qSOFA评分在灾害创伤患者早期脓毒症中的诊断效能
胡 盼,刘 蕾,唐 昊,何海燕,胡艳红
qSOFA评分在灾害创伤患者早期脓毒症中的诊断效能
胡 盼1,刘 蕾2,唐 昊3,何海燕2,胡艳红1
目的 探讨快速序贯器官功能评分(quick Sequential Organ Failure Assessment, qSOFA)在急诊创伤患者早期脓毒症筛查中的有效性。 方法 选取第三军医大某附属医院2016-08-01至2016-11-30收治的70例急诊创伤患者,采用qSOFA及全身炎性反应综合征(systemic inflammatory response syndrome,SIRS)评分方法筛查脓毒症,根据测评工具的不同将患者分为qSOFA组及SIRS组两组;以2012国际脓毒症指南标准作为诊断脓毒症的“金标准”,计算其诊断灵敏度及特异度,绘制受试者工作特征曲线(receiver operating characteristic curve,ROC)。 结果 70例创伤患者中,qSOFA组共计检出脓毒症46例,其中确诊31例,诊断灵敏度为80.56%,特异度为55.88%;SIRS组共计检出脓毒症47例,其中确诊29例,诊断灵敏度为80.56%,特异度为48.57%。qSOFA组和SIRS组ROC的曲线下面积(area under the curve,AUC)分别为0.71和0.64,曲线下面积比较,差异无统计学意义(P=0.276)。qSOFA组与SIRS组的总住院时间分别为(23.5±8.3)d、(30.1±14.3)d,差异具有统计学意义(P=0.002);qSOFA组与SIRS组的30 d病死率分别为6.5%和12.7%,差异无统计学意义(P=0.504)。 结论 2种测评工具应用于急诊创伤患者脓毒症筛查诊断的准确性无差异,以qSOFA≥2作为急诊创伤患者早期脓毒症筛查工具值得推荐。
快速序贯功能评分;脓毒症;创伤
创伤是导致青壮年死亡的首要原因[1]。近年来,随着自然灾害、人为灾难的急剧增加,创伤患者也逐年增多。而脓毒症是感染、烧/创伤、休克等急危重症患者的严重并发症之一,病情进展迅速,有极高的病死率。虽然随着救治技术的进步,脓毒症患者病死率已显著下降,但仍高达20%[2],因此,脓毒症成为灾难医学研究的热点课题。随着研究者对脓毒症病理生理机制研究的深入,以及脓毒症临床治疗的不断改观,2016年2月美国医学会杂志刊发了由美国重症医学会与欧洲重症医学会共同发布的关于脓毒症新的定义及诊断标准脓毒症3.0[3,4],把脓毒症定义为:宿主对感染的反应失调,导致危及生命的器官功能损害[4,5]。该定义强调感染导致宿主内稳态失衡,需要紧急识别和干预,突出了潜在的器官功能障碍,体现了严重感染引起机体的病理生理学改变,如果仅有感染,而无器官功能损害,就不能诊断为脓毒症,这有助于把无并发症的感染排除在外,便于脓毒症的快速识别和及时救治。同时专家组将脓毒症2.0中的21条诊断指标进行分析,筛选出预测脓毒症患者的指标,结果提取出3个重要指标:呼吸频率(respiratory rate,RR)≥22次/min、格拉斯哥昏迷评分(glasgow coma scale,GCS)≤13分、收缩压(systolic blood pressure,SBP)≤100 mmHg(1 mmHg=0.133 kPa);这3个指标被命名为快速序贯器官衰竭评分(quick Sequential Organ Failure Assessment,qSOFA)[6-8]。有研究显示qSOFA 指标数据更容易获得,且在非重症监护室(院外、急诊科、普通病房)脓毒症患者中的实用性更高[7]。虽然脓毒症3.0 的定义和诊断标准反映了感染导致机体的病理生理损害,但其有效性和可靠性仍需临床实践验证。本研究通过对比qSOFA及全身炎性反应综合征(systemic inflammatory response syndrome,SIRS)两种评分标准在第三军医大某附属医院创伤科收治的急诊创伤患者中早期脓毒症筛查的准确性,分析qSOFA评分在急诊创伤患者早期脓毒症的诊断效能。
1 对象与方法
1.1 对象 选取我院2016-08-01至2016-11-30收治的急诊创伤患者作为研究对象。总共纳入患者70人,其中qSOFA组检出46人,SIRS组检出47人,分别统计检出患者的基本资料(年龄、性别)及临床资料[受伤机制及创伤严重度评分(injury severity score,ISS)、急性生理与慢性健康评分Ⅱ(acute physiology and chronic health evaluation Ⅱ,APACHEⅡ)、GCS评分、SOFA评分]。
1.2 方法 筛查工具:分别采用qSOFA及SIRS评分对入组患者进行评估,根据测评工具的不同将患者分为qSOFA组及SIRS组两组。纳入标准:年龄>18岁;外伤史。排除标准:排除住院期间由于慢性疾病导致器官功能障碍的患者。qSOFA评价指标为:(1)RR≥22次/min;(2)GCS≤13分;(3)SBP≤100 mmHg。每项指标各计1分,≥2分即为阳性检出。SIRS组采用SIRS评分加上临床感染确诊,SIRS组评价指标为:(1)体温>38℃或<36℃;(2)心率>90次/min;(3)白细胞>12×109/L或<4×109/L或幼稚细胞比例超过10%;(4)呼吸频率>20次/min或动脉血气分析动脉血二氧化碳分压(partial pressure of carbon dioxide,PaCO2)<32 mmHg,符合至少两项指标则为阳性检出。
脓毒症诊断“金标准”:2012国际脓毒症指南标准中所定义的脓毒症标准作为诊断脓毒症的确定性标准。
1.3 统计学处理 采用SAS 9.1.3软件进行统计分析。正态分布计量资料采用表示,计量资料的比较采用配对t检验,计数资料的比较采用χ2检验。计算诊断标准的灵敏度和特异度,绘制受试者工作特征曲线(receiver operating characteristic curve,ROC)曲线,曲线下面积(area under the curve,AUC)采用配对比较法,以P<0.05为差异有统计学意义。
2 结 果
2.1 一般资料 两种评分标准纳入患者的基本资料、受伤机制及ISS评分、APACHE II评分、GCS评分、SOFA评分差异无统计学意义(P>0.05,表1)。
2.2 两组诊断脓毒症诊断效能比较 70例创伤患者中,“金标准”诊断脓毒症患者36例,用两种方法分别进行评分和诊断。qSOFA阳性46例,其中脓毒症患者31例;SIRS阳性47例,脓毒症患者29例。qSOFA评分诊断灵敏度为86.11%,特异度为55.88%;SIRS评分诊断灵敏度为85.29%,特异度为48.57%。qSOFA和SIRS评分ROC曲线下面积分别为0.71和0.64,曲线下面积比较,差异无统计学意义(Z=0.470,P=0.276),见表2、图1。
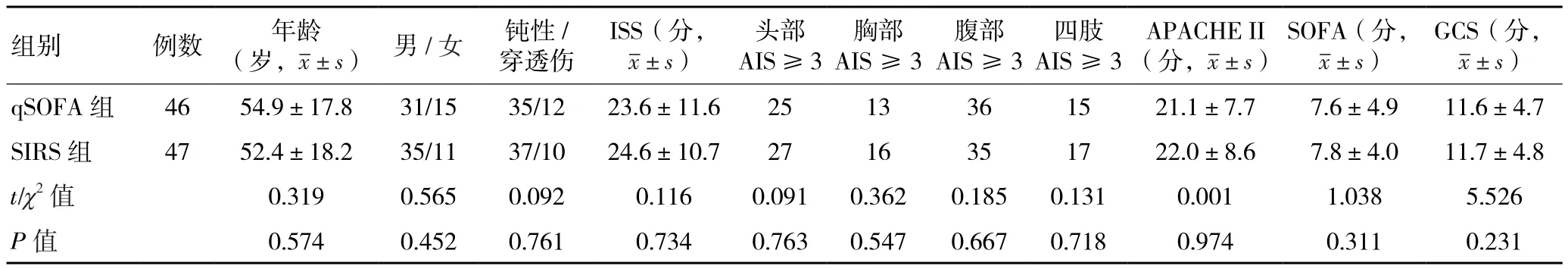
表1 两组急诊创伤患者一般资料比较
2.3 两组急诊创伤患者诊断预后指标的比较 与SIRS组比较,qSOFA组总住院时间明显缩短,差异具有统计学意义[(30.1±14.3)d vs (23.5±8.3)d;t=5.457,P=0.002];qSOFA 组30 d 病死率也有所降低,差异无统计学意义(6.5% vs 12.7%;χ2=1.037,P=0.504)。
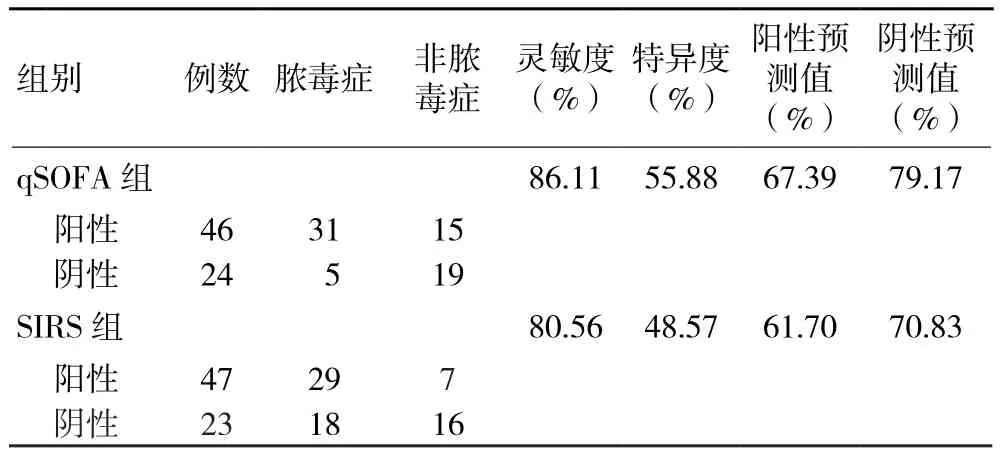
表2 两组急诊创伤患者诊断脓毒症诊断效能比较
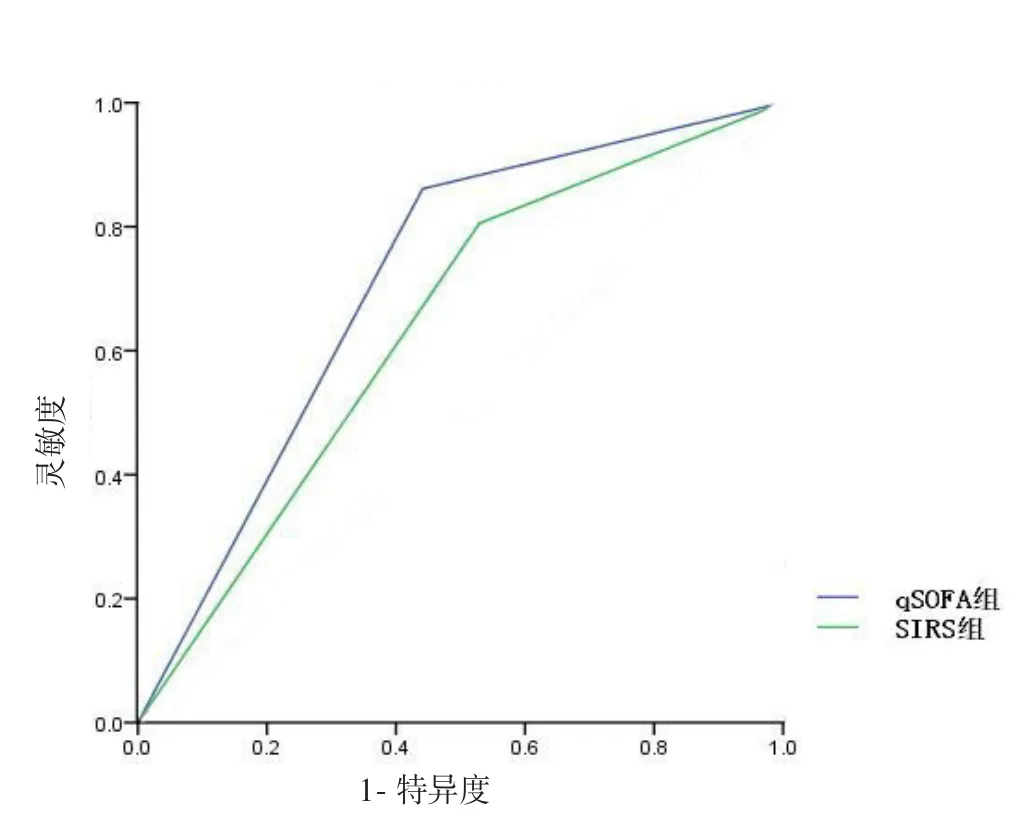
图1 两组急诊创伤患者诊断脓毒症诊断效能的ROC曲线
3 讨 论
灾难医学研究的重点课题之一就是创伤救护,早期识别创伤导致的脓毒症患者,依然是一个难题。1992、2012及2016版脓毒症指南都指出脓毒症的治疗关键是早期识别,尽早诊断及干预,从而降低其病死率[9,10]。目前大多数研究采用1992版指南来定义脓毒症,即采用SIRS作为评分标准,但其过于宽泛,缺乏特异性。因此,最近脓毒症3.0共识会议为了制定一份更好的、更精确的纳入标准,达到提高诊断的灵敏度和特异度的目的[4],筛查了130万份疑似感染病历,通过对比不同的临床指标,证实qSOFA比SIRS更有效、更能准确地预测脓毒症,设立qSOFA目的是为了提高疑似脓毒症的筛查率,以便于早期识别,尽早进行干预[5,11,12]。同时脓毒症3.0共识会议上还指出qSOFA标准有助于重复识别和诊断脓毒症。此外,SIRS标准作为脓毒症的筛查工具首次提出,与qSOFA一样,也应用于疑似感染的患者,目的在于早期识别脓毒症患者[13,16]。然而,对比这两种脓毒症诊断标准,SIRS标准本质上是基于专家共识,而qSOFA标准是基于大样本多元变量分析和确定性分析,比SIRS标准更具有说服力。但是,qSOFA的构想和来源是基于现在和之前的回顾性数据,还应进一步采用前瞻性研究证实工具的有效性以及筛查能力[3,17-19]。因此,本研究通过对临床创伤患者进行4个月的观察,对比了qSOFA及 SIRS评分的诊断效能,但比较差异无统计学意义。基于当前的文献报道及本研究结果,尽管在脓毒症定义方面qSOFA评分还不能替代SIRS评分,但作为脓毒症筛查工作qSOFA及SIRS评分的诊断效能并无显著差异,且qSOFA评分更为简单便捷,更适用于急诊或院前急救等难以获得实验室指标的情况。创伤患者死亡的三高峰曲线提示,后期创伤死亡的主要原因是脓毒症,而早期诊断和治疗是脓毒症救治时效性的关键[1]。qSOFA评分具有简单、易获取的特点,适合创伤患者的早期救治,因此qSOFA评分可以替代SIRS评分作为急诊创伤患者的脓毒症筛查工具[1,2,20]。
在患者预后评估方面,多项研究在关于各种严重程度疑似感染的、大样本前瞻性研究中发现,SIRS是器官功能衰竭和预测死亡的有效指标,但仅有10%的器官功能衰竭与30 d病死率相关[7,10,20];Giamarellos-Bourboulis等[10]发现,SIRS未能有效地预测住院患者或急诊患者的感染,然而SIRS评分标准中的部分内容是来自于临床医师的主观判断,这些评估主要是基于生理学、调查或研究的标准。在纳入了1031例急诊疑似感染患者的研究中,文献[8,14]发现,SIRS评分筛出的患者病死率较高,但是研究者希望SIRS评分标准可排除高血糖和意识状态的改变这两个相关性因素。qSOFA评分的优势在于,床旁筛查有器官功能衰竭或死亡风险的脓毒症患者的数据更容易获得,无需依赖实验室指标,更有利于为灾害性创伤患者提供快速、便捷的床旁诊断标准。笔者认为,尤其在需要及时识别出高危感染患者的急诊科、院外急救和灾难救护现场,以qSOFA≥2作为脓毒症的筛查工具值得推荐。由于本研究为回顾性调查,难免存在信息上的缺陷,期待在今后大数据的研究中进一步改进。
【参考文献】
[1]Sobrino J, Shafi S. Timing and causes of death after injuries [J]. Proc( Bayl Univ Med Cent), 2013, 26(2): 120-123.
[2]Vincent J L, Mira J P, Antonelli M. Sepsis: older and newer concepts [J]. Lancet Respir Med, 2016, 4(3): 237-240. DOI: 10.1016/S2213-2600(15)00522-6.
[3]Singer M, Deutschman C S, Seymour C W, et al. The third international consensus definitions for sepsis and septic shock( sepsis-3) [J]. JAMA, 2016, 315(8): 801-810. DOI: 10.1001/jama.2016.0287.
[4]郭凤梅, 邱海波. 思考与解读Sepsis新定义和诊断标准 [J]. 中华内科杂志, 2016, 55( 6 ): 420-422. DOI: 10.3760/cma.j.issn.0578-1426.2016.06.002.
[5]Deutschman C S. Imprecise medicine: the limitations of sepsis-3 [J]. Crit Care Med, 2016, 44(5): 857. DOI: 10.1097/CCM.0000000000001834.
[6]Williams J M, Greenslade J H, Mckenzie J V, et al. SIRS, qSOFA and organ dysfunction: insights from a prospective database of emergency department patients with infection [J]. Chest, 2017, 151(3): 586-596. DOI: 10.1016/ j.chest.2016.10.057.
[7]Franchini S, Duca A. qSOFA should replace SIRS as the screening tool for sepsis [J]. Crit Care, 2016, 20(1): 409. DOI: 10 .1186/s13054-016-1562-4.
[8]Vincent J L. qSOFA does not replace SIRS in the definition of sepsis [J]. Critical Care, 2016, 20(1): 210. DOI: 10.1186/s13054-016-1389-z.
[9]Deis A, Whiles B, Simpson S. SIRS vs qSofa at presentation in patients with diagnosed severe sepsis and septic shock [J]. Chest, 2016, 150(4): 348A. DOI: 10.1016/ j.chest.2016.08.361.
[10]Giamarellos-Bourboulis E J, Tsaganos T, Tsangaris I, et al. Validation of the new sepsis-3 definitions: proposal for improvement in early risk identification [J]. Clin Microbiol Infect, 2017, 23(2): 104-109. DOI: 10.1016/j.cmi. 2016.11.003.
[11]Huson M A, Kalkman R, Stolp S M, et al. The impact of HIV on presentation and outcome of bacterial sepsis and other causes of acute febrile illness in Gabon [J]. Infection, 2015, 43(4): 1-9. DOI: 10.1007/s15010-015-0753-2.
[12]Grobusch M P, Greub G. Diagnosis of febrile illness in the tropics--how many tests are enough [J]. Travel Med Infect Dis, 2015, 13(1): 98-99. DOI: 10.1016/ j.tmaid.2014.10.017.
[13]Zhang Z, Li Q. Identifying sepsis in clinical database with sepsis-3 definition [J]. Crit Care Med, 2016, 44(11): e1145. DOI: 10.1097/CCM.0000000000001989.
[14]Balk R A, Cerra F B, Knaus W A, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee [J]. Chest, 1992, 101(6): 1644-1655.
[15]Overhaus M, Moore B A, Flynn B A, et al. Biliverdin schützt die intestinale Integrität in der Sepsis [C]// Chirurgisches Forum 2004, 2004: 279-281. DOI: 10. 1007/978-3-642-18547-2_86.
[16]D'Acremont V, Kilowoko M, Kyungu E, et al. Beyond malaria--causes of fever in outpatient Tanzanian children [J]. N Engl J Med, 2014, 370(9): 809-817. DOI: 10.1056/ NEJMoa1214482.
[17]Wang T, Derhovanessian A, De C S, et al. Subsequent infections in survivors of sepsis: epidemiology and outcomes [J]. J Intensive Care Med, 2014, 29(2): 87-95. DOI: 10.1177/0885066612467162.
[18]Motalib S, Dries D J. The sepsis saga: sepsis-3-ready for prime time[J]. Air Med J, 2016, 35(5): 265-267. DOI: 10.1016/j.amj.2016.06.003.
[19]Huson M A, Kalkman R, Grobusch M P, et al. Predictive value of the qSOFA score in patients with suspected infection in a resource limited setting in Gabon [J]. Travel Med Infect Dis, 2017(15): 76-77. DOI: 10.1016/ j.tmaid.2016.10.014.
[20]Whittle J, Walker D. The new international sepsis guidelines( sepsis-3): the central message remains [J]. Br J Hosp Med( Lond), 2016, 77(4): 208. DOI: 10.12968/ hmed.2016.77.4.208.
(2017-02-07收稿 2017-04-06修回)
(本文编辑 罗发菊)
Diagnostic efficacy of qSOFA score in patients with early sepsis after acute trauma
HU Pan1, LIU Lei2, TANG Hao3, HE Haiyan2, and HU Yanhong1. 1. Department of Outpatient, 2. Department of Nursing, 3. Department of Intensive Care Unit, Institute of Field Surgery, Daping Hospital, The Third Military Medical University, Chinese People's Liberation Army, Chongqing 400042, China
LIU Lei, E-mail: ttcrystalma@163.com
Objective This study objective was to investigate the effectiveness of quick Sequential Organ Failure Assessment (qSOFA) in screening for early sepsis in patients following acute trauma. Methods A total sample of 70 patients with acute trauma presented to a hospital affiliated to the Third Military Medical University of PLA from 1st August to the 30th November 2016 were enrolled in this study. The qSOFA score and systemic inflammatory response syndrome (SIRS) were applied to determine the presence of sepsis; the patients were divided into qSOFA group and SIRS group according to the difference in the evaluation tools. The 2012 sepsis guideline was used as the definite standard, the diagnostic sensitivity and specificity of qSOFA and SIRS were analyzed and compared, and then the receiver operating characteristic curve (ROC) was drawn. Results Among the 70 patients with acute trauma, 46 were predicted to have sepsis by qSOFA and 31 were definitively diagnosed; 47 patients were predicted to have sepsis by SIRS, with 29 definitively diagnosed. The diagnostic sensitivity and specificity of qSOFA were 86.11% and 55.88%, respectively. The diagnostic sensitivity and specificity of SIRS were 80.56% and 48.57%, respectively. The area under the curve (AUC) of ROC in qSOFA group and SIRS group were 0.71 and 0.64, respectively. There was no statistically significant difference in the AUC (P=0.276). The length of hospital stay in qSOFA and SIRS groups were (23.5±8.3) days and (30.1±14.3) days respectively, and the difference was statistically significant (P=0.002). The 30 d mortality rates of qSOFA and SIRS groups were 6.5% and 12.7% respectively; there was no statistically significant difference (P=0.504). Conclusions There is no difference in the sensitivity and specificity between qSOFA and SIRS scores in the diagnosis of sepsis after acute trauma. The qSOFA score can be used as a screening tool for early sepsis in patients with acute trauma. It is recommended to use qSOFA ≥ 2 as an early predictor of sepsis for emergency trauma patients.
qSOFA; sepsis; trauma
R641;R459.7
10.13919/j.issn.2095-6274.2017.05.003
400042 重庆,第三军医大学大坪医院野战外科研究所:1. 门诊部,2. 护理部,3. 重症监护室
刘 蕾, E-mail:ttcrystalma@163.com

