistic regression analysis. Results Compared with those in survival group, in death group, GCS score was significantly lower; bleeding volume was significantly more; incidence rate of basal ganglia hemorrhage was significantly lower; incidence rates of cerebellar hemorrhage and combination of intraventricular hemorrhage were significantly higher; therapy rate of surgery was lower ((P<0.05). Analysis of the area under the ROC curve showed that GCS and the bleeding volume had a certain clinical value in prediction of death within 30 days after admission in patients with spontaneous intracerebral hemorrhage (P<0.001). Single factor and multiple factors logistic regression analysis showed that CGS, bleeding volume and cerebellar hemorrhage were the independent risk factors of death within 30 days after admission in patients with spontaneous intracerebral hemorrhage. Conclusion GSC, the bleeding volume and cerebellar hemorrhage are the independent risk factors of death within 30 days after admission in patients with spontaneous intracerebral hemorrhage.
Cerebral hemorrhage; Death; Risk factors
内蒙古自治区自然科学基金项目(2016LH0820)
010050 呼和浩特,内蒙古医科大学附属医院体检中心(石海英、张强、王学静),急救中心(郝林军)
R743.34
A
1002-3429(2017)08-0083-04
10.3969/j.issn.1002-3429.2017.08.025
2017-05-24 修回时间:2017-06-18)

