专业护理干预对院内缺血性卒中患者从发现至静脉溶栓用药时间的影响
方 霞,汪 燕,刘 斌,刘 燕,顾 群
·临床医学·
·论著·
专业护理干预对院内缺血性卒中患者从发现至静脉溶栓用药时间的影响
方 霞,汪 燕,刘 斌,刘 燕,顾 群
目的 探讨专业护理对院内缺血性卒中患者从发现至静脉溶栓用药时间的影响。方法 选取我院2010-2016年发生缺血性卒中并实施重组人组织纤维蛋白溶酶原激活剂(recombinant tissue plasminogen activator,rt-PA)静脉溶栓的住院患者19例。将其中8例由急诊科和神经科经过溶栓专业培训护士实施静脉溶栓的患者归为专业组,将其余11例在其他科室住院期间发生缺血性卒中,由未经过溶栓培训护士实施rt-PA静脉溶栓的患者归为对照组。分别统计从发现至溶栓治疗时间(find to needle time,FNT)、下达医嘱到溶栓开始时间(preparation to needle time,PNT)以及患者溶栓后90 d的改良Rankin量表(modified Rankin scale,mRS)评分,分别对上述指标进行单因素分析,并通过问卷调查方式分别评估经过溶栓专业培训护士和未经过溶栓培训护士对院内卒中的认知情况。结果 单因素分析结果显示,专业组FNT明显短于对照组,差异有统计学意义(P<0.05);专业组PNT明显短于对照组,差异有统计学意义(P<0.05);2组患者溶栓治疗后90 d的mRS评分无明显差异(P>0.05);经过溶栓专业培训的护士对院内卒中的认知程度明显高于未经过溶栓培训的护士。结论 急诊和神经科病区院内卒中的FNT明显短于其他科室;经过正规溶栓培训的护士可以缩短院内卒中FNT。
静脉溶栓;院内卒中;溶栓护理
院内卒中(in-hospital stroke,IHS)是指非卒中原因住院患者在住院期间发生的卒中,占急性卒中的4%~17%,其中手术和实施有创操作患者发生率高[1]。我院缺血性卒中静脉溶栓工作主要在急诊与神经内科进行,护理人员均受过溶栓专业培训,IHS患者可以及时行溶栓治疗,而其他科室IHS患者的静脉溶栓率偏低,与非溶栓专业科室缺乏急性卒中处置的相关培训有关,因此本研究试图分析并探讨不同护理人员对院内缺血性卒中静脉溶栓用药时间的影响,为进一步优化IHS静脉溶栓流程提供依据。
1 对象与方法
1.1 研究对象
选取2010-2016年在我院实施重组人组织纤维蛋白溶酶原激活剂(recombinant tissue plasminogen activator,rt-PA)静脉溶栓的IHS患者共19例作为研究对象。其中男13例,女6例,年龄65~90岁,平均(80.26±8.35)岁。纳入对象符合《中国急性缺血性脑卒中诊治指南2014》诊断标准[2],均经头颅磁共振确诊,有详细的溶栓记录。将以上患者分为2组,(1)专业护理组:由经过溶栓专业护理培训护士进行静脉溶栓的急诊科和神经科住院患者8例,其中男性5例,女性3例,年龄65~89岁,平均(77.75±9.80)岁;(2)对照组:由未经过溶栓护理培训护士进行静脉溶栓的其他科室住院患者11例,其中男性7例,女性4例,年龄66~90岁,平均(78.09±8.71)岁。2组患者一般资料比较差异无统计学意义(P>0.05),具有可比性。分别选取经过溶栓专业培训的急诊和神经科护士,以及未经过溶栓培训的其他科室护士各25名作为问卷调查对象。
1.2 方法
1.2.1 数据采集 通过回顾溶栓记录和医嘱记录对IHS静脉溶栓患者的救治过程进行还原。统计护士发现患者出现症状至静脉开始注射药物的时间(find to needle time,FNT)。医生下达静脉溶栓医嘱至溶栓开始的时间(preparation to needle time,PNT)。溶栓治疗90 d后随访,对患者进行改良的Rankin量表(modified Rankin scale,mRS)评分。
1.2.2 问卷调查 问卷由神经科医师自行设计,采用现场填写的方式进行,20 min内完成。共发放问卷50份,回收有效问卷46份,有效回收率为92%。按是否接受过rt-PA静脉溶栓培训将参加问卷调查的护士分为受训组和对照组,并分别计算各组回答的正确率。
1.3 统计学处理
运用SPSS 20.0软件进行统计学分析。计数资料组间比较采用χ2检验,计量资料用均数±标准差(x±s)表示,进行方差齐性检验,组间比较采用两独立样本t检验,P<0.05为差异有统计学意义。
2 结果
2.1 计量资料单因素分析
2组间IHS患者年龄差异无统计学意义(P>0.05),FNT、PNT差异有统计学意义(P<0.05或P<0.01)。患者溶栓后90dmRS评分差异无统计学意义(P>0.05)。见表1。

表1 2组患者FNT、PNT及mRS评分的比较(x±s)
注:FNT:发现至溶栓时间,PNT:下达医嘱至溶栓开始时间,mRS:改良Rankin量表
2.2 问卷调查结果分析
问卷调查结果显示,受训组护理人员在对IHS患者的识别、rt-PA静脉溶栓流程、配药方法和并发症认知方面,回答正确率均高于对照组。见表2。
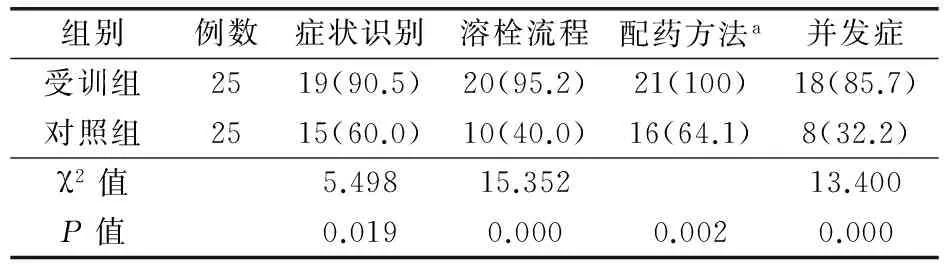
表2 2组护理人员对IHS静脉溶栓的认知程度比较[例(%)]
注:a使用Fisher确切概率法。IHS:院内卒中
3 讨论
急性缺血性卒中是急诊科和神经科的常见病,而rt-PA静脉溶栓是目前公认最有效的治疗方法之一[3]。患者发病后如能及时给予静脉溶栓治疗,使闭塞的血管再通,可改善缺血半暗带的供血,缩小脑梗死面积,从而减轻脑组织的损伤程度[4]。我院自2009年开始急性脑梗死rt-PA静脉溶栓以来,致力于开展急诊和神经科医护人员的溶栓培训、简化诊治流程、加强部门协作,力争缩短急诊患者到院至溶栓的时间。而发生在院内非卒中治疗科室的急性脑梗死常由于医务人员缺乏相关培训及知识,无法及时识别,加上重视程度不够、会诊延误、检查耗时等问题,错过了溶栓治疗的最佳时机。护士往往是IHS患者的第一发现人,护士对急性脑卒中认知和判断存在差异,经过溶栓培训的护士能够更快地识别并报告责任医师,配合医师完成溶栓前的各项化验检查并及时给予患者溶栓药物,从而缩短FNT[5]。本研究问卷调查结果显示,受训组护士在症状识别、溶栓流程、溶栓药物使用以及溶栓并发症的认识方面均高于对照组,溶栓前的准备时间也短于对照组。理论上IHS患者发病时已在院内,其FNT应明显短于院外卒中患者。但事实并非如此,非专业科室的IHS患者在院内诊治过程中耽搁了大量时间,在早期识别、科室协作、检查化验、谈话沟通,护理工作方面的问题也较为突出,例如溶栓前静脉通道的建立、心电监护仪和注射泵的安装、导尿和胃管置入等操作延误都会增加FNT。以上问题共同导致了IHS患者发病至溶栓时间的延长,同时也提示院内卒中溶栓流程仍有很大的优化空间。与患者接触最多的护理人员,是静脉溶栓的关键一环,对待急性卒中应有警惕性和时间紧迫感,并熟知静脉溶栓的流程和溶栓药物的使用方法,为减少IHS患者的死亡率和致残率做出努力。此外,笔者观察到2组IHS溶栓患者溶栓后90 d的mRS评分无统计学差异,可能与样本量的限制有关。笔者初步探讨了护理工作对院内卒中静脉溶栓的影响,下一步将对护理工作在静脉溶栓过程中的各环节和步骤进行深入分析和研究。
[1] Saltman AP, Silver FL, Fang J, et al. Care and outcomes of patients with in-hospital stroke[J].JAMA Neurol, 2015, 72(7): 749-755. DOI:10.1001/jamaneurol.2015.0284.
[2] 中华医学会神经病学分会. 中国急性缺血性脑卒中诊治指南(2014)[J]. 中华神经科杂志, 2015, 48(4):246-257.
[3] Gumbinger C, Reuter B, Stock C, et al. Time to treatment with recombinant tissue plasminogen activator and outcome of stroke in clinical practice: retrospective analysis of hospital quality assurance data with comparison with results from randomised clinical trials[J]. BMJ, 2014, 348: g3429. DOI:10.1136/bmj.g3429.
[4] 肖静,江思德,唐明山. 急性脑梗死患者阿替普酶静脉溶栓预后相关危险因素初步研究[J]. 河北医学, 2015, 21(1): 30-32. DOI:10.3969/j.issn.1006-6233.2015.01.010.
[5] 何霞婷,褚安红. 急诊专业组护士对急性脑卒中患者诊疗时间的影响[C]. 中华医学会急诊医学分会第十六次全国急诊医学学术年会论文集, 2013: 353.
(本文编辑:彭润松)
Effect of professional nursing intervention on the medication time of intravenous thrombolytic therapy in inpatients with ischemic stroke
Fang Xia, Wang Yan, Liu Bin, Liu Yan, Gu Qun
(Department of Neurology, No. 411 Hospital of CPLA, Shanghai 200081, China)
Objective To investigate the effect of professional nursing intervention on the medication time of intravenous thrombolytic therapy in inpatients with ischemic stroke.Methods Selected for the study were 19 cases of ischemic stroke that occurred during their stay in the hospital from 2010 to 2016, and they were treated with intravenous thrombolysis of recombinant human tissue plasminogen activator (rt-PA). Of the 19 cases, 8 cases treated with intravenous thrombolysis implemented by trained professional nurses in the emergency and the neurology departments were assigned as the professional nursing group, the other 11 cases treated with intravenous thrombolysis of rt-PA implemented by non-professional nurses in other medical departments were assigned as the control group. Statistical analyses were made on the scores of from perceiving to needle time (PNT), find to needle time (FNT) and the scores of Modified Rankin Scale(MRS)90 days after thrombolytic therapy, and single-factor analyses were also made on the above indicators. Then, awareness of ischemic stroke perceived respectively by trained professional nurses and non-professional nurses was assessed by the approach of questionnaire.Results Single-factor analyses indicated that PNT of the trained professional nursing group was significantly shorter than that of the control group, and statistical significance could be noticed when comparisons were made between them(P<0.01). The FNT of the trained professional nursing group was also significantly shorter than that of the control group, and there was no statistical significance when comparisons were made between them(P<0.05). And there were neither significant differences in mRS scores 90 days after intravenous thrombolytic therapy, when comparisons were made between the 2 groups(P<0.05). The awareness of in-hospital stroke by the professional nursing group was significantly higher than that of the non-professional nursing group.Conclusion The PNT of the in-hospital stroke patients in the emergency and neurological wards was significantly shorter than that of the other departments of the hospital. Nurses with regular thrombolytic therapy training could obviously shorten the time from stroke onset to thrombolytic therapy.
Intravenous thrombolysis; In-hospital stroke; Thrombolytic nursing
200081 上海,解放军第四一一医院神经内科(方霞、汪燕、刘燕、顾群);海军上海东体育会路离职干部休养所(刘斌)
顾群,电子信箱:gq1975@soho.com
R473.74
A [DOI] 10.3969/j.issn.1009-0754.2016.05.018
2016-06-16)