肾组织内皮素受体A、B在老年糖尿病肾病发展中的作用研究
何华妮
(海南省琼海市人民医院 肾内科,海南 琼海 571400)
肾组织内皮素受体A、B在老年糖尿病肾病发展中的作用研究
何华妮
(海南省琼海市人民医院 肾内科,海南 琼海 571400)
目的探讨肾组织中内皮素受体A、B(ETAR、ETBR)表达变化在老年糖尿病肾病发展中的作用。方法选取2015年1月-2016年6月该院收治的糖尿病肾病老年患者34例,根据糖尿病肾病病理分型分为:糖尿病肾病Ⅰ级(D1组10例),Ⅱ级(D2组12例),Ⅲ级(D3组12例);选取同期在该院行肾肿瘤切除术后远离肾肿瘤的正常组织为对照组(10例)。免疫组织化学检测ETAR、ETBR的表达量;免疫荧光双染法定位ETAR、ETBR在肾组织的分布部位。收集生化检测指标,计算肾小球硬化率,进行相关性分析。结果D3组尿蛋白水平高于D2和D1组,差异有统计学意义(P<0.05);D3组肾小球滤过率(GFR)和白蛋白(Alb)与D1组比较差异有统计学意义(P<0.05);D3组和D2组肾小球硬化率均高于D1组,差异有统计学意义(P<0.05)。糖尿病肾病各组ETAR、ETBR表达量均高于对照组,差异有统计学意义(P<0.05);对照组ETAR表达量少于ETBR,随着病情加重糖尿病肾病患者肾组织中ETAR表达量逐渐增加,组间比较差异有统计学意义(P<0.05);D2组ETBR表达量最高,与D1组和D3组比较差异无统计学意义(P>0.05);ETAR/ETBR在各组比较差异有统计学意义(P<0.05)。ETAR在肾小管近端和远端均存在表达,ETBR主要表达于肾小管近端。糖尿病肾病患者肾组织中ETAR表达量与病程、尿蛋白水平、肾小球硬化率(ROG)呈正相关;ETBR表达量与病程呈负相关;ETAR/ETBR比值与病程、尿蛋白水平及ROG呈正相关,与Alb、GFR呈负相关。结论老年糖尿病患者肾组织中ETAR、ETBR表达量增加,ETAR/ETBR值倒置与病情发展呈正相关。
糖尿病肾病;肾组织;内皮素受体;老年人
Abstract:ObjectiveTo investigate the endothelin receptor A,B (ETAR,ETBR)expression in renal tissue of the development in elder diabetic nephropathy.MethodsFrom January 2015 to June 2016,34 elderly patients with diabetic nephropathy in our hospital were divided into 3 groups according to pathological type:10 cases of group D1(12 cases),grade D2 group(12 cases),grade D3 group.Patients underwent renal tumor resection from renal tumors in our hospital as the control group (10 cases).The expressions of ETAR and ETBR were detected by immunohistochemistry.The location of ETAR and ETBR in renal tissue was detected by immunofluorescence double staining method.Biochemical detection indexes were collected to calculate the rate of glomerular sclerosis,and the correlation was analyzed.ResultsThe urine protein level of D3 group was significantly higher than that of D2 and D1 group,the difference was statistically significant (P<0.05).Glomerular filtration rate(GFR)and albumin(Alb)had significant difference between group D3 and D1(P<0.05).D3 group and D2 group glomerular sclerosis rate were significantly higher than that in D1 group,thedifference had statistical difference (P<0.05).The expression of ETAR and ETBR in diabetic nephropathy group were significantly higher than the control group,the difference was statistically significant(P<0.05).The expression of ETAR was less than ETBR in the control group,with the aggravation of increased expression of ETAR in renal tissue of diabetic nephropathy patients,the differences between groups were statistically significant(P<0.05).The expression of ETBR in D2 group was the highest,and no statistically significant differences between D1 group and D3 group (P>0.05).ETAR/ETBR in each group had statistically significant difference(P<0.05).ETAR was expressed in proximal and distal renal proximal tubule.ETBR was mainly expressed in proximal tubule.The expression of ETAR in renal tissue of patients with diabetic nephropathy and duration,urinary protein level and ROG were positively correlated.The expression of ETBR was negatively related to the amount and duration.ETAR/ETBR ratio and the course of disease,urinary protein level,ROG were positively correlated,negatively correlated with Alb,GFR.ConclusionsThe expression of ETAR and ETBR in the renal tissues of the elderly patients with diabetes mellitus are significantly increased,and the inversion of ETAR/ETBR value is positively correlated with the development of the disease.
Keywords:diabetic nephropathy;renal tissue;endothelin receptor;elder
糖尿病肾病多发于老年人群,是导致糖尿病患者死亡的主要并发症之一[1]。研究发现,糖尿病肾病患者血浆和尿液中内皮素1(endothelin-1,ET-1)含量增加并参与了病情的发展,ET-1主要通过内皮素受体 A(endothelin type a receptor,ETAR)、内皮素受体 B(endothelin type b receptor,ETBR)2种受体亚型发挥作用[2-3]。相关研究[4]显示,正常人肾脏ETAR与ETBR的比值为1∶2,但糖尿病肾病患者肾组织ETAR和ETBR的变化仍处在动物实验层面,且结论存在争议[5-7]。本研究通过观察不同糖尿病肾病时期老年患者肾组织中ETAR和ETBR表达变化,探讨其与老年糖尿病发展的关系。
1 资料与方法
1.1 一般资料
选取2015年1月-2016年6月本院收治的糖尿病肾病老年患者34例。肾活检前均告知患者必要性和危险性,签署知情同意书;排除合并继发性肾脏病变、心力衰竭及严重感染的患者。其中,男性25例,女性 11例;年龄 60~79岁,平均(64.91±9.35)岁。根据美国肾病学会2010年颁布的糖尿病肾病病理分型标准,分为糖尿病肾病Ⅰ级(D1组10例),Ⅱ级(D2组12例),Ⅲ级(D3组12例)。选取同期在本院行肾肿瘤切除术后距肾肿瘤>3 cm的组织,苏木精 - 伊红染色法(hematoxylin-eosin staining,HE)染色后显微镜下观察为形态正常的肾组织为对照组(10例)。其中,男性7例,女性3例;年龄60~76岁,平均(66.08±11.70)岁。糖尿病肾病患者与对照组患者之间性别构成、年龄比较差异无统计学意义(P>0.05)。
1.2 方法
1.2.1 肾病理检查 入选患者进行肾组织光学显微镜、免疫荧光及电子显微镜检查,其中,光学显微镜检查包括:HE染色;PAS染色法(periodic acid-schiff stain,PAS);正六胺银染色法 (aeriodic acid-silver methe-namine,PASM-Masson) 染色;Masson 三色染色。计算肾小球硬化率(Glomerular sclerosis rate,ROG)。经本科与超声科协作进行肾活检组织穿刺,将标本初步处理后送上级医院或广州金域医学检验中心进一步检查及处理。
1.2.2 免疫组织化学检测 取肾组织石蜡包块,二甲苯脱蜡,酒精梯度脱水,3%过氧化氢37℃孵育15min,磷酸盐缓冲液冲洗3次;修复抗原,羊血清工作液封闭20 min,分别滴加ETAR、ETBR多克隆抗体(上海研谨生物科技有限公司,1∶1 000稀释),4℃冷藏过夜,磷酸盐缓冲液冲洗3次,滴加生物素标记的二抗,37℃孵育60 min,磷酸盐缓冲液洗净;滴加辣根过氧化物酶(horse radish peroxidase,HRP)标记的链霉素卵白素工作液,37℃孵育60 min,二氨基联苯胺(Diaminobenzidine,DAB)染色,蒸馏水洗净后苏木素复染,脱水、透明、干燥及封片,高倍光镜视野下观察胞质为棕黄色的为阳性,进行半定量分析;采用Image pro plus 6.0软件测定ETAR、ETBR表达量。
1.2.3 免疫荧光双染法 肾组织制作2 μm冷冻切片,采用直接免疫荧光法和间接免疫荧光法,共聚焦显微镜下观察染色结果。近端和远端肾小管的蛋白标志物分别为LTL、THP(上海玉博生物科技有限公司),集合管蛋白标志物为DBA(上海浩然生物技术有限公司),按试剂盒说明书进行操作。
1.3 统计学方法
数据分析采用SPSS 14.0统计软件,计量资料以均数±标准差(±s)表示,用方差分析,两两比较用t检验;回归分析用Pearson法,P<0.05为差异有统计学意义。
2 结果
2.1 生化检测结果和肾小球硬化率
经单因素方差分析,各组尿蛋白、肾小球滤过率(glomerular filtration rate,GFR)、白蛋白(Albumin,Alb)、肾小球硬化率(Glomerular sclerosis rate,ROG)间差异有统计学意义(P<0.05),各组尿蛋白水平差异有统计学意义;进一步两两比较显示,D3组尿蛋白高于D2和D1组,差异有统计学意义(P<0.05);D3组GFR、Alb均低于D2和D1组,差异有统计学意义(P<0.05);D3组和D2组ROG高于D1组,差异有统计学意义(P<0.05)。糖尿病肾病各组间糖化血红蛋白(HbA1C)、血清肌酐(serum creatinine,Scr)水平比较差异无统计学意义P>0.05)。见表1。
2.2 免疫组织化学检测结果
经单因素方差分析,各组ETAR、ETBR表达量比较差异有统计学意义(P<0.05),各组ETAR、ETBR表达量有差异;进一步两两比较显示,糖尿病肾病各组ETAR、ETBR表达量高于对照组,差异有统计学意义(P<0.05);对照组ETAR表达量少于ETBR,随着病情加重糖尿病肾病患者肾组织中ETAR表达量逐渐增加,组间比较差异有统计学意义(P<0.05);D2组ETBR表达量最高,与D1组和D3组比较差异无统计学意义(P>0.05);ETAR/ETBR在各组比较差异有统计学意义(P<0.05)。见表2和图1。
表1 各组患者生化检测结果和肾小球硬化率比较 (±s)

表1 各组患者生化检测结果和肾小球硬化率比较 (±s)
注:1)与 D1 组比较,P<0.05;2)与 D2 组比较,P<0.05
组别ROG/%对照组 0.04±0.02 4.21±0.52 115.62±3.78 39.96±6.15 59.71±10.05 0.50±0.11 D1 组 1.57±0.35 7.52±1.67 104.05±7.43 39.02±5.36 86.63±4.93 2.11±1.95 D2 组 2.51±0.83 7.28±1.31 88.19±22.59 33.38±8.09 83.85±6.79 13.80±5.161)D3 组 5.17±2.661)2) 7.60±1.69 68.27±26.131)2) 31.89±9.771) 93.05±6.19 18.63± 15.541)F值 4.068 0.826 8.339 6.350 0.995 10.985P值 0.035 0.195 0.005 0.018 0.082 0.001尿蛋白/(g/d)HbA1C/%GFR Alb/(g/L)Scr/(μmol/L)
2.3 糖尿病肾病患者免疫荧光双染色结果
以LTL为近端肾小管标志物,4',6-二脒基-2-苯基吲哚(4',6-diamidino-2-phenylindole,DAPI)为蓝色荧光染料,Merge为蓝色与绿色染料混合染色结果(见图2)。ETAR在肾小管近端和远端存在表达,ETBR主要表达于肾小管近端。
2.4 相关性分析
单因素相关性分析显示,糖尿病肾病患者肾组织中ETAR表达量与病程、尿蛋白水平及ROG呈正相关;ETBR表达量与病程呈负相关;ETAR/ETBR比值与病程和尿蛋白水平、ROG呈正相关,与Alb、GFR呈负相关。见表3。
表2 各组肾小管ETAR和ETBR表达量 (±s)
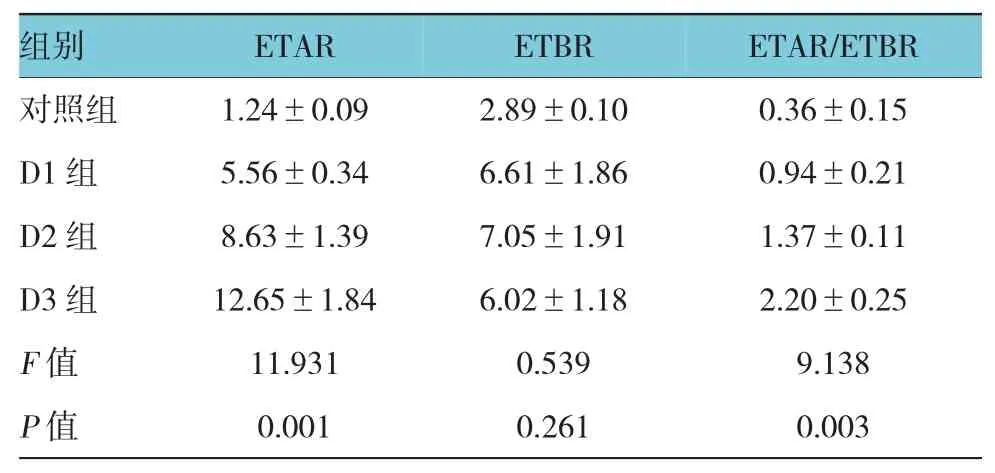
表2 各组肾小管ETAR和ETBR表达量 (±s)
组别ETAR/ETBR对照组 1.24±0.09 2.89±0.10 0.36±0.15 D1 组 5.56±0.34 6.61±1.86 0.94±0.21 D2 组 8.63±1.39 7.05±1.91 1.37±0.11 D3 组 12.65±1.84 6.02±1.18 2.20±0.25F值 11.931 0.539 9.138P值 0.001 0.261 0.003 ETAR ETBR


图1 各组肾小管ETAR和ETBR染色结果 (免疫组织化学×400)
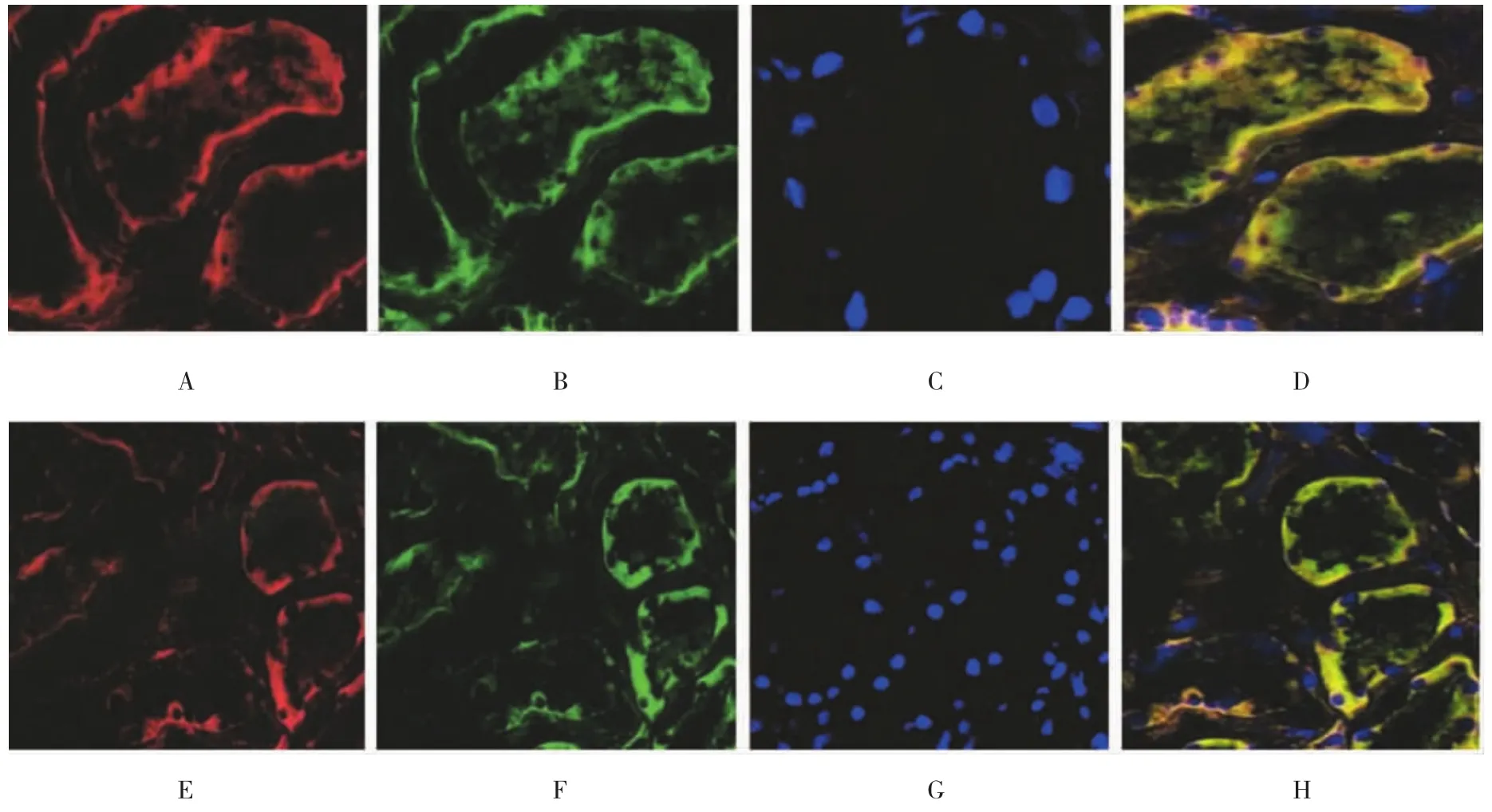
图2 糖尿病肾病患者肾小管ETAR和ETBR双染色结果 (免疫荧光×400)

表3 ETAR、ETBR影响因素相关性分析
3 讨论
ET-1与ETAR结合后可诱导炎症反应、血管收缩及细胞增殖[8-10],与ETBR结合后可介导内皮素浓度相关的NO释放[11],促进循环中ET-1清除和水钠排泄,起到舒张血管、利尿降压的作用[12-13]。本研究显示,人正常肾组织中多表达于肾小管,肾小球中无表达;糖尿病肾病肾组织中ETAR、ETBR在肾小管表达水平提升,肾小球中也有表达。免疫荧光双染法显示,肾组织中皮质内部集合管、近曲小管和远端小管中多分布ETAR;近端小管中多分布ETBR。本研究中收集人肾组织时多为肾皮质部分,只有少量髓质,因此无法得到人肾脏髓质和集合系统的分布情况。
本研究显示,人正常肾组织中ETAR表达量低于ETBR,糖尿病肾病早期肾组织中ETAR和ETBR表达水平均提升,随着病情进展ETAR表达水平高于ETBR,在糖尿病肾病Ⅲ级时ETAR与ETBR的比值达到2∶1。说明ET系统在糖尿病肾病发展中发挥作用,其机制可能与糖尿病肾病患者血管内皮功能受损有关。当肾脏局部ET-1分泌量增加时,其相应的2个受体含量也存在改变,在病情早期ETBR可竞争性抑制ETAR与ET-1结合,扩张血管,保护肾组织;随病情发展ETBR分泌不足,肾组织损伤加重。相关性研究显示,ETAR表达水平与病程、尿蛋白量、ROG呈正相关,ETBR与病程呈负相关,与其他两项无相关性,提示ETAR在糖尿病肾病进展中发挥重要作用;ETAR与ETBR的比值异常与病程、ROG、尿蛋白量、GFR有相关性,说明在糖尿病肾病发展中的作用不可忽视。
综上所述,糖尿病可激活内皮素系统,肾脏组织中持续高表达ETAR及ETAR/ETBR比值异常参与糖尿病肾病的发生、发展。本研究可为干预内皮素途径治疗糖尿病肾病提供新的理论基础。
[1]ZANATTA C M,VERIONESE F V,DASILVALORETO M,et al.Endothelin-1 and endothelin a receptor immunoreactivity is increased in patients with diabetic nephropathy[J].Renal Failure,2012,34(3):308-315.
[2]WATSON A M,LI J,SCHUMACHER C,et al.The endothelin receptor antagonist avosentan ameliorates nephropathy and atherosclerosis in diabetic apolipoprotein E knockout mice[J].Diabetologia,2010,53(1):192-203.
[3]ANDRESS D L,COLL B,PRITCHETT Y,et al.Clinical efficacy of the selective endothelin A receptor antagonist,atrasentan,in patients with diabetes and chronic kidney disease (CKD)[J].Life Sciences,2012,91(13/14):739-742.
[4]YUAN W M,LI Y,WANG J,et al.Endothelin-receptor antagonists for diabetic nephropathy:a meta-analysis[J].Nephrology,2015,20(7):459-466.
[5]SALEH M A,POLLOCK J S,POLLOCK D M,et al.Distinct actions of endothelin A selective versus combined endothelin A/B receptor antagonists in early diabetic kidney disease[J].Journal of Pharmacology&Experimental Therapeutics,2011,338(1):263-270.
[6]RITZ E,WENZEL R R.Endothelin antagonist as add-on treatment for proteinuria in diabetic nephropathy:is there light at the end ofthe tunnel[J].Journalofthe American Society of Nephrology Jasn,2011,22(4):593-595.
[7]KOHAN D E,BARTON M.Endothelin and endothelin antagonists in chronic kidney disease[J].Kidney International,2014,86(5):896-904.
[8]HU C,CONG X D,DAI D Z,et al.Argirein alleviates diabetic nephropathy through attenuating NADPH oxidase,Cx43,and PERK in renaltissue[J].Naunyn-Schmiedeberg'sArchivesof Pharmacology,2011,383(3):309-319.
[9]GRAY S P,JANDELEIT-DAHM K.The pathobiology of diabetic vascular complications-cardiovascular and kidney disease[J].Journal of Molecular Medicine,2014,92(5):441-452.
[10]ABDEL-RAHMAN E M,SAADULLA L,REEVES W B,et al.Therapeutic modalities in diabetic nephropathy:standard and emerging approaches[J].Journal of General Internal Medicine,2012,27(4):458-468.
[11]MANN J F,GREEN D,JAMERSON K,et al.Avosentan for overt diabetic nephropathy[J].Journal of the American Society of Nephrology Jasn,2010,21(3):527-535.
[12]TURGUT F,BOLTON W K.Potential new therapeutic agents for diabetic kidney disease[J].American Journal of Kidney Diseases,2010,55(5):928-940.
[13]REICHETZEDER C,TSUPRYKOV O,HOCHER B,et al.Endothelin receptor antagonists in clinical research-Lessons learned from preclinical and clinical kidney studies[J].Life Sciences,2014,118(2):141-148.
ETAR and ETBR receptor subtypes in development of diabetic nephropathy in elderly
Hua-ni He
(Department nephrology,Qionghai People's Hospital,Qionghai,Hainan 571400,China)
R323.6
A
10.3969/j.issn.1005-8982.2017.15.009
1005-8982(2017)15-0042-05
2016-12-26