非瓣膜病性心房颤动患者血栓前体蛋白与P选择素水平变化
赵红丽,刘丽敏,张晓丹,周佳萌,王小溪
· 论著 ·
非瓣膜病性心房颤动患者血栓前体蛋白与P选择素水平变化
赵红丽1,刘丽敏1,张晓丹1,周佳萌1,王小溪1
目的 分析非瓣膜病性心房颤动(NVAF)患者血栓前体蛋白(TpP)与P选择素(Ps)水平变化。方法 选择2014年5月~2015年10月于沈阳医学院附属第二医院心血管内科住院治疗NVAF患者206例(NVAF组),男性132例,女性74例,年龄39~79岁。另入选冠状动脉粥样硬化性心脏病(冠心病)(78例)和扩张型心肌病(扩心病)(2例)无心房纤颤(房颤)患者作为对照组(80例)。NVAF组患者依据CHADS2评分分为CHADS2≥2组(87例)及CHADS2<2组(119例);另外NVAF组患者中接诊时可明确AF发作时间者共87例,按AF持续时间分为≥48 h组(59例)及<48 h组(28例);此外NVAF组患者中住院期间可明确区分AF类型者共102例,分为持续性AF组(66例)和阵发性AF组(36例)。收集入选者病例记录的基线资料包括:性别、年龄、左房内径(LAD)、左室射血分数(LVEF)、AF持续时间和类型、CHADS2评分等。应用酶联免疫吸附法测定Ps和TpP水平。结果 NVAF组与对照组年龄、性别构成、合并疾病比例、LAD、LVEF比较,差异无统计学意义(P均>0.05)。NVAF组较对照组TpP、Ps略有升高,但差异无统计学意义(P均>0.05)。与CHADS2<2组比较,CHADS2≥2组年龄增加,合并高血压与糖尿病比例增加,TpP及Ps水平显著升高,差异有统计学意义(P均<0.05)。AF持续时间≥48 h组及<48 h组年龄、性别构成、合并疾病比例、LAD、LVEF比较,差异无统计学意义(P均>0.05)。≥48 h组较<48 h组TpP及Ps水平偏高,但差异无统计学意义(P均>0.05)。持续性AF组和阵发性AF组年龄、性别构成、合并高血压比例、LAD、LVEF比较,差异无统计学意义(P均>0.05)。持续性AF组较阵发性AF组合并糖尿病比例、TpP水平、Ps水平偏高,但差异无统计学意义(P均>0.05)。结论 NVAF患者当CHADS2≥2时TpP及Ps水平增高,监测TpP和Ps水平有益于识别卒中危险。
血栓前体蛋白;P选择素;心房颤动
心房颤动(房颤,AF)是临床常见的心律失常,由于心血管疾病谱的变化,非瓣膜性疾病成为AF最常见的病因[1]。左房血栓引起AF,而左房血栓形成的机制涉及局部血流淤滞、内皮功能障碍及血液的高凝状态等。血栓前体蛋白(TpP)是血栓中不溶性纤维蛋白的直接前体,在血浆中的浓度反映了循环中凝血酶的活性。TpP水平升高表明有急性血栓形成的危险,有较高的诊断灵敏性。P选择素(Ps)是细胞黏附分子选择素家族成员之一,在炎症反应的启动、介导白细胞在内皮上黏附和聚集及血栓形成过程中均发挥重要作用[2]。本研究在分析非瓣膜病性房颤(NVAF)患者TpP与Ps水平变化并探讨其临床意义。
1 资料与方法
1.1 研究对象和分组 选择2014年5月~2015年10月于沈阳医学院附属第二医院心血管内科住院治疗NVAF患者206例,作为NVAF组,男性132例,女性74例,年龄39~79岁。NVAF定义:无风湿性二尖瓣狭窄、机械/生物瓣膜、二尖瓣修复情况下发生的AF[3]。其中冠状动脉粥样硬化性心脏病(冠心病)167例,扩张型心肌病(扩心病)39例。排除标准:合并急性冠脉综合症、感染性疾病、肝功能指标超过正常范围上限3倍、肌酐清除率<60 ml/min、甲状腺功能及凝血功能异常、恶性肿瘤、出血性疾病、服用华法林患者。另入选冠心病(78例)和扩心病(2例)无AF患者作为对照组(80例),男性48例,女性32例,年龄40~78岁。NVAF组患者依据CHADS2评分分为CHADS2≥2组(87例)及CHADS2<2组(119例);另外NVAF组患者中接诊时可明确AF发作时间者共87例,按AF持续时间分为≥48 h组(59例)及<48 h组(28例);此外NVAF组患者中住院期间可明确区分AF类型者共102例,分为持续性AF组(66例)和阵发性AF组(36例)。
1.2 方法 收集入选者病例基线资料包括:性别、年龄、左房内径(LAD)、左室射血分数(LVEF)、AF持续时间和类型、CHADS2评分[4]等。AF类型包括持续性和阵发性,持续性AF定义为AF发作需要药物或者电复律干预,阵发性AF为AF发作7 d内可自行终止。所有入选者于入院次日清晨抽取空腹静脉血4 ml,TpP管用枸椽酸钠抗凝,3000 rpm离心10 min,收集血清和血浆于-70℃保存待测。应用酶联免疫吸附法(Elisa)测定血清Ps(试剂盒由BPB Biomedicals.Inc 提供)和血浆TpP(试剂盒购于上海西唐生物科技有限公司)。
1.3 统计学分析 所有数据用SPSS 13.0统计软件进行分析。计量资料采用均数±标准差(±s)表示,两组间均数的比较采用t检验,计数资料采用例数(构成比)表示,组间比较采用χ2检验。P<0.05为差异有统计学意义。
2 结果
2.1 NVAF组与对照组患者基线资料比较 两组年龄、性别构成、合并疾病比例、LAD、LVEF比较,差异无统计学意义(P均>0.05)。NVAF组较对照组TpP、Ps略有升高,但差异无统计学意义(P均>0.05)(表1)。
2.2 CHADS2≥2组与CHADS2<2组基线资料比较 与CHADS2<2组比较,CHADS2≥2组年龄、合并高血压与糖尿病比例增加,TpP及Ps水平显著升高,差异有统计学意义(P均<0.05)(表2)。
2.3 AF持续时间≥48 h组及<48 h组基线资料比较 两组年龄、性别构成、合并疾病比例、LAD、LVEF比较,差异无统计学意义(P均>0.05)。≥48 h组较<48 h组 TpP及Ps水平偏高,但差异无统计学意义(P均>0.05)(表3)。
2.4 持续性AF组和阵发性AF组基线资料比较 两组年龄、性别构成、合并高血压比例、LAD、LVEF比较,差异无统计学意义(P均>0.05)。持续性AF组较阵发性AF组合并糖尿病比例、TpP水平、Ps水平偏高,但差异无统计学意义(P均>0.05)(表4)。
3 讨论
AF是最常见的心律失常之一。心室律(率)紊乱、心功能受损和心房附壁血栓形成是主要病理生理特征。血栓栓塞是AF最严重的并发症,血栓形成原因有:①AF时心房失去有效收缩,导致血流缓慢、淤滞及血液流变学发生改变;②AF时心房和肺静脉内膜受损以及血液成份发生改变;③在心腔内膜细胞、血小板、凝血、纤溶系统以及血液流变学等多种因素变化的综合作用下促成血栓形成。TpP为高分子量可溶性纤维蛋白多聚体,是不溶性纤维蛋白的直接前体,其水平升高表示血栓形成已经启动并且纤维蛋白单体已开始聚合,是反映血栓前状态的敏感指标[5]。Ps是重要的黏附分子之一,可介导炎症细胞与血小板、内皮细胞黏附活化,参与血栓形成,是评估体内高凝状态及血栓形成倾向的敏感指标[6,7]。本研究中通过检测TpP及Ps水平发现,NVAF患者两项指标高于非AF患者,进一步证实AF患者存在血栓前状态,与Sohara等[8]研究结果一致。
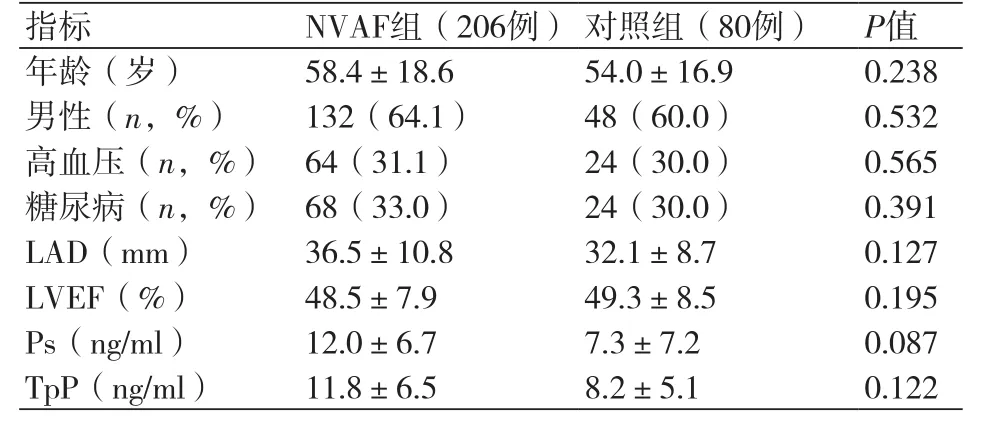
表1 NVAF组与对照组患者基线资料比较
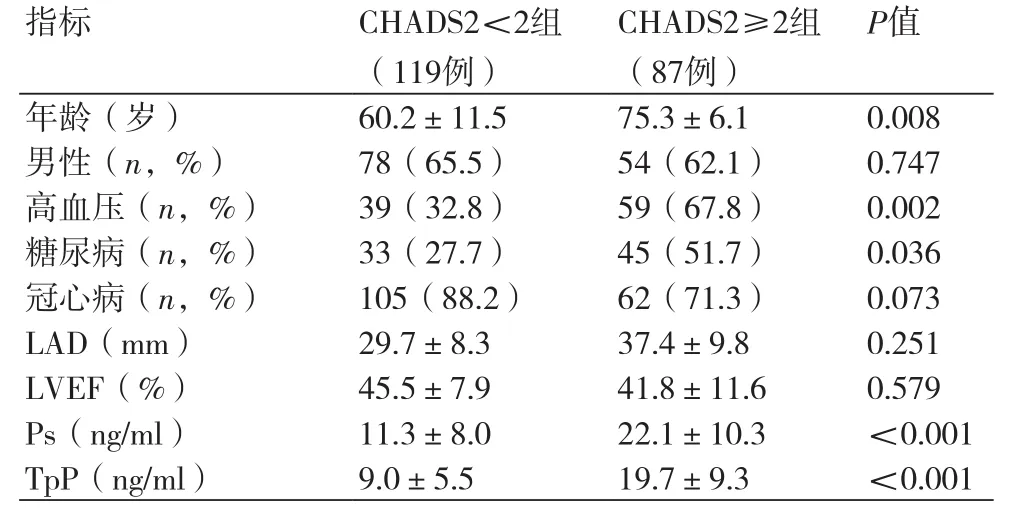
表2 CHADS2≥2组与CHADS2<2组基线资料比较

表3 房颤持续时间≥48 h组及<48 h组基线资料比较
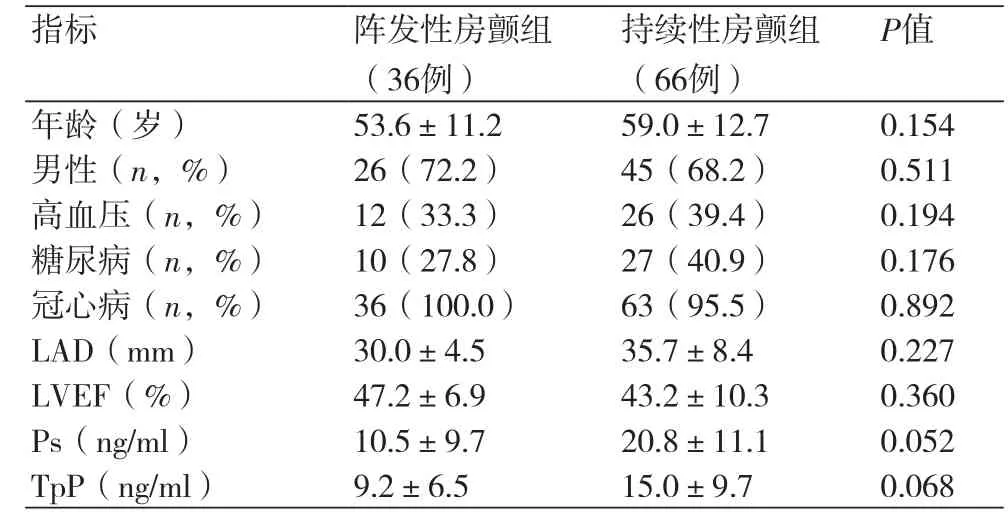
表4 持续性房颤组和阵发性房颤组基线资料比较
AF转复时血栓栓塞发生风险为5%~7%,转复后心房的功能障碍将持续一段时间,心房顿抑常需要几天或几周恢复,在此期间血流动力学改变产生高切变力导致心房内膜细胞损伤和胶原暴露,血小板激活黏附。对于持续时间超过48 h的AF,仍处于血栓形成风险中。高龄、肥胖、合并器质性心脏病、左房增大等是阵发性AF进展为持续性AF的预测指标[9],上述指标均与炎症反应及动脉粥样硬化形成相关,易致血小板活化、血管内皮损伤。本研究中,AF发作持续时间≥48 h患者TpP及Ps水平高于<48 h患者,持续性AF患者TpP及Ps水平高于阵发性AF患者。
CHADS2评分是临床常用的卒中危险评分系统,≥2者为卒中高危人群,该人群中已发生栓塞、高血压、糖尿病、心力衰竭且高龄居多。本研究中,与CHADS2<2组比较,CHADS2≥2组年龄较高,合并高血压与糖尿病比例增加,TpP及Ps水平显著升高。监测外周血TpP和Ps水平有益于识别存在高凝状态及血栓形成倾向的患者,及时干预,预防栓塞发生。
[1] 中华医学会心血管病分会. 中国部分地区心房颤动住院病例回顾性调查[J]. 中华心血管病杂志,2013,31(12):913-6.
[2] 刘兆奕,刘丽敏. 血栓前体蛋白与P 选择素对老年急性冠脉综合征的预测价值[J]. 中国老年保健医学,2013,11(1):10-2.
[3] January CT,Wann LS,Alpert JS,et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society[J]. Circulation,2014,130(23):e199-267.
[4] Camma J,Kirchhof P,Lipg Y,et al. Guidelines for the management of atrial fibrillation: the task force for the management of atrial fibrillation of the European society of cardiology (esc)[J]. Eur Heart J,2010,31(19):2369-429.
[5] 蔡凯,徐辉,夏明凯,等. 不同类型冠心病病人血浆血栓前体蛋白和纤维蛋白原含量的变化[J]. 中西医结合心脑血管病杂志,2005,3(12):1035-6.
[6] 王锋. P选择素与糖尿病肾病[J]. 中华糖尿病杂志,2005,13(5):396-400.
[7] 白晓玲. 血小板活化状态与原发性肾病综合征患儿高凝状态的研究[J]. 肾脏病与透析肾移植杂志,1999,8(1):34-5.
[8] Sohara H,Amitani S,Kurose M,et al. Atrial fibrillation activates platelets and coagulation in a time-dependent manner: a study in patients with paroxysmal atrial fibrillation[J]. J Am Coll Cardiol,1997, 29(1):106-12.
[9] Huxley RR,LopezFL,FolsomAR,et al. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: The Atherosclerosis Risk in Communities(ARIC) Study[J]. Circulation, 2011,123(14):1501-8.
本文编辑:姚雪莉
Level changes of thrombus precursor protein and P-selectin in patients with non-valvu1ar atrial fibrillation
ZHAO Hong-li*, LIU Li-min, ZHANG Xiao-dan, ZHOU Jia-meng, WANG Xiao-xi.*Department of Cardiovascular Diseases, Second Affiliated Hospital of Shenyang Medical College, Shenyang 110002, China.
Objective To analyze the level changes of thrombus precursor protein (TpP) and P-selectin (Ps) in patients with non-valvu1ar atrial fibrillation (NVAF). Methods NVAF patients (n=206, male 132, female 74 and aged from 39 to 79) were chosen and included into NVAF group from the Department of Cardiovascular Diseases of the Second Affiliated Hospital of Shenyang Medical College from May 2014 to Oct. 2015. The patients with coronary heart disease (CHD, n=78) and dilated cardiomyopathy (DCM, n=2) were chosen and included into control group (n=80). NVAF group was divided, according to CHADS2 scores, into CHADS2≥2 group (n=87) and CHADS2<2 group (n=119). There were 87 cases in NVAF group with definite AF attack time and they were divided into ≥48 h group (n=59) and <48 h group (n=28). In addition, there were 102 cases in NVAF group with definite AF types and they were divided into sustained AF group (n=66) and paroxysmal AF group (n=36). The baseline materials were collected from the patients, including sex, age, left atrial diameter (LAD), left ventricular ejection fraction (LVEF), duration and types of AF and CHADS2 scores. The levels of Ps and TpP were detected by using enzyme-linked immunosorbent assay (ELISA). Results The comparison in compositions of age and sex, ratio of patients with complicating diseases, LAD and LVEF had no statistical significance between NVAF group and control group (all P>0.05). The levels of TpP and Ps increased a little in NVAF group compared with control group but the difference was not statistically significant (all P>0.05). Compared with CHADS2<2 group, age and ratio of patients with complicating hypertension and diabetes increased, and levels of TpP and Ps increased significantly in CHADS2≥2 group (all P<0.05). The comparison in compositions of age and sex, ratio of patients with complicating diseases, LAD and LVEF had no statistical significance between ≥48 h group and <48 h group (all P>0.05). The levels of TpP and Ps increased a little in ≥48 h group compared with <48 h group but the difference was not statistically significant (all P>0.05). The comparison in compositions of age and sex, ratio of patients with hypertension, LAD and LVEF had no statistical significance betweensustained AF group and paroxysmal AF group (all P>0.05). The ratio of patients with complicating diabetes and levels of TpP and Ps were higher in sustained AF group than those in paroxysmal AF group but the difference was not statistically significant (all P>0.05). Conclusion The levels of TpP and Ps are higher in NVAF patients with CHADS2≥2. Monitoring the levels of TpP and Ps is beneficial to identifying stroke risk.
Thrombus precursor protein; P-selectin; Atrial fibrillation
R541.75
A
1674-4055(2016)11-1326-03
沈阳市科技创新专项资金(F14-158-9-27);沈阳医学院科技基金项目(20131013)
1110002 沈阳,沈阳医学院附属第二医院心血管内科
刘丽敏,E-mail:zhaoyi1013@163.com
10.3969/j.issn.1674-4055.2016.11.12