地佐辛复合不同浓度左布比卡因在臂丛神经阻滞中的效果观察
曹菁
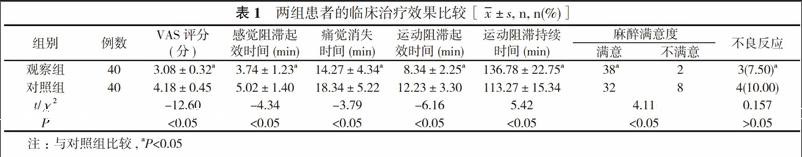
【摘要】 目的 比較地佐辛复合不同浓度左布比卡因在臂丛神经阻滞中的效果, 探讨合适的麻醉方法。方法 80例行上肢手术患者, 采用随机双盲分为观察组和对照组, 各40例。两组患者均常规臂丛神经阻滞准备, 观察组患者应用0.25%左布比卡因30 ml+地佐辛2 mg;对照组患者应用0.375%左布比卡因30 ml+地佐辛2 mg。观察比较两组患者的疼痛视觉模拟评分法(VAS)评分、麻醉效果、麻醉满意程度及药物不良反应。结果 观察组患者的VAS评分为(3.08±0.32)分, 低于对照组的(4.18±0.45)分, 差异具有统计学意义(P<0.05)。观察组患者的感觉阻滞起效时间(3.74±1.23)min、痛觉消失时间(14.27±4.34)min、运动阻滞起效时间(8.34±2.25)min, 均短于对照组的(5.02±1.40)、(18.34±5.22)、(12.23±3.30)min, 差异均具有统计学意义(P<0.05)。观察组患者的运动阻滞持续时间为(136.78±22.75)min, 长于对照组的(113.27±15.34)min, 差异具有统计学意义(P<0.05)。观察组患者中麻醉满意38例(95.00%)高于对照组的32例(80.00%), 差异具有统计学意义(P<0.05)。两组患者的药物不良反应发生率比较差异无统计学意义(7.50% VS 10.00%, P>0.05)。两组患者麻醉期间及麻醉后生命体征均稳定, 所有患者无局麻药中毒反应、膈神经或喉返神经阻滞等发生。结论 0.375%左布比卡因和0.25%左布比卡因配伍地佐辛用于肌间沟臂丛神经阻滞, 均获得满意的效果, 且随着左布比卡因药物浓度的增加, 运动阻滞程度的增加, 产生更强的镇痛效果, 值得临床应用。
【关键词】 地佐辛;左布比卡因;浓度;臂丛神经阻滞
DOI:10.14163/j.cnki.11-5547/r.2016.36.010
【Abstract】 Objective To compare effects by dezocine combined with different concentrations of levobupivacaine in brachial plexus nerve block, and to investigate appropriate measure in anesthesia. Methods A total of 80 patients receiving upper limb surgery were divided by randomized double-blind method into observation group and control group, with 40 cases in each group. Both groups received conventional preparation for brachial plexus nerve block. The observation group received 30 ml of 0.25% levobupivacaine + 2 mg of dezocine. The control group received 30 ml of 0.375% levobupivacaine + 2 mg of dezocine. Observation was made on visual analogue scale (VAS) score, anesthetic effect, anesthetic satisfaction and adverse drug reactions between the two groups. Results The observation group had lower VAS score as (3.08±0.32) points than (4.18±0.45) points in the control group, and the difference had statistical significance (P<0.05). The observation group had feeling block beginning time as (3.74±1.23) min, pain disappearance time as (14.27±4.34) min, and motor block beginning time as (8.34±2.25) min, which were all shorter than (5.02±1.40), (18.34±5.22) and (12.23±3.30) min in the control group, and their differences all had statistical significance (P<0.05). The observation group had more anesthetic satisfaction cases as 38 cases (95.00%) than 32 cases (80.00%) in the control group, and the difference had statistical significance (P<0.05). There was no statistically significant difference of incidence of adverse reactions between the two groups (7.50% VS 10.00%, P>0.05). Both groups had stable vital signs during and after anesthesia, and there was no local anesthesia drug poisoning reactions, phrenic nerve block or recurrent laryngeal nerve block in any case. Conclusion Both of 0.375% levobupivacaine and 0.25% levobupivacaine, combining with dezocine, provide satisfactory effects in interscalene brachial plexus nerve block. Increasing in concentration of levobupivacaine leads to enhanced motor block degree and intensified analgesic effect. This method is worth clinical application.