颈椎退行性疾病Bryan间盘置换术后椎旁骨化影响因素分析
韩骁,田伟,刘波,何达,吕艳伟,马驰,王晋超
(北京积水潭医院,北京100035)
颈椎退行性疾病Bryan间盘置换术后椎旁骨化影响因素分析
韩骁,田伟,刘波,何达,吕艳伟,马驰,王晋超
(北京积水潭医院,北京100035)
目的 探讨颈椎退行性疾病患者行Bryan间盘置换后节段活动度、假体偏移程度及倾斜角度与椎旁骨化(PO)的关系。方法 选取颈椎退行性疾病行Bryan间盘置换患者76例(手术节段90个),平均随访时间均超过10年。分别于术前、术后3个月、末次随访时拍射X线光片,测量置换节段活动度;末次随访时在冠状位重建CT图像上测量假体偏移程度及假体的倾斜角度,并采用McAfee分型判断末次随访时PO分级。回顾性分析末次随访时发生4级PO的影响因素,假体偏移程度及倾斜角度与PO分级及节段活动度的关系。结果 术前、术后3个月、末次随访时置换节段活动度分别为9.2°±4.7°、8.2°±4.8°、8.7±5.1°,各时间段比较P均>0.05;末次随访时节段活动度与术后3个月时节段活动度呈正相关(r=0.572,P<0.01)。末次随访时冠状位假体偏移程度的中位数为0.61(0~7.08)mm,假体倾斜角度的中位数为0.84°(0.01°~9.79°);末次随访时假体偏移程度与末次随访置换节段活动度呈负相关(r=-0.379,P=0.001)。末次随访时发生4级PO共17个节段(15例)、0~3级PO共73个节段(63例),PO 4级患者手术时年龄大于0~3级患者(P<0.05),术后3个月及随访时置换节段活动度均低于0~3级患者(P均<0.01)。与冠状位假体偏移程度≤3 mm患者比较,>3 mm患者置换节段末次随访PO分级更高、节段活动度更低(P均<0.01)。与冠状位假体倾斜角度≤5°患者比较,>5°患者置换节段末次随访PO分级更高、节段活动度更低(P均<0.05)。结论 颈椎人工间盘置换术术后患者保持早期置换节段活动度,可有效避免4级PO的发生;假体安放偏离中心或在冠状位发生倾斜均会造成远期随访时PO分级更高,并对远期活动度产生影响,尤其避免偏移程度超过3 mm或倾斜程度超过5°。
颈椎退行性疾病;颈椎人工间盘置换术;节段活动度;假体位置;异位骨化;椎旁骨化
颈椎人工间盘置换术(CADR)术后最重要的运动学参数是节段活动度,如果患者术后节段活动度减少或丢失,说明手术效果不佳[1]。研究发现,CADR术后异位骨化是造成节段活动度丧失的主要原因[2]。由于异位骨化与骨赘的形态及好发位置相同[3],且二者对CADR术后患者远期节段活动度的影响相同[4],因此异位骨化亦被描述为“异位骨化或骨赘”,本研究将二者统称为椎旁骨化(PO)。以往研究结果显示,人工间盘假体在矢状面的位置不佳与远期随访PO分级及术后远、近期节段活动度丢失有关[5]。但目前尚未见假体冠状位位置不佳对颈椎运动功能影响的报道。本研究探讨颈椎退行性疾病患者行Bryan间盘置换后节段活动度、假体偏移程度及倾斜角度与PO的关系。
1 临床资料
1.1 基本资料 选取2004年1月~2010年5月北京积水潭医院收治的76例颈椎退行性疾病行Bryan间盘置换术患者,男47例、女29例,年龄26~70岁、平均46.6岁。术前CT及MRI显示拟手术节段存在骨赘和(或)间盘突出,造成脊髓和(或)神经根受压,神经定位症状、体征与影像学相符,拟手术节段≤2个。患者均经过3~6个月正规保守治疗无效,术前JOA评分4~16.5分、中位数14分。76例患者均行Bryan间盘置换术,手术节段90个,单节段62例、双节段14例,C3~44例、C4~521例、C5~650例、C6~715例。手术采用颈部横切口,Smith-Robinson入路,透视定位并切除病变椎间盘,置入Bryan人工间盘假体。术中切除后方增生骨赘及后纵韧带以充分减压,注意保留钩椎关节。术后平均随访时间10.1(5.8~12.7)年。
1.2 治疗效果 ①JOA评分:术前、末次随访时行JOA评分。JOA评分改善率=[(随访评分-术前评分)/(17-术前评分)]×100%。结果显示,术前及末次随访时JOA评分分别为(14.0±3.5)、(16.5±1.9)分,末次随访时JOA改善率为75%。② Odom评分:末次随访时行Odom评分评价整体疗效。Odom评分标准:很好:无颈椎疾病相关症状,正常工作不受限;较好:间断性出现颈椎疾病相关症状,对日常工作无明显影响;一般:症状有改善,但正常生活明显受限;差:症状无改善甚至加重。本组末次随访时Odom评分结果为很好52例(68.4%),较好15例(19.7%),一般8例(10.5%),差1例(1.3%)。③影像学指标:分别于术前、术后3个月、末次随访时拍射中立位及过伸过屈位X线光片。置换节段活动度由过伸过屈位测量得出。使用末次随访时标准的冠状位重建CT图像评价假体位置情况。所选的冠状位重建CT图像在矢状面应平行于手术节段下方椎体的后壁,在轴位应平行于手术节段下方椎体的后壁,并选取通过假体中央的那一层进行测量[6]。于末次随访时在该冠状位图像上测量假体偏移程度及假体倾斜角度,采用McAfee分型[4]选择冠状位假体前部的层面判断PO分级。0级为无骨化;1级为骨化达到,但未超过椎间隙水平;2级为骨化侵入椎间隙水平;3级为骨化与上位椎体间形成桥状连接,但过屈过伸位X光片显示节段仍保持活动;4级为关节融合。所有影像学资料由两位脊柱外科专业医师在医学影像存档和通讯系统(PACS)影像学工作站中分别独立测量,最后定量结果取平均数,定性结果由讨论达成一致。结果显示,本组患者随访期间节段活动度均保持良好,置换节段活动度术前、术后3个月、末次随访时分别为9.2°±4.7°、8.2°±4.8°、8.7±5.1°,各时间段比较P均>0.05;末次随访时与术后3个月时的节段活动度呈正相关(r=0.572,P<0.01)。末次随访时冠状位假体偏移程度的中位数0.61(0~7.08)mm,四分位数间距为2.43 mm;假体倾斜角度的中位数0.84°(0.01°~9.79°),四分位数间距为2.86°。末次随访时假体偏移程度与置换节段活动度呈负相关(r=-0.379,P=0.001),与术前及术后3个月手术节段活动度均无关(P均>0.05)。
1.3 末次随访时PO发生情况及其影响因素 末次随访时发生4级PO共17个节段(15例)、0~3级PO共73个节段(63例),2例双节段置换患者同时存在PO 4级及非4级的节段。末次随访时PO 4级患者手术时年龄大于0~3级患者(P<0.05),术后3个月及随访时置换节段活动度均低于0~3级患者(P均<0.01);PO 4级与0~3级患者术前置换节段活动度比较差异无统计学意义(P>0.05),见表1。Logistic回归分析结果显示,术后3个月手术节段活动度是4级PO发生的影响因素,且为保护因素(OR=0.685,P<0.01),见表2。

表1 末次随访时PO 0~3级与4级患者的基本资料比较±s)
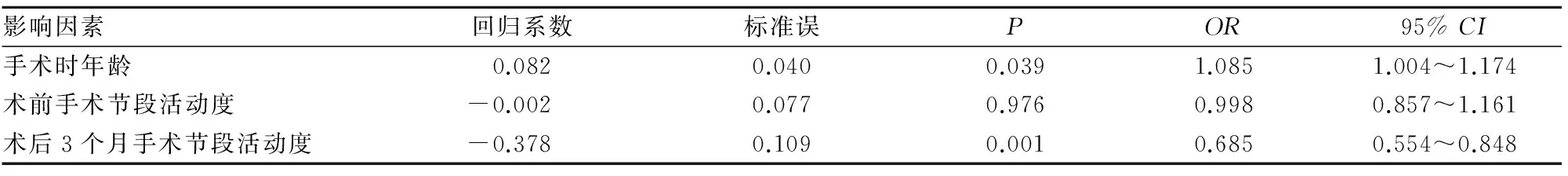
表2 4级PO影响因素的多因素Logistic回归分析结果
1.4 末次随访时假体偏移程度及倾斜角度与PO分级及置换节段活动度的关系 与冠状位假体偏移程度≤3 mm者比较,>3 mm者置换节段PO分级更高、节段活动度更低(P均<0.01)。与冠状位假体倾斜角度≤5°者比较,>5°者置换节段PO分级更高、节段活动度更低(P均<0.05)。见表3、4。

表3 置换节段活动度与假体偏移程度、假体倾斜角度的关系±s)

表4 PO分级与假体偏移程度、假体倾斜角度的关系(节段)
2 讨论
CADR术后节段活动度的变化趋势报道不一[4~8]。提示CADR术后节段活动度能否保持术前水平是一个有争议的话题。本组末次随访置换节段活动度与术前相比无统计学差异,提示CADR术后平均10年节段活动度均保持较好。
根据髋、膝人工关节置换术的经验,假体活动度的保持取决于下列三个因素:一是假体设计因素,如几何特性、材料、活动性等方面;二是患者因素,如年龄、体质量、术前运动状况等;三是手术因素。假体设计方面,不同的假体设计可能造成不同的生物力学特点。Rousseau等[9]研究了球窝型假体术后节段活动状态,发现不同中心位置和不同直径的假体术后节段活动度均无明显差异。Goel等[10]用有限元分析法比较球窝型假体、三明治型假体、弹性假体,发现球窝型假体保留了和术前相似的节段活动度,而另外两型的节段活动度较原始状态有所增加。对于小关节受力的分析表明,弹性假体能更好地模拟原始状态。Kowalczyk等[11]对比了Bryan、Prestige LP、ProDisc-C三种假体,发现前两者在术后1年保留了术前节段活动度,而ProDisc-C则有所增加。患者因素指的是术前患者的自身情况,包括全身条件,如年龄、性别、体质量等;其次为局部条件,对于CADR主要包括术前节段活动度、术前退变程度、术前症状持续时间及严重程度等[1,12]。手术因素则是指术中假体的放置位置、手术类型等,对于CADR 重要的因素包括假体置入深度、假体置入角度、单节段或多节段手术等,亦包括术后康复方面,如颈托佩戴时间等[5]。
在CADR开展早期就已经认识到因为间盘置换术后PO造成节段活动度丧失的问题[2]。高等级PO(3级或4级)的出现会限制置换节段的活动度,从而违背了该手术保持手术节段术前生物力学环境的初衷。Radcliff等[13]研究表明,颈椎间盘置换术后5年仍可保留颈椎屈伸及侧方弯曲的活动度,高等级PO发生率为29.7%。Quan等[14]报道,21例Bryan间盘置换术后随访8年的患者中9例出现高等级PO。Loumeau等[15]发现,CADR术后7年人工间盘组保留了>7°的屈伸角及4.4°侧方活动角,术后均未出现置入人工间盘移位、下沉及椎间隙丢失,高等级PO发生率为59%。4级PO与1~3级PO发生机制不同,其并不是由0~3级PO逐级进展形成[2],并未发生体积较大的椎旁骨赘或骨化灶,而是在钩椎关节直接发生的骨性融合[2]。CADR术后是否发生融合与假体型号较小无关,因为即使假体较小,与钩椎关节处的紧密接触相比在后方上下椎体间仍存在较大距离[2]。本研究单独分析4级PO的影响因素,在评估假体冠状位位置与远期活动度的关系时去掉PO分级为4级的节段。结果显示,末次随访时发生4级PO患者术后3个月节段活动度较低,术后3个月手术节段活动度的保持是避免发生4级PO的保护因素。因此,保持CADR术后节段早期活动度,可避免4级PO的发生。
假体位置的正确安放是CADR成功的保障[6]。假体在冠状面不居中可能导致冠状面失衡,造成关节突关节应力不均,进而影响假体功能。关于假体在冠状位位置正确安放的研究较多,但位置不佳对颈椎运动功能影响的报道较少。本研究结果显示,末次随访时假体偏移程度与手术节段活动度呈负相关,假体偏移程度与术前或术后3个月随访手术节段活动度无关,说明假体是否居中不会影响术后早期节段活动度,但与远期节段活动度有关。本研究根据冠状位假体偏移程度将手术节段分为两组,结果显示假体偏移程度>3 mm组PO分级更高;根据冠状位假体倾斜角度,将手术节段分为两组,结果显示假体倾斜角度>5°组患者PO分级更高;上述结果说明假体安放偏离中心或在冠状位发生倾斜均会造成远期随访时PO分级更高。本研究进一步分析了假体偏移程度及倾斜角度与手术节段远近期活动度的关系,结果显示,假体偏移程度及倾斜角度与术后3个月节段活动度无关,但是偏移程度>3 mm及倾斜角度>5°患者末次随访时手术节段活动度更低;说明假体安放偏离中心或是在冠状位发生倾斜均会造成远期随访时活动度丢失。
综上所述,CADR术后患者保持早期活动度,可以避免4级PO的发生;假体安放偏离中心或在冠状位发生倾斜均会造成远期随访时PO分级更高,并对远期活动度产生影响,临床应避免偏移程度超过3 mm或倾斜程度超过5°。但本研究患者均为长期随访病例,缺乏术前冠状位CT结果,无法判断术前PO分级情况,未进行假体冠状位位置与PO分级进展关系的评估,今后将进一步完善。
[1] Tian W, Han X, Liu B, et al. Clinical and radiographic results of cervical artificial disc arthroplasty over three years′ follow-up cohort study[J]. Chinese Medical Journal, 2010,123(21):2969-2973.
[2] McAfee PC, Cunningham BW, Devine J, et al. Classification of heterotopic ossification (HO) in artificial disk replacement[J]. J Spinal Disord Tech, 2003,16(4):384-389.
[3] Kouyoumdjian P, Bronsard N, Vital JM, et al. Centering of cervical disc replacements[J]. Spine, 2009,34(15):1572-1577.
[4] Sasso RC, Best NM, Metcalf NH, et al. Motion analysis of bryan cervical disc arthroplasty versus anterior discectomy and fusion: results from a prospective, randomized, multicenter, clinical trial[J]. J Spinal Disord Tech, 2008,21(6):393-399.
[5] Park DK, Lin EL, Phillips FM. Index and adjacent level kinematics after cervical disc replacement and anterior fusion: in vivo quantitative radiographic analysis[J]. Spine, 2011,36(9):721-730.
[6] Pickett GE, Rouleau JP, Duggal N. Kinematic analysis of the cervical spine following implantation of an artificial cervical disc[J]. Spine, 2005,30(17):1949-1954.
[7] Kim SW, Shin JH, Arbatin JJ, et al. Effects of a cervical disc prosthesis on maintaining sagittal alignment of the functional spinal unit and overall sagittal balance of the cervical spine[J]. Eur Spine J, 2008,17(1):20-29.
[8] Zhang Z, Gu B, Zhu W, et al. Clinical and radiographic results of Bryan cervical total disc replacement: 4-year outcomes in a prospective study[J]. Arch Orthop Trauma Surg, 2013,133(8):1061-1066.
[9] Rousseau MA, Bonnet X, Skalli W. Influence of the geometry of a ball-and-socket intervertebral prosthesis at the cervical spine: a finite element study[J]. Spine, 2008,33(1):E10-E14.
[10] Goel VK, Faizan A, Palepu V, et al. Parameters that effect spine biomechanics following cervical disc replacement[J]. Eur Spine J, 2012,21(Suppl 5):S688-699.
[11] Kowalczyk I, Lazaro BC, Fink M, et al. Analysis of in vivo kinematics of 3 different cervical devices: Bryan disc, ProDisc-C, and Prestige LP disc[J]. J Neurosurg Spine, 2011,15(6):630-655.
[12] 田伟,韩骁,刘波,等.术前因素对人工颈椎间盘置换术中期疗效的影响[J].中华外科杂志,2010, 48(2): 108-111.
[13] Radcliff K, Coric D, Albert T. Five-year clinical results of cervical total disc replacement compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled, multicenter investigational device exemption clinical trial[J]. J Neurosurg Spine, 2016,25(2):213-224.
[14] Quan GM, Vital JM, Hansen S, et al. Eight-year clinical and radiological follow-up of the bryan cervical disc arthroplasty[J]. Spine, 2011,36(8):639-646.
[15] Loumeau TP, Darden BV, Kesman TJ, et al. A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease (SCDD) following ProDisc-C total disc arthroplasty (TDA) versus anterior cervical discectomy and fusion (ACDF)[J]. Eur Spine J, 2016,25(7):2263-2270.
Influencing factors for paravertebral ossification in patients with cervical degenerative disease after Bryan artificial disc replacement
HANXiao,TIANWei,LIUBo,HEDa,LYUYanwei,MAChi,WANGJinchao
(BeijingJishuitanHospital,Beijing100035,China)
Objective To discuss the relationship of segmental range of motion (ROM), implant deviation and implant tilt with the paravertebral ossification (PO) in patients with cervical degenerative disease after Bryan cervical artificial disc replacement (CADR). Methods A total of 90 Bryan discs which were implanted into 76 patients with cervical degenerative disease were retrospectively analyzed. The average follow-up time was more than 10 years. The segmental ROM was measured by X-ray at the preoperation, 3 months′ follow-up and the last follow-up. We used the coronal reconstruction CT to evaluate the implant deviation and implant tilt at the last follow-up, and determined the grades of PO by McAfee at the last follow-up. We retrospectively analyzed the influence factors of grade 4 PO as well as the relationship of segmental ROM, implant deviation and implant tilt with the grade of PO. Results The segmental ROM at preoperation, 3 months′ follow-up and the last follow-up was 9.2°±4.7°, 8.2°±4.8° and 8.7±5.1° (allP>0.05). The segmental ROM at 3 months′ follow-up and the last follow-up was positively correlated (r=0.572,P<0.01). The median and interquartile range of implant deviation was 0.61 (0-7.08) mm and 0.84 (0.01-9.79)°. The implant tilt was negatively correlated with segmental ROM at the last follow-up (r=-0.379,P=0.001). At the last follow-up there were 17 segments (15 patients) with grade 4 PO and 73 segments (63 patients) with grade 0-3 PO. Patients who had grade 4 PO were older than the patients with the grade 0-3 PO (P<0.05). Patients with the grade 4 PO had less segmental ROM than that of patients with the grade 0-3 PO at the 3 months′ and last follow-up (allP<0.01). The segment whose implant deviation was greater than 3 mm would have a higher PO grade (P<0.01), and less ROM at the last follow-up (allP<0.01). The segment whose implant tilt was greater than 5° would have a higher PO grade (P<0.01), and less ROM at the last follow-up (P<0.05). Conclusions Maintaining the segmental ROM after the early stage of CADR can avoid the grade 4 PO. The implant deviation or implant tilt will cause the higher grade of PO in the long-term follow-up and will influence the long term ROM, and especially we should avoid the implant deviation more than 3 mm or implant tilt more than 5°.
cervical degenerative disease; cervical artificial disc replacement; segmental range of motion; prosthesis positioning; heterotopic ossification; paravertebral ossification
北京市科学技术委员会资助项目(Z161100000516134);北京市医院管理局“青苗”计划专项经费资助(QML20160402)。
韩骁(1981-),男,副主任医师,研究方向为脊柱退行性疾病及创伤的诊断和治疗。E-mail: hanxiaomd@vip.163.com
田伟(1959-),男,主任医师,研究方向为脊柱非融合技术、脊柱外科微创技术和脊柱外科导航技术等。获得国家科技进步二等奖。E-mail: tianweijst@vip.163.com
10.3969/j.issn.1002-266X.2017.04.002
R653
A
1002-266X(2017)04-0013-04
2016-04-23)

