Human and animal sarcocystosis in Malaysia∶A review
Baha Latif,Azdayanti Muslim
Parasitology Discipline,Faculty of Medicine,Universiti Teknologi MARA,Sungai Buloh,Selangor,Malaysia
Human and animal sarcocystosis in Malaysia∶A review
Baha Latif,Azdayanti Muslim*
Parasitology Discipline,Faculty of Medicine,Universiti Teknologi MARA,Sungai Buloh,Selangor,Malaysia
ARTICLE INFO
Article history:
revised form 12 Aug 2016
Accepted 25 Aug 2016
Available online 24 Sep 2016
Sarcocystosis
Zoonosis
Human
Animal
Malaysia
Sarcocystosis is a zoonotic disease caused by a coccidian intracellular protozoan parasite of the genus Sarcocystis.More than 200 Sarcocystis species have been recorded and the parasites are found in mammals,birds and reptiles.They require two hosts to complete their life cycle.In Malaysia,sarcocystosis was reported as a potential emerging food and water-borne disease after a series of large outbreak of human infections.There was not enough attention given before even though it was reported in both humans and animals. The first human case of invasive muscular sarcocystosis among local Malaysian was reported in 1975.Besides,a retrospective autopsy examination on 100 tongues revealed 21%positive cases.On top of that,a sero-epidemiological survey conducted in 243 subjects in West Malaysia showed that 19.7%had Sarcocystis antibodies.The clinical symptoms of muscular sarcocystosis were first described comprehensively in 1999. Meanwhile,many types of animals including livestock were found harbor the sarcocysts in their tissue.The first case of human intestinal sarcocystosis was reported in 2014.This review indicates that human sarcocystosis is currently endemic in Malaysia and parallel to that reported in animals.However,more studies and investigations need to be conducted since the source of human infection remains unknown.
1.Introduction
Sarcocystosis is a zoonotic disease caused by a coccidian intracellular protozoan of the genus Sarcocystis.Sarcocystis spp. requires two hosts to complete its life cycle;with sexual reproduction in the intestine of carnivores or omnivores(definitive host)and asexual reproduction in the tissues of herbivores(intermediate hosts)[1].It was first observed in 1843 by Miescher as white threadlike cysts and simply known as Miescher's tubule for 20 years[1].To date,there are more than 200Sarcocystisspeciesrecorded in the world and the parasites can be found in the tissues of mammals,humans,birds,reptiles and probably in fish[1,2].
There are two forms of sarcocystosis inflicting in man;intestinal and muscular.Intestinal sarcocystosis is acquired whenhumans eat raw or undercooked meat which harbors the cystic stage of the parasite.Man becomes the definitive host after the ingestion of raw beef or pork infected with Sarcocystis hominis(S.hominis)and Sarcocystis suihominis(S.suihominis),respectively[2].If acquired,it can cause gastroenteritis.However,in most people,the infections are asymptomatic and self-limiting[1,2].Muscular sarcocystosis infection is acquired by the ingestion of contaminated food and water with sporocysts[3]. In this case,the parasite forms the muscular type in which consequently cause clinical signs such as fever,myalgia and arthralgia.Generally,based on early reports,the prevalence of human extra intestinal sarcocystosis was considered low with only less than 100 cases reported worldwide[1].
Tel:+60 125740014,+60 36126 7428
Fax:+60 36126 7073
E-mail:azdayanti@salam.uitm.edu.my
Foundation Project:Partly supported by Ministry of Education,Malaysia under Research Acculturation Grant Scheme(RAGS)Grant(600-RMI/RAGS 5/3(76/ 2014)).
Peer review under responsibility of Hainan Medical University.The journal implements double-blind peer review practiced by specially invited international editorial board members.
In Malaysia,muscular sarcocystosis was reported as a potential emerging food-borne zoonosis after a series of large outbreak of human infections.However,there was not enough attention given before even though it was reported in both humans and animals.Therefore,the aim of this review is to provide the latest updates regarding sarcocystosis in humans and animals in Malaysia.
2.Human muscular sarcocystosis
Historically,the first case of muscular sarcocystosis in Malaysia recorded involving an English man who had returnedto England from Sarawak,East Malaysia[4].Second case was reported by Jeffrey in 1974,in patient who also had returned to U.K from Malaysia[5].However,the first human case of extra-intestinal sarcocystosis among local Malaysian was reported in 1975 which involved a Malay man[6]followed by an incidental finding of sarcocyst in nasopharyngeal/oropharyngeal tissues of an Orang Asli girl with malignancy[7]within the same year.Since that,a total of~13 cases of invasive muscular sarcocystosis have been reported sporadically until 1992[8-10]. However,most of the findings were incidentally taken from autopsied/biopsied specimens with no symptoms described.In addition,most of the cases were associated with malignancies. Nevertheless,seroprevalence study conducted in 1978 showed that 20%out of 243 respondents from four main ethnic groups in Malaysia had antibodies for Sarcocystis,indicating the endemicity of the disease[11].On top of that,examination of human tongue tissue in 100 routine autopsies revealed a prevalence rate of 21%[12].
2221-1691/Copyright©2016 Hainan Medical University.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
The clinical symptoms of the infection were first described in Malaysia after the firstoutbreak reported in1999 involving 7 out of 15 US servicemen[13].Acute manifestations including fever,myalgia and bronchospasm were noted and extensive investigation showed transient lymphadenopathy and subcutaneousnodulesassociated with eosinophilia,raised erythrocyte sedimentation rate,and elevated levels of muscle creatinine kinase.Muscle biopsy examination from one patient revealed microscopic sarcocysts.No more case of human sarcocystosis has been reported since 1999 until two large outbreaks of probable acute symptomatic muscular sarcocystosis which happened recently among travelers in two Malaysian islands(Figure 1),Tioman Island is located 32 km off the East Coast of Peninsular Malaysia,while Pangkor Island is located in Perak,3.5 km off the West Coast of Peninsular Malaysia.
The outbreak were known to start during the late summer of July-August 2011 after Geo Sentinel(The surveillance program of the International Society of Travel Medicine and Centers for Disease Control)reported at least 32 acute cases of extraintestinal sarcocystosis suspected among travelers upon returning home from Tioman Island[14].Most of them were from Germany while the others were from Europe,North America and Asia.The clinical symptoms of fever and severe muscle pain were recorded within days and weeks in addition to the laboratory findings which had shown peripheral eosinophilia and the rise of serum creatinine phosphokinase level.Further results from muscle biopsy taken from two patients had revealed the possibility of sarcocystosis in the patients[15,16]. Following that,a survey for sarcocystosis was conducted soon after the outbreak in Tioman Island by Malaysian authorities but no trace of Sarcocystis parasites were found in humans,animals or in the water samples during that time[14].A small number of samples was the limitation of the study.Moreover,no wild life was included for the screening of the study.

Figure 1.Location of the reported cases of human muscular sarcocystosis in Malaysia.
Approximately few months to one year later(July-August 2012),another wave of outbreak involving 65 people from various nationalities and with the history of travelling to Tioman Island were identified[17]with having almost similar symptoms as reported before.This second group of patients formed a total of 100 cases suspected with muscular sarcocystosis.Muscle biopsy taken form eight patients revealed that six of them had myositis and intramuscular cysts were identified in two patients[17].Slesak and his colleagues in their further investigations involving 26 patients in German reported that the incubation period was approximately 2 weeks with biphasic development[18].The third wave of extra intestinal sarcocystosis-like illness was suspected in May 2014 comprising 6 German patients[19]. All patients suffered from fever,myalgia and headache.No muscle biopsies were taken.However,the history,clinical symptoms and laboratory findings had shown the possibility of sarcocystosis.
Another concurrent outbreak of symptomatic sarcocystosis was reported within the same time frame(January 2012)but from different vicinity.From 92 college students and teachers,89 of them were identified with symptoms including fever,myalgia,headache and cough after visiting Pangkor Island[20]. Molecular detection from biopsied specimens of 4 patients had revealed that the infection was caused by Sarcocystis nesbitti(S.nesbitti)[20-22].Non-Malaysians were noticed to experience the symptoms longer and severe than the Malaysians[21]. Phylogenetic analysis suggested the source of infection was probably from snakes[22],but until now,the findings are still uncertain.
Therefore,following the latest outbreaks,it is now postulated that the possible source of infection of human muscular sarcocystosis in Malaysia is the contamination of food and water with sporocysts of S.nesbitti excreted with snakes(definitive hosts). Historically,the species was first discovered in the skeletal muscle of a rhesus monkey in China[23].Through intensive research conducted in Malaysia in search for the clue and source of infection,S.nesbitti have been identified in the fecal sample of Naja khaoutia(cobra)and in reticulated python by molecular analysis[24].The latter findings suggested the possibility of snake as the source of infection with rhesus monkey or rats probably serve as intermediate host(Figure 2). The summary of human muscular sarcocystosis in Malaysia is shown in Table 1.
The spectrum of clinical symptoms is broad and varies among individual ranging from asymptomatic to chronic and prolonged form of infection in which can also cause relapse[32]. Myalgia with or without fever,>5%eosinophilia,elevated serum creatinine phosphokinase levels,myositis and negative trichinellosis and toxoplasmosis by serology are considered as the most important parameters for acute muscular sarcocystosis[32].It was noted that the elevated level of blood eosinophils and serum creatinine phosphokinase were prominent during the late phase(~4 weeks post-departure)of period[19,32].
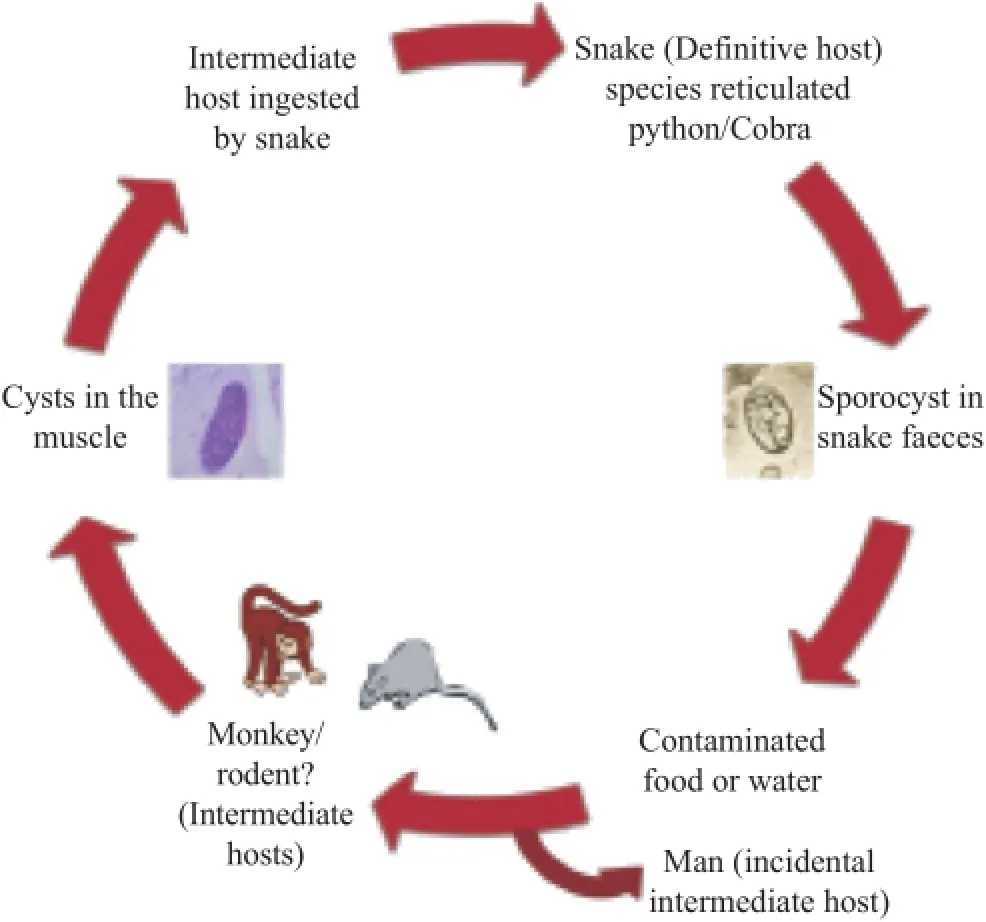
Figure 2.Possible sources of infection with human muscular sarcocystosis in Malaysia.
Generally,there is no definite treatment for human muscular sarcocystosis.The infection is usually mild and self-limiting in most of the cases,and no treatment is required.Anti-parasitic agents such as albendazole or ivermectin are used to suppress the symptoms of the infection.Oral steroids such as prednisolone(used for severe myalgia to reduce inflammation associated with muscularinvolvement)havebeen used for treatment in some of the cases[19,32].Metronidazole and cotrimoxazole(antibacterial)are used for eosinophilic myositis.Recent investigation following the outbreak cases of muscular sarcocystosis in Tioman Island indicated the effectiveness of cotrimoxazole in prolonged symptoms of the disease[31].
3.Animal muscular sarcocystosis
Sarcocystis species requires alternate intermediate host(prey)-definitive host(predator)relationship to complete the life cycle.In Malaysia,sarcocysts have been found in the muscle tissue of a variety of wild animals(intermediate hosts)including slow loris[33],long tailed monkey[34],and rodents[35,36].Apart from that,muscular sarcocystosis was reported in mammals and birds with 15%and 20%infection rate respectively in a studyconducted among necropsied wild captive and zoo animals[37]. Meanwhile,in livestock(Table 2),sarcocysts have been identified in water buffaloes[38-41],sheep[42,43],goats[43,44]and cattles[41,43,45].
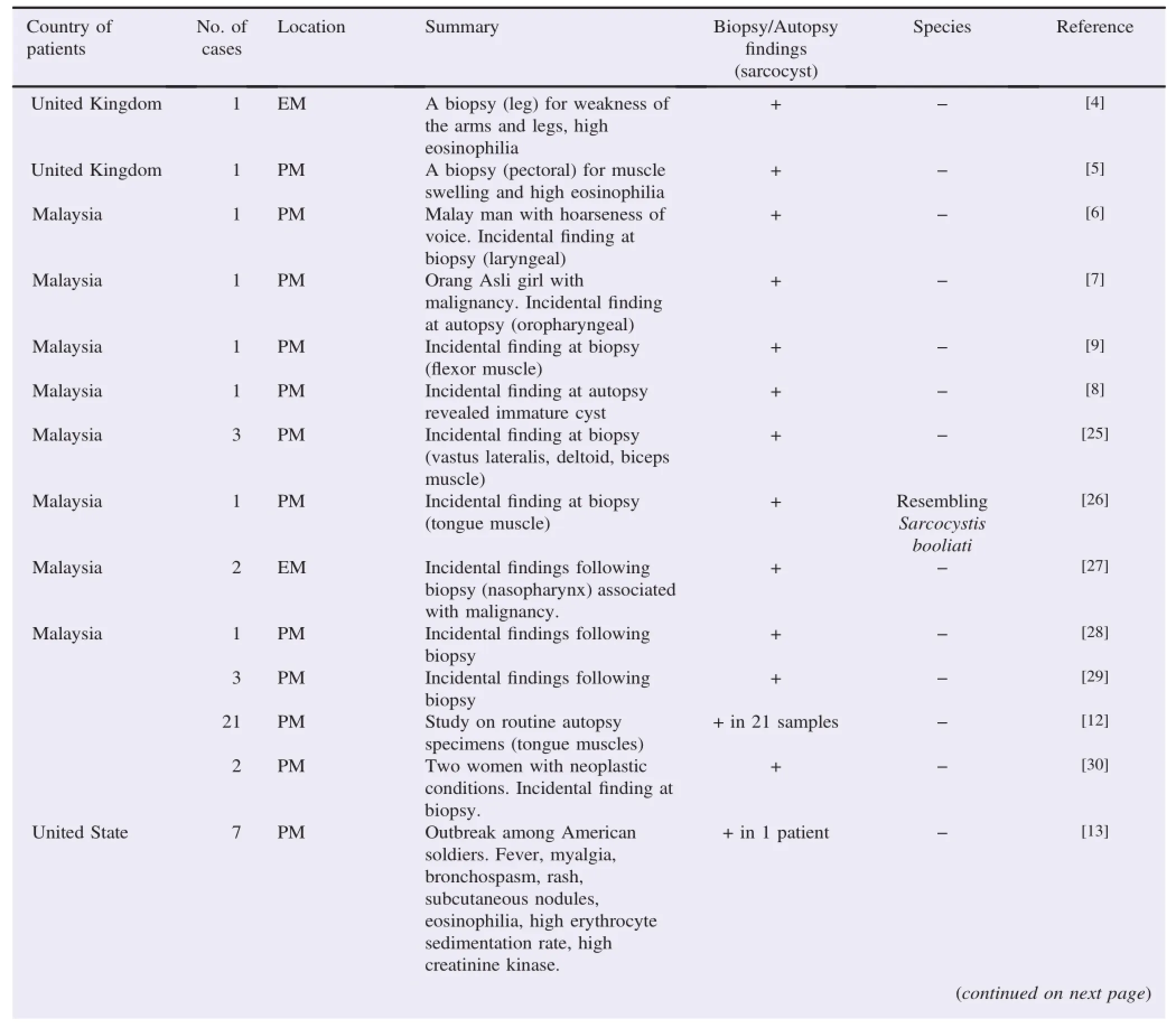
Table 1Reported cases of human muscular sarcocystosis in Malaysia during 1965-2014.
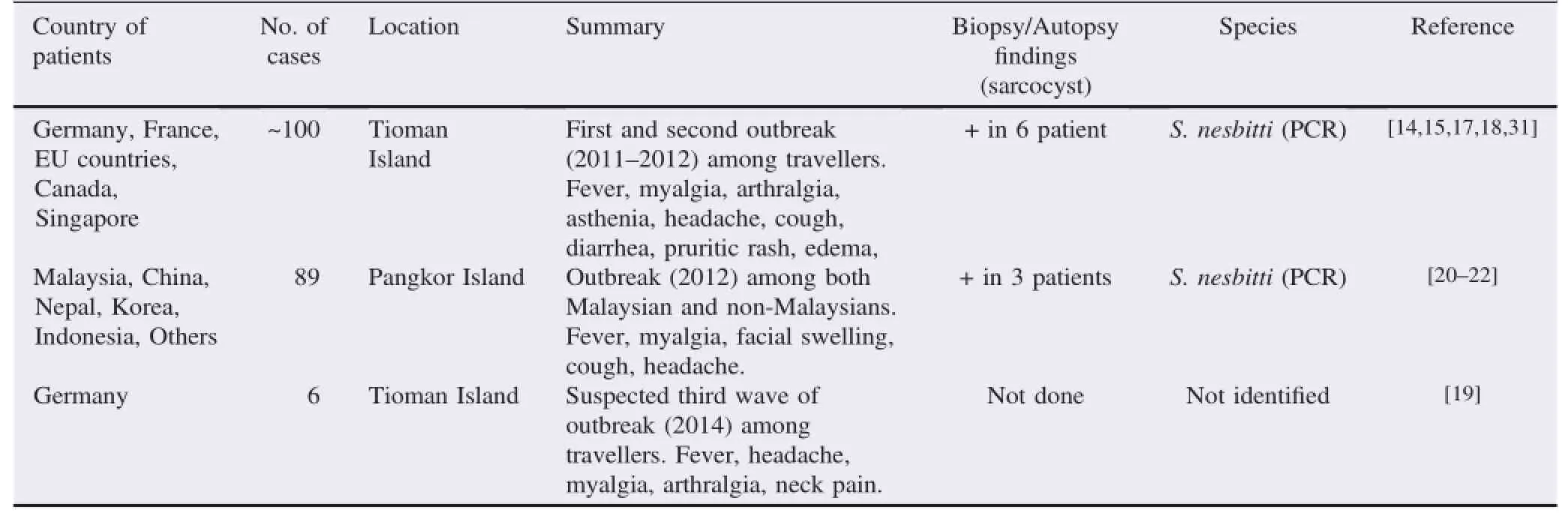
Table 1(continued)
The infection is usually mild and animals with muscular sarcocystosis seldom show any symptoms.However,some species are known to cause pathological effects in meatproducing animals including anorexia,anemia,weight loss,muscle weakness,lymphadenopathy,abortion,and eventually death in severe infections[2].The severity might be influenced by species of the Sarcocystis parasite,intensity of the infection and the condition of the animal(during pregnancy or lactation,stress)[2].Sarcocystis cruzi(S.cruzi)in cattle is the most prevalent and pathogenic[46].However,the parasites are usually seen mainly as an incidental finding at necropsy.
Even though many reportshavebeen established in Malaysia,the information regarding the source of infections(the definitive hosts)are relatively undetermined.The intermediate host/prey becomes infected by ingesting contaminated food/ water or environment with the sporocysts shed in the feces of the definitive hosts(Figure 3)[2].Cats and dogs are known as the definitive hosts for Sarcocystis fusiformis(S.fusiformis)and Sarcocystis levinei,respectively[38,40].Complete life cycle also was documented for Sarcocystis orientalis/Sarcocystis singaporensis,Sarcocystis villivillosus and Sarcocystis zamani in rats(Rattus norvegicus),which a Malaysian snake python served as the definitive host[47].

Figure 3.Sporocyst in dog's fecal sample(100×).
In sheep,four species of Sarcocystis have been documented. S.ovicanis and Sarcocystis arieticanis are pathogenic,form microscopic cysts,and are transmissible by dogs while Sarcocystis ovifelis and Sarcocystis medusiformis are non-pathogenic,form macroscopic cysts,and transmissible by cats.In goats,there are two microscopic forms:Sarcocystis capricanis andSarcocystis hircicanis,which dogs served as the definitive hosts. In cattle,the transmission of S.bovicanis is via canids,Sarcocystis hirsute is via felids and S.hominis is via human[4].PCR studies in Malaysia have identified S.ovicanis,S.capracanis,and S.bovicanis for sheep,goats and cattles,respectively[43]. Species identification either by molecular detection or ultrastructural studies is crucial because some species are more pathogenic to the livestock and most importantly,to detect the zoonotic species such as S.hominis.
Table 2Muscular sarcocystosis among meat producing animals in Malaysia.
4.Human and animal intestinal sarcocystosis
Human serves both as the definitive and intermediate hosts in the parasite's life cycle.The known species where man is confirmed as a definitive host are S.hominis and S.suihominis which can be acquired from infected beef and pork,respectively[2].
Only one case of intestinal sarcocystosis has been reported in Malaysia involving an asymptomatic female Orang Asli from Temiar group[48].However,the exact species was not determined in latter study as diagnosis was only performed by microscopic examination.It is speculated that the prevalence of intestinal sarcocystosis is underreported due to a lack of study conducted in Malaysia and the symptoms are usually mild or self-limiting.Most of the symptomatic cases found in natural-acquired or experimental study in other countries reported that the infected patients or volunteers experienced nausea,vomiting,acute or chronic diarrhea and abdominal pain[1].The range of the clinical manifestations depends on the intensity ofinfection orthe speciesofthe Sarcocystis parasites.Sarcocysts from pork is believed to cause more serious problem than beef[2].
5.Diagnosis
The diagnosis of muscular sarcocystosis is usually made by detection of macroscopic or microscopic cysts(Figure 4)in the tissue sample of skeletal muscle,tongue,esophagus,diaphragm and heart.Macroscopic cyst can be seen by naked eyes,but it is restricted to a few species such as S.fusiformis in water buffalo and S.nesbitti in long tailed monkey[49].The cysts are spindle to oval in shape,two stages are recognized,the peripheral metrocytes and large numbers of centrally located bananashaped bradyzoites.Sizes of cysts and bradyzoites vary among species.These differences in the size of the cysts and internal structures could attribute to the cyst age and strains of the Sarcocystis spp.
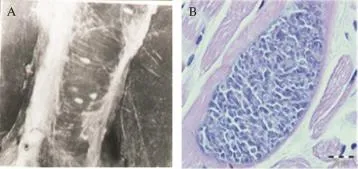
Figure 4.A:Macroscopic sarcocysts in animal muscle tissue;B:Microscopic sarcocyst in animal muscle tissue.H&E 100×.
The actual prevalence of muscular sarcocystosis needs to be addressed carefully due to the difference in approached diagnostic.Direct muscle/tissue compression between two glass slides is considered as the most rapid and easiest method for microscopic examination.The technique has been used widely in Malaysia[37,41,43,44],but its sensitivity is low[44].To improve the detection,Ng et al.has suggested the use of modified methylene blue staining(without acetic acid)in a tissue compression technique[50].Moreover,the latter technique was reported to have a moderate agreement with nested PCR. Therefore,it would be useful in examining large numbers of samples.
Other methods used for microscopic examination are histological examination with H&E or Giemsa staining and peptic digestion and immunofluorescent[51].In Malaysia,indirect fluorescence antibody technique method was used to detect the prevalence of antibodies to Sarcocystis,but some serum showed positive reactions to Toxoplasma as well[11].Whether due to cross reaction or poly-parasitism,it could not been justified.For the identification of the species,most of the previous studies depended on the morphology,size of the cyst(Figure 5)and the thickness of the cyst wall.Electron microscopy was commonly used to differentiate the structure of the sarcocysts[34,38].
Lately,molecular-based techniques(PCR)have been used frequently especially for the identification of the species due to its reliability and accuracy.However,it should be incorporated with other standard detection methods for sarcocystosis[44]. The final diagnosis is still by looking at the presence of sarocysts in the autopsied,biopsied or necropsied specimens. In Malaysia,S.ovicanis,S.capracanis,S.bovicanis and the latest S.nesbitti,Sarcocystis singaporensis and Sarcocystis zuoi have been identified by molecular techniques[20,22,43,45,47].
For intestinal sarcocystosis,diagnosis is usually made by the detection of oocyst/sporocyst in the stool sample of humans or animals(predators/definitive hosts).Generally,acid-fast stain such as Ziehl-Neelsen staining is used to demonstrate apicomplexan parasite including Sarcocystis species.However,the latter technique is limited to the time of sporocysts excretion.According to Dubey,the pre-patent periods for S.hominis and S.suihominis are 14-18 days and 11-13 days,respectively[2].To the best of our knowledge,onlyone case of human intestinal sarcocystosis has been reported in Malaysia by microscopic examination but the species could not be determined[48].While in animals,intestinal sarcocystosis infection is commonly detected by mucosal scrapings during the post mortem rather than stool examination.
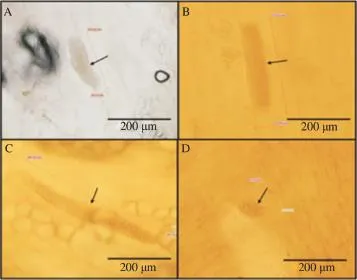
Figure 5.Different size of microsarcocysts from animal tissue.
Considering the limitations,molecular studies could be the best way to identify the Sarcocystis parasite.Latest finding by Lau et al.(2013)has identified Sarcocystis spp in the stool sample of snakes located in Malaysia by phylogenetic analyses based on 18S rRNA sequenced data[24].Still,both microscopy and molecular analysis are important and should be incorporated together for future studies.
6.Conclusion
Extra precautions should be undertaken to avoid the infections.Following recent outbreaks,Centers for Disease Control has suggested few recommendations for safe food and water consumption.Any person who is experiencing fever or prominent myalgia with travelling history to Tioman Island/Pangkor Island or any tropical countries is encouraged to seek some medical checkup.Human is most likely to acquire the infections by accidental ingestion of sporocysts shed by some carnivorous or predatory animals which would have acquired the infection by ingesting sarcocysts found in the herbivorous intermediate host.Human sarcocystosis is endemic in Malaysia and parallels to that reported in animals. It is suggested that the possibility of snake as the source of infection with rhesus monkey or rats may serve as the intermediate host.
Conflict of interest statement
We declare that we have no conflict of interest.
Acknowledgments
We would like to thank our institution,University Teknologi MARA for continuous support in the form of providing the facilities for our laboratory works.This paper is part of the research work funded by Ministry of Education,Malaysia under Research Acculturation Grant Scheme Grant(600-RMI/RAGS 5/3(76/2014)).
References
[1]Fayer R,Esposito DH,Dubey JP.Human infections with Sarcocystis species.Clin Microbiol Rev 2015;28(2):295-311.
[2]Dubey JP.Foodborne and waterborne zoonotic sarcocystosis.Food Waterborne Parasitol 2015;1(1):2-11.
[3]Dorny P,Praet N,Deckers N,Gabriel S.Emerging food-borne parasites.Vet Parasitol 2009;163(3):196-206.
[4]Mandour AM.Pathology and symptomatology of Sarcocystis infection in man.Trans R Soc Trop Med Hyg 1965;59(4):432-5.
[5]Jeffrey HC.Sarcosporidiosis in man.Trans R Soc Trop Med Hyg 1974;68(1):17-29.
[6]Kutty MK,Dissanaike AS.A case of human Sarcocystis infection in West Malaysia.Trans R Soc Trop Med Hyg 1975;69(5-6):503-4.
[7]Kutty MK,Mohan Das A,Dissanaike AS.Sarcocystis infection in an Orang Asli:the second human case from Malaysia.Southeast Asian J Trop Med Public Health 1975;6(3):400-1.
[8]Prathap K,Dissanaike AS.The fourth case of Sarcocystis infection in man in Malaysia.Southeast Asian J Trop Med Public Health 1978;9(3):452-3.
[9]Prathap K,Dissanaike AS.Third case of Sarcocystis from man in Malaysia.Southeast Asian J Trop Med Public Health 1976;7(3): 489.
[10]Kan SP,Pathmanathan R.Review of sarcocystosis in Malaysia. Southeast Asian J Trop Med Public Health 1991;22(Suppl 22): 129-34.
[11]Thomas V,Dissanaike AS.Antibodies to Sarcocystis in Malaysians.Trans R Soc Trop Med Hyg 1978;72(3):303-6.
[12]Wong KT,Pathmanathan R.High prevalence of human skeletal muscle sarcocystosis in south-east Asia.Trans R Soc Trop Med Hyg 1992;86(6):631-2.
[13]Arness MK,Brown JD,Dubey JP,Neafie RC,Granstrom DE.An outbreak of acute eosinophilic myositis attributed to human Sarcocystis parasitism.Am J Trop Med Hyg 1999;61(4):548-53.
[14]Husna Maizura AM,Khebir V,Chong CK,Shah A,Hakim L. Surveillance for sarcocystosis in Tioman Island,Malaysia.Malays J Public Health Med 2012;12(2):39-44.
[15]Sonnenburg FV,CramerJP,Freedman DO,PlierDA,Esposito DH,Sotir MJ,et al.Notes from the field:acute muscular sarcocystosis among returning travelers-Tioman Island,Malaysia,2011.MMWR Morb Mortal Wkly Rep 2012;61(2):37-8.
[16]Tappe D,Ernestus K,Rauthe S,Schoen C,Frosch M,Muller A,et al.Initial patient cluster and first positive biopsy findings in an outbreak of acute muscular Sarcocystis-like infection in travelers returning from Tioman island,Peninsular Malaysia,in 2011.J Clin Microbiol 2013;51(2):725-6.
[17]Esposito DH,Freedman DO,Neumayr A,Parola P.Ongoing outbreak of an acute muscular Sarcocystis-like illness among travellers returning from Tioman Island,Malaysia,2011-2012. Euro Surveill 2012;17(45):20310.
[18]Slesak G,Tappe D,Keller C,Cramer J,G¨uthoff W,Zanger P,et al.[Muscular sarcocystosis after travel to Malaysia:a case series from Germany].Dtsch Med Wochenschr 2014;139(19):990-5.German.
[19]Tappe D,Stich A,Langeheinecke A,von Sonnenburg F,Muntau B,Schafer J,et al.Suspected new wave of muscular sarcocystosis in travellers returning from Tioman Island,Malaysia,May 2014.Euro Surveill 2014;19:20816.
[20]Abubakar S,Teoh BT,Sam SS,Chang LY,Johari J,Hooi PS,et al. Outbreak of human infection with Sarcocystis nesbitti,Malaysia,2012.Emerg Infect Dis 2013;19(12):1989-91.
[21]Italiano CM,Wong KT,AbuBakar S,Lau YL,Ramli N,Syed Omar SF,et al.Sarcocystis nesbitti causes acute,relapsing febrile myositis with a high attack rate:description of a large outbreak of muscular sarcocystosis in Pangkor Island,Malaysia,2012.PLoS Negl Trop Dis 2014;8(5):e2876.
[22]Lau YL,Chang PY,Tan CT,Fong MY,Mahmud R,Wong KT. Sarcocystis nesbitti infection in human skeletal muscle:possible transmission from snakes.Am J Trop Med Hyg 2014;90(2):361-4.
[23]Mandour AM.Sarcocystis nesbitti n.sp.from the rhesus monkey. J Protozool 1969;16(2):353-4.
[24]Lau YL,Chang PY,Subramaniam V,Ng YH,Mahmud R,Ahmad AF,et al.Genetic assemblage of Sarcocystis spp.in Malaysian snakes.Parasit Vectors 2013;6:257.
[25]Tappe D,Abdullah S,Heo CC,Kannan Kutty M,Latif B.Review paper human and animal invasive muscular sarcocystosis in Malaysia-recent cases,review and hypotheses.Trop Biomed 2013;30(3):355-66.
[26]Pathmanathan R,Kan SP.Human Sarcocystis infection in Malaysia. Southeast Asian J Trop Med Public Health 1981;12:247-50.
[27]Pathmanathan R,Kan SP.Two cases of human sarcocystosis in East Malaysia.Med J Malays 1987;42(3):212-4.
[28]Pathmanathan R,Jayalakshmi P,Kan SP.A case of human muscular sarcocystosis in Malaysia.J Malays Soc Health 1988;6: 45-7.
[29]Pathmanathan R,Kan SP.Three cases of human Sarcocystis infection with a review of human muscular sarcocystosis in Malaysia.Trop Geogr Med 1992;44(1-2):102-8.
[30]Shekhar KC,Pathmanathan R,Krishnan R.Human muscular sarcocystosis associated with neoplasms?Case report.Trop Biomed 1998;15(2):61-4.
[31]Slesak G,Schafer J,Langeheinecke A,Tappe D.Prolonged clinical course of muscular sarcocystosis and effectiveness of cotrimoxazole among travelers to Tioman Island,Malaysia,2011-2014. Clin Infect Dis 2014;60(2):329.
[32]Esposito DH,Stich A,Epelboin L,Malvy D,Han PV,Bottieau E,et al.Acute muscular sarcocystosis:an international investigation among ill travelers returning from Tioman Island,Malaysia,2011-2012.Clin Infect Dis 2014;59(10):1401-10.
[33]Zaman V.Sarcocystis sp.in the slow loris,Nycticebus coucang. Trans R Soc Trop Med Hyg 1970;64(1):195-6.
[34]Kan SP,Prathap K,Dissanaike AS.Light and electron microstructure of a Sarcocystis sp.from the Malaysian long-tailed monkey,Macaca fascicularis.Am J Trop Med Hyg 1979;28(4):634-42.
[35]Kan SP.Ultrastructure of the cyst wall of Sarcocystis spp.from some rodents in Malaysia.Int J Parasitol 1979;9(5):475-80.
[36]Ambu S,Yeoh EYS,Mak JW,Chakravarthi S.Prevalence of Sarcocystis spp.in rodents in Peninsular Malaysia.Int e-J Sci Med Edu 2011;5(2):29-38.
[37]Latif B,Vellayan S,Omar E,Abdullah S,Mat Desa N.Sarcocystosis among wild captive and zoo animals in Malaysia.Korean J Parasitol 2010;48(3):213-7.
[38]Kan SP,Dissanaike AS.Studies on Sarcocystis in Malaysia.II. Comparative ultrastructure of the cyst wall and zoites of Sarcocystis levinei and Sarcocystis fusiformis from the water buffalo,Bubalus bubalis.Z Parasitenkd 1978;57(2):107-16.
[39]Dissanaike AS,Kan SP.Studies on Sarcocystis in Malaysia.I. Sarcocystis levinei n.sp.from the water buffalo Bubalus bubalis. Z Parasitenkd 1978;55(2):127-38.
[40]Dissanaike AS,Kan SP,Retnasabapathy A,Baskaran G.Developmental stages of Sarcocystis fusiformis(Railliet,1897)and Sarcocystis sp.,of the water buffalo,in the small intestines of cats and dogs respectively.Southeast Asian J Trop Med Public Health 1977;8(3):417.
[41]Latif B,Vellayan S,Heo CC,Kannan Kutty M,Omar E,Abdullah S,et al.High prevalence of muscular sarcocystosis in cattle and water buffaloes from Selangor,Malaysia.Trop Biomed 2013;30(4):699-705.
[42]Norlida O,Zarina M,LatifB,Abo R,Al-Sultan I. A histopathological appraisal of ovine sarcocystosis in Kelantan. J Adv Biomed Pathobiol Res 2012;2(4):137-42.
[43]Latif B,Kannan Kutty M,Muslim A,Hussaini J,Omar E,Heo CC,et al.Light microscopy and molecular identification of Sarcocystis spp.in meat producing animals in Selangor,Malaysia.Trop Biomed 2015;32(3):444-52.
[44]Kutty MK,Latif B,Muslim A,Hussaini J,Daher AM,Heo CC,et al. Detection of sarcocystosis in goats in Malaysia by light microscopy,histology,and PCR.Trop Anim Health Prod 2015;47(4):751-6.
[45]Ng YH,Fong MY,Subramaniam V,Shahari S,Lau YL.Short communication:genetic variants of Sarcocystis cruzi in infected Malaysian cattle based on 18S rDNA.Res Vet Sci 2015;103:201-4.
[46]Lindsay DS,Blagburn BL,Braund KG.Sarcocystis spp.and sarcocystosis.Br Med J 1995;5(3):249-54.
[47]Beaver PC,Maleckar JR.Sarcocystis singaporensis Zaman and Colley,(1975)1976,Sarcocystis villivillosi sp.n.,and Sarcocystis zamani sp.n.:development,morphology,and persistence in the laboratory rat,Rattus norvegicus.J Parasitol 1981;67(2):241-56.
[48]Lee SC,Ngui R,Tan TK,Muhammad Aidil R,Lim YA.Neglected tropical diseases among two indigenous subtribes in Peninsular Malaysia:highlighting differences and co-infection of helminthiasis and sarcocystosis.PLoS One 2014;9(9):e107980.
[49]Yang ZQ,Wei CG,Zen JS,Song JL,Zuo YX,He YS,et al. A taxonomic re-appraisal of Sarcocystis nesbitti(Protozoa:Sarcocystidae)from the monkey Macaca fascicularis in Yunnan,PR China.Parasitol Int 2005;54(1):75-81.
[50]Ng YH,Subramaniam V,Lau YL.Modified use of methylene blue in the tissue compression technique to detect sarcocysts in meatproducing animals.Vet Parasitol 2015;214(1-2):200-3.
[51]Poulsen CS,Stensvold CR.Current status of epidemiology and diagnosisofhumansarcocystosis.JClinMicrobiol2014;52(10):3524-30.
12 Apr 2016
in revised form 1 Aug,2nd
Review article http://dx.doi.org/10.1016/j.apjtb.2016.09.003
Azdayanti Muslim,Faculty of Medicine,University Teknologi MARA,Sungai Buloh Campus,Jalan Hospital,47000,Sungai Buloh,Selangor,Malaysia.
 Asian Pacific Journal of Tropical Biomedicine2016年11期
Asian Pacific Journal of Tropical Biomedicine2016年11期
- Asian Pacific Journal of Tropical Biomedicine的其它文章
- Therapeutic applications of collagenase(metalloproteases)∶A review
- Cytotoxic activity and phytochemical standardization of Lunasia amara Blanco wood extract
- Antiacanthamoebic properties of natural and marketed honey in Pakistan
- GC-MS analysis of bioactive compounds present in different extracts of an endemic plant Broussonetia luzonica(Blanco)(Moraceae)leaves
- Anti-nitric oxide production,anti-proliferation and antioxidant effects of the aqueous extract from Tithonia diversifolia
- Anthelmintic activity of Saba senegalensis(A.DC.)Pichon(Apocynaceae)extract against adult worms and eggs of Haemonchus contortus
