Diagnosis of neurocysticercosis among patients with seizures in northern coastal districts of Andhra Pradesh,India
Bala Chandra Sekhar Pappala,Jyothi Padmaja Indugula,Sateesh Kumar Talabhatula,Ramalakshmi Suryakarani Kolli,Arpit Kumar Shrivastava,Priyadarshi Soumyaranjan Sahu
1Department of Microbiology,Andhra Medical College,Visakhapatnam,Andhra Pradesh,India
2Great Eastern Medical School and Hospital,Srikakulam,Andhra Pradesh,India
3Department of Neurology,Andhra Medical College,Visakhapatnam,Andhra Pradesh,India
4Department of Microbiology,Rangaraya Medical College,Kakinada,E.G.,Andhra Pradesh,India
5Department of Biotechnology,School of Biotechnology and Kalinga Institute of Medical Sciences,KIIT University,Bhubaneswar,India
6Division of Pathology,School of Medicine,International Medical University,57000 Kuala Lumpur,Malaysia
Diagnosis of neurocysticercosis among patients with seizures in northern coastal districts of Andhra Pradesh,India
Bala Chandra Sekhar Pappala1,Jyothi Padmaja Indugula2,Sateesh Kumar Talabhatula3,Ramalakshmi Suryakarani Kolli4,Arpit Kumar Shrivastava5,Priyadarshi Soumyaranjan Sahu6*
1Department of Microbiology,Andhra Medical College,Visakhapatnam,Andhra Pradesh,India
2Great Eastern Medical School and Hospital,Srikakulam,Andhra Pradesh,India
3Department of Neurology,Andhra Medical College,Visakhapatnam,Andhra Pradesh,India
4Department of Microbiology,Rangaraya Medical College,Kakinada,E.G.,Andhra Pradesh,India
5Department of Biotechnology,School of Biotechnology and Kalinga Institute of Medical Sciences,KIIT University,Bhubaneswar,India
6Division of Pathology,School of Medicine,International Medical University,57000 Kuala Lumpur,Malaysia
ARTICLE INFO
Article history:
Accepted 12 Jun 2016
Available online 20 Sep 2016
Neurocysticercosis
Cysticercosis
Seizures
Andhra Pradesh
Objective:To report cases of neurocysticercosis(NCC)from three neighboring districts of Andhra Pradesh state in India where NCC burden was never explored before.
Methods:A total of 160 patients presenting with recent onset seizures were recruited from neurology,general medicine,and pediatric outpatient clinics of a local major tertiary care teaching hospital serving above districts during the period 2011-2014.Brain imaging was performed in all the above cases.A commercial immunoglobulin G-ELISA kit(sensitivity=85%;specificity=94%)was employed for the serological diagnosis of NCC.
Results:The recruited patients presented with generalized,simple partial,and complex partial seizures(55%,31.25%and 13.75%respectively).NCC was diagnosed in 44 of 160(27.5%)seizure cases based on imaging characteristics,and a positive serum antibody ELISA.No association was detected between seropositivity with the number and location of the lesion(s)in the brain.
Conclusions:The possible potentiality of NCC could be identified as an underlying cause of the recent onset of seizures in this region as explored in the present study.It is recommended that NCC should be suspected as one of the major differential in every recent onset seizure with or without a radio imaging supportive diagnosis,especially in areas endemic for taeniasis/cysticercosis.
1.Introduction
Thecentralnervoussystemisknowntobethemostcommonsite of infection with Taenia solium(T.solium)metacestode larvaecausing neurocysticercosis(NCC).This is a major public health problemintropicaldevelopingcountrieswhereitaffectspatientsof all ages[1].Human gets infected either by accidental ingestion of T.solium eggs through contaminated food/vegetables or due to endogenous autoinfection particularly in subjects who are carriers of the adult worm in their intestine;by either means,eggs containing the hexacanth larvae disseminate hematogenously to the brain developing into metacestode larvae or cysts[2].
Tel:+91 9438724729
E-mail:priyadarshi_sahu@yahoo.com
This study was carried out in accordance with the Code of Ethics of the World Medical Association(Declaration of Helsinki)approved by the Institutional Ethics Committee of Andhra Medical College,Vishakhapatnam,Andhra Pradesh,India. Informed written consent was obtained from each patient included in this study.
Foundation Project:Partially supported by the Indian Council of Medical Research Ad-hoc Research Grant(IRIS ID:2010-10530).
Peer review under responsibility of Hainan Medical University.The journal implements double-blind peer review practiced by specially invited international editorial board members.
The clinical manifestations of NCC are non-specific and varied,depending on the number of lesions as well as the developmental stage of the parasite.Seizures are the commonest manifestation,occurring in 50%-80%of patients[3,4].NCC is considered to be the single most common cause of epilepsy in the developing countries which are known to be endemic for T.solium taeniasis/cysticercosis[5,6].A recent meta-analysis summarizes the proportion of NCC among patients withepilepsy(PWE),and suggests that in endemic communities nearly one-third of PWE are living with T.solium cystic lesions in their brain[7].NCC was found to be associated with approximately one-third of all cases presenting with active epilepsy in either urban or rural regions as per a study reported from Vellore district of Tamil Nadu,India[8].The pleomorphic and unpredictable course of NCC could be related to either the parasite factors(viz.,biological stage and numbers)or the host immunogenetic factors[9].
2221-1691/Copyright©2016 Hainan Medical University.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
T.solium cysticercosis occurs in many resource-poor countries,especially those with warm and tropical climates of Latin America,Asia and Sub-Saharan Africa[10].NCC is a common chronic neurological disorder with sero-prevalence of 0.1%-6%in India and 0.02%-6%in China,Korea,Vietnam [11].In a recent Indian study,89.66%cases having neurological manifestations with inflammatory granulomas were found consistent with diagnosis of NCC[12].However,the serodiagnostic confirmation was not performed in those cases.There are many provinces where reports are still unavailable orscanty thereby underestimating its actual burden in this country[6].
The present study was done in Andhra Pradesh,a southern coastal state in India,previously known to be endemic for T.solium cysticercosis in pig and man where various forms of cysticercosis in man have been reported[13-16].However,no laboratory confirmed case was reported so far from the studied three neighboring districts(Visakhapatnam,Vizianagaram,Srikakulam).Either due to lack of a confirmatory diagnosis or unawareness about the necessity of its documentation,there was a lack of reported cases or notifications which probably had given the false impression about its low prevalence or rareness in this region.Keeping this into consideration,the present study was conducted with the objective to address the problem of NCC among cases of recent onset of seizures in the above three neighboring districts of Andhra Pradesh.In order to supplement the clinical suspicion of NCC,usefulness of a serological test detecting antibody by ELISA in addition to brain imaging is discussed.
2.Materials and methods
2.1.Patients
The present study was conducted in Andhra Medical College Hospital in Visakhapatnam,a major tertiary care healthcare establishment in the study area,serving the populations most commonly from Visakhapatnam,Vizianagaram and Srikakulam districts of Andhra Pradesh(Figure 1).A total of 160 patients were recruited in the present study.The majority of which were from neurology,general medicine,or pediatrics outpatient clinics of the above hospital during the period of 2011-2014,and rest were referral cases from other corporate hospitals in the same locality.Informed consent was obtained from patients or legal guardians of each of the study subjects. Detailed history was collected from patients and/or guardians and a routine clinical examination was conducted before to include them for this study.Screening of anti-cysticercus antibodies in serum was performed as stated in Section 2.4.All samples were analyzed in one laboratory employing same protocol.
2.1.1.Inclusion criteria
Seizure patients clinically and/or radiologically suspected to be NCC,withinagerangeof3-65years,andlivinginanyoftheabove three districts of Andhra Pradesh for at least a year were included.
2.1.2.Exclusion criteria
Patients not living in the study area for a year or short term tourists/visitors,of age range either<2 years or>65 years,suspected female patients with detection of underlying pregnancy were excluded.Also patients having past history of head injury,symptoms of febrile seizures in children,recent history of any other chronic disease excluded from the present screening study.
2.2.Brain imaging
Brain imaging by CT or magnetic resonance imaging(MRI)was performed in all cases.The study subjects were initially hypothesized as possible cases of NCC based on two minor plus one epidemiological criterion as per the revised diagnostic criteria suggested by Del Brutto[1].
2.3.Specimen
Under aseptic precautions,3 mL of venous blood was collected from all the recruited patients upon written consent. The collected whole blood sample from each case was allowed to clot at room temperature.The serum was separated and then stored in pair at-80°C till use.
2.4.T.solium immunoglobulin G(IgG)ELISA in serum
A commercially procured ELISA Kit(NovaTec Diagnostics,Germany)was employed for detection of anti-cysticercus IgG antibodies in sera from all the recruited cases following manufacturer's instructions.Briefly,antigen coated wells supplied by the kit manufacturer were incubated with 1:10 diluted patient/ control serum(diluted with the serum diluent fluid provided inthe kit).A negative control serum,a cut-off control serum and a positive control serum(all reagents supplied by the manufacturer)were also used for validity of the test.Absorbance was measured at 450 nm.A sample was considered positive for anti-T.solium antibody when the optical density value was estimated to be more than that of the low positive control serum.The sensitivity and specificity of the above ELISA for anticysticercus antibody detection in serum were previously estimated to be 85%and 94%respectively based on results of the test using sera from a group of known cases(cases with a definitive diagnosis of NCC)and another group comprising healthy normal individuals as described in an earlier study[17].
3.Results
In this study,a total of 55%cases presented with generalized seizures,whereas the seizure type was simple partial and complex partial in 31.25%and 13.75%of cases,respectively(Table 1). The two-tailed P value was calculated to be equivalent to 0.7235 when the seropositivity results were analyzed comparing two groups of patients who presented either with generalized or partial seizures(simple and complex partial seizures combined).
Based on CT and/or MRI findings,85 seizure patients had solitary lesion in brain.A total of 75 had multiple lesions which included 37 cases with 2-4 lesions,and 38 with>4 lesions(Table 2).The association between seropositivity for NCC,and the number of lesions in brain was found to be not statistically significant since the two-tailed P value was estimated to be 0.4786.

Table 1Results of the anti-cysticercus IgG-ELISA in seizure patients with different type of seizure.
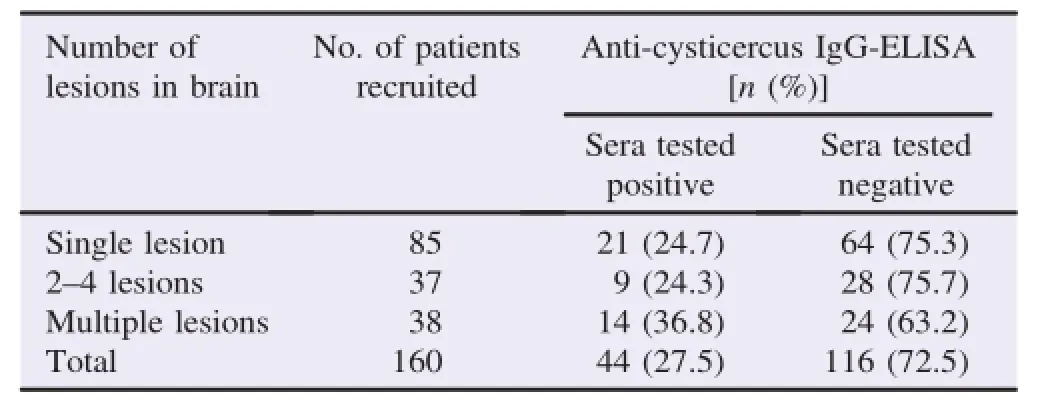
Table 2Results of the anti-cysticercus IgG-ELISA in seizure patients with respect to CT and MRI scan imaging features.
The distribution of lesions in various parts of brain is presented in Table 3.In this series,the lesions were most common in parietal lobe followed by frontal lobe,occipital,temporal lobes and other regions like basal ganglia,ventricles etc.However,percentage of seropositive cases was comparable.Presence of either single or multiple lesions and characteristics of lesions are presented in Table 4.In this series,majority had granular nodular cysts with inflammation(17 cases single+8 cases multiple=total 25 cases).Only calcified cysts were seen in a total of 7 cases(i.e.2 cases with single lesion+5 cases with>1 lesions)and single vesicular lesions in 2 cases.The age range of these cases was found to be between 4 and 65 years and there were 60%males and 40%females.
In serological analysis,total 27.5%of patients were found positive for anti-cysticercus IgG antibodies.Among the positive sera tested,26.1%had generalized seizures,32.0%had simple partial seizures and 22.7%had complex partial seizures(Table 1).Among other complaints of these seropositive patients,headache was major complaint accounting for 30.7%,vomiting 40%,hemiparesis 36.4%,muscle weakness 33.3%and altered sensorium 28.6%(Figure 2).
In this study,24.7%of seropositive cases had single lesion,24.3%had 2-4 lesions and 36.8%had multiple lesions(Table 2).In this screening study,CT and/or MRI scan revealed presence of lesions in all seropositive cases.Among these seropositive cases,27.9%of lesions were seen in the parietal lobe,28.1%in the frontal lobe and fronto-parietal lobes,15.0% in occipital and parieto-occipital lobes,34.3%in all regions and 25.0%in other parts of the brain(Table 3).Further characteristics of the brain lesions are shown in Table 4.In this series,majority had granular nodular lesions with active perilesional inflammation around either single(17 cases)or multiple(8 cases)lesions(total 25 cases);calcified cysts in 7 cases and vesicular stage in 2 cases were also detected.Among the seropositive cases,10 cases had multiple cysts with different stages of development.
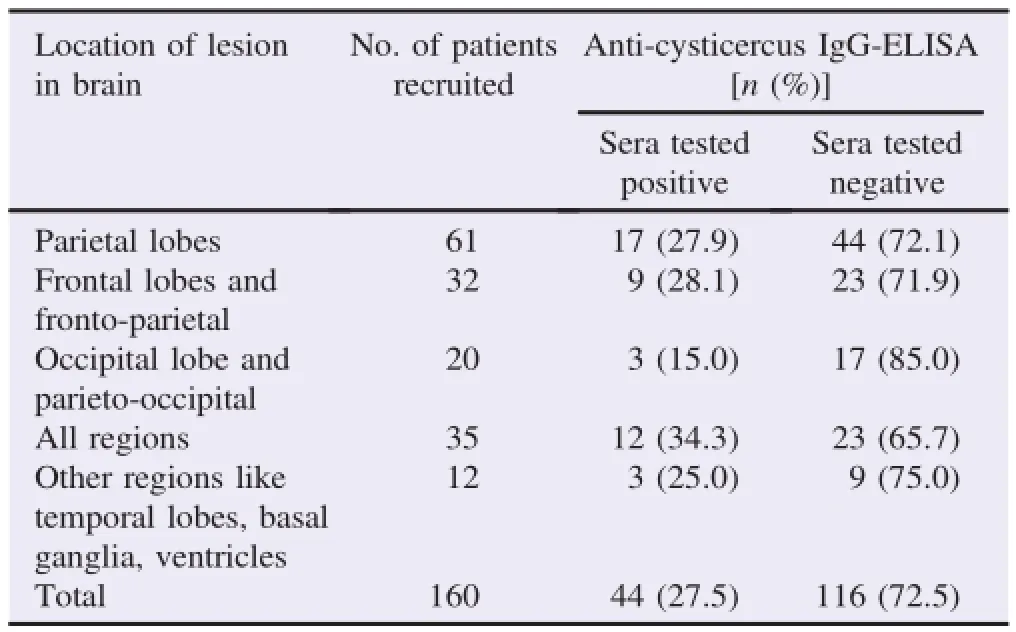
Table 3Results of the anti-cysticercus IgG-ELISA in seizure patients with respect to location of lesions in the brain.
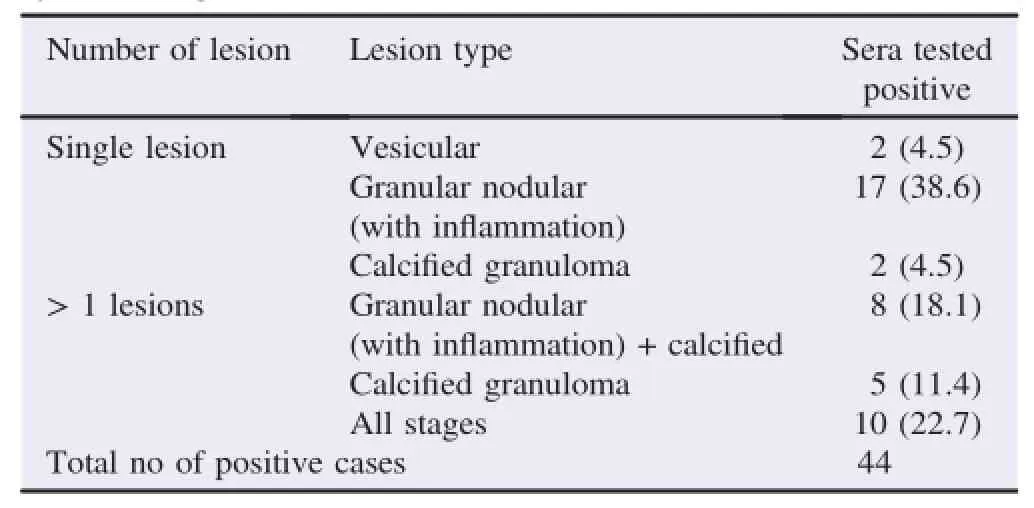
Table 4Type or stage of the lesion in the cases tested positive by the anticysticercus IgG-ELISA[n(%)].

Figure 2.Distribution of clinical signs/symptoms,and seizure pattern in afebrile seizure cases diagnosed to be positive for anti-cysticercus IgG-ELISA vs. all the recruited cases.
In this study,70.45%of seropositive cases were identified to be from low socioeconomic background,and 29.55%were from high socioeconomic background.Of these,68.1%were residing in rural areas and 31.8%were residing in urban area.In 44 seropositive cases,45.45%had history of pork consumption.
4.Discussion
NCC is considered to be a major public health problem in India.NCC has been suspected as a major definable risk of epilepsy in this country[18].However,information about its prevalence is either lacking or incompletely recorded even if the whole country is assumed to be highly endemic for T.solium taeniasis/cysticercosis.The north coastal districts of Andhra Pradesh were never explored before.This is the first ever study in these three neighboring districts of Andhra Pradesh where the proportion of PWE suffering from NCC is estimated and also the possible associated factors are discussed here.For the first time,a series of cases from the hospital-based screening,as in this study,revealed more than one fourth of the total number of cases presenting with seizures due to the NCC that was evident based on the serum antibody reactivity as well as CT/MRI brain findings compatible with it.Therefore,by detection of anticysticercus IgG antibodies in serum,the possible potentiality of NCC can be identified as an underlying cause of the recent onset of seizures in this region.There were few earlier studies from other Indian provinces which showed similar levels of occurrence of cysticercosis as a cause of acquired seizure[19].
The result of the present study was similar to most of the other studies reported earlier.In our study,majority of the seizure cases were in pediatric age group in contrast to adults. Researchers from other parts have also reported more cases in pediatric age group[20-23].Parija and Raman reported predominance between 16 and 48 age group[22].In an earlier study,the predominant age group was found to be ranging between 30 and 49 years[24].In the study of Kotokey et al.,the predominant age group was between 21 and 30[25]. Whereas,other two recent studies reported the predominant age group as 10-65 and 8-60,respectively[26,27].
In present study,females were predominant than males with percentage of 34.4%.In an earlier study,females were reported to be predominant(58%)than males[20].In other studies,also males were predominant than females[21,23].In some other studies,also males were diagnosed predominantly accounting 53%-95%in different regions[24,26,27].
Predominance of type of seizures in seropositive NCC patients in different studies shows generalized seizures are more commonly than the partial seizures.In present study,simple partial seizures are predominant with 31.25%.In other studies,also generalized seizures were the predominant type[20,21,23,27]. Hence,the result of present study was contradictory to most of the other studies reported earlier.
In the present study,headache is predominant followed by vomiting,hemiparesis,muscle weakness and altered sensorium. In our earlier studies[16,23],headache was predominant followed by vomiting,pallor,altered sensorium,and muscle weakness. Headache was predominant followed by mental retardation,and psychiatric symptoms in another study reported elsewhere[21].Similarly,headache was also predominant accounting for 15.6%as documented from another recent study[28].
In the present study,multiple lesions in all regions of brain are predominant with percentage of 36.8%and 34.33%,respectively. In other similar studies,multiple lesions in parietal regions were predominant with 42.85%and 34.32%,respectively[23].Thus,results of the present study were similar to other studies reported earlier.
In this case series,the granular nodular lesions with inflammation were predominant with percentage of 38.6%.In a recent study from Odisha,a state neighboring to Andhra Pradesh,calcified cysts were predominant,accounting for 47.06%of the total patients diagnosed to be NCC[23].In other studies,either mixed lesions,or immunologically active lesions were reported to be predominant[29,30].Hence,the results of our study were found to be in accordance with findings from other Indian studies.
In the present study,45.4%of seropositive cases have history of pork consumption.In other studies,91.3%of seropositive cases had a history of pork consumption[26].This may be due to cultural differences or difference in dietary habits of populations in different parts of the world.
Both,NCC and epilepsy,are an increasing burden on the welfare and economy of developing countries[5,31].In the present study,70.4%of seropositive cases belong to low socioeconomic status,i.e.yearly income<2 lakhs and 29.6% belong to high socioeconomic status.The results of presentstudy are similar to the study of Kirmani et al.in which 89% belong to low socioeconomic status and 11.1%belong to high socioeconomic status[28].Similar findings were also reported from an epidemiological study report from the incidences in a recent study from Malaysia[32].
In the present study,68.1%belong to rural area and 31.9% belongtourbanareawhichcoincideswiththestudyofKirmanietal. inwhich60%belongtoruralareaand40%belongtourbanarea[28]. In an earlier study from a rural medical college hospital in Andhra Pradesh,18 cases of cysticercus cellulose at rare sites were reported.Out of total 18,15 cases had parasite located in the subcutaneous tissue of chest wall,breast,left lumbar region,umbilicus,abdominal wall,back,extremities,and neck region;there were 2 cases with cysticercus larvae in eye and 1 case had a cyst detected in the oral cavity[13].There was a case of orbital cysticercosis in Vishakhapatnam where a small cysticercus cyst of the superior rectus muscle was detected by CT[33].Cysticercosis in eye has been also reported from various other locations in Andhra Pradesh including the latest report of a retrobulbar optic nerve cysticercosis[34].
Nevertheless,the prevalence of anti-cysticercus antibodies detected in sera from the present series of cases with seizure may not be the true picture if the figures are extrapolated to a larger population in the same territory or even the whole province of Andhra Pradesh in India.The commercially procured ELISA kit detects antibodies against antigens of the parasite which are not defined or not declared by the manufacturer as stated earlier[23]. Therefore,further study screening antibodies specific to more defined antigens of the larval parasite might result in different prevalence scenario.
Management of NCC needs to be individualized as recommended elsewhere[35].Recent literatures emphasize the need for focused and targeted programs which also encourage for stronger public health approach based on equity for prevention,control,and management of epilepsy in India[36].
This is the first hospital-based report of a series of NCC cases from three neighboring districts of Andhra Pradesh in India where the burden of seizures due to NCC was never explored before.In our study,NCC is found to be more common in females with low socioeconomic status living in rural area with partial seizures. Detectinganti-cysticercusIgGantibodiesinserumcouldrevealthe potentialityofpossibleNCCasanunderlyingcauseofrecentonset seizuresinthestudiedcases.Although,theCT/MRIscanisapotent diagnostic tool compared to antibody detection,the diagnostic decision can be better made if both the modalities are considered together.However,itisrecommendedtosuspectNCCasoneofthe majordifferential,andsoitshouldberuledoutineveryrecentonset seizure case,with or without an imaging based supportive diagnosis,especially in the regions which are endemic for T.solium taeniasis/cysticercosis.
Conflict of interest statement
We declare that we have no conflict of interest.
Acknowledgments
The authors acknowledge the hospital authority of Andhra Medical College Hospital in Visakhapatnam for administrative support to conduct this study.This work was partially supported by the Indian Council of Medical Research Ad-hoc Research Grant(IRIS ID:2010-10530)awarded to Priyadarshi Soumyaranjan Sahu at School of Biotechnology and Kalinga Institute of Medical Sciences,Kalinga Institute of Industrial Technology University,Bhubaneswar.
References
[1]Del Brutto OH.Diagnostic criteria for neurocysticercosis,revisited. Pathog Glob Health 2012;106(5):299-304.
[2]Parija SC,Balamurungan N,Sahu PS,Subbaiah SP.Cysticercus antibodies and antigens in serum from blood donors from Pondicherry,India.Rev Inst Med Trop Sao Paulo 2005;47: 227-30.
[3]Flisser A.Taeniasis and cysticercosis due to Taenia solium.Prog Clin Parasitol 1994;4:77-116.
[4]Medina MT,DeGiorgio C.Introduction to neurocysticercosis:a worldwide epidemic.Neurosurg Focus 2002;12:6.
[5]Singh BB,Khatkar MS,Gill JP,Dhand NK.Estimation of the health and economic burden of neurocysticercosis in India.Acta Trop 2016;http://dx.doi.org/10.1016/j.actatropica.2016.01.017.
[6]Prasad KN,Prasad A,Verma A,Singh AK.Human cysticercosis and Indian scenario:a review.J Biosci 2008;33:571-82.
[7]Ndimubanzi PC,Carabin H,Budke CM,Nguyen H,Qian YJ,Rainwater E,et al.A systematic review of the frequency of neurocyticercosis with a focus on people with epilepsy.PLoS Negl Trop Dis 2010;4:e870.
[8]Rajshekhar V,Raghava MV,Prabhakaran V,Oommen A,Muliyil J. Active epilepsy as an index of burden of neurocysticercosis in Vellore district,India.Neurology 2006;67:2135-9.
[9]Kashyap B,Das S,Jain S,Agarwal A,Kaushik JS,Kaur IR.Correlationbetweentheclinicoradiologicalheterogeneityandtheimmuneinflammatory profiles in paediatric patients with neurocysticercosis from a tertiary referral centre.J Trop Pediatr 2012;58:320-3.
[10]Wu HW,Ito A,Ai L,Zhou XN,Acosta LP,Lee Willingham A III. Cysticercosis/taeniasis endemicity in Southeast Asia:current status and control measures.Acta Trop 2016;http://dx.doi.org/10.1016/ j.actatropica.2016.01.013.
[11]Rajshekhar V,Joshi DD,Doanh NQ,van De N,Xiaonong Z.Taenia solium taeniosis/cysticercosis in Asia:epidemiology,impact and issues.Acta Trop 2003;87:53-60.
[12]Balaji JD,Meikandan D.Clinical and radiological profile of neurocysticercosis in South Indian children.Indian J Pediatr 2011;78:1019-20.
[13]Gole S,Gole G,Satyanarayana V,Deshpande A,Tati S.Cysticercosis at rare sites:our experience at a rural medical college in Andhra Pradesh,India.Internet J Parasit Dis 2012;5(1):1-9.
[14]Sreedevi C,Hafeez M,Kumar PA,Rayulu VC,Subramanyam KV,Sudhakar K.PCR test for detecting Taenia solium cysticercosis in pig carcasses.Trop Anim Health Prod 2012;44(1):95-9.
[15]Yashodhara P,Elizabeth B.Clinical profile of childhood neuro cysticercosis.Int J Sci Res 2015;4:1963-6.
[16]Sahu PS,Seepana J,Padela S,Sahu AK,Subbarayudu S,Barua A. Neurocysticercosis in children presenting with afebrile seizure: clinical profile,imaging and serodiagnosis.Rev Inst Med Trop Sao Paulo 2014;56:253-8.
[17]Sahu PS,Parija SC,Narayan SK,Kumar D.Evaluation of an IgGELISA strategy using Taenia solium metacestode somatic and excretory-secretory antigens for diagnosis of neurocysticercosis revealing biological stage of the larvae.Acta Trop 2009;110:38-45.
[18]Raina SK,Razdan S,Pandita KK,Sharma R,Gupta VP,Razdan S. Active epilepsy as indicator of neurocysticercosis in rural Northwest India.Epilepsy Res Treat 2012;2012:802747.
[19]Udani V.Paediatric epilepsy-an Indian perspective.Indian J Pediatr 2005;72:309-13.
[20]Foyaca-Sibat H,Cowan LD,Carabin H,Targonska I,Anwary MA,Serrano-Ocaña G,et al.Accuracy of serological testing for the diagnosis of prevalent neurocysticercosis in outpatients with epilepsy,Eastern Cape Province,South Africa.PLoS Negl Trop Dis 2009;3:e562.
[21]Blocher J,Schmutzhard E,Wilkins PP,Gupton PN,Schaffert M,Auer H,et al.A cross sectional study of people with epilepsy andneurocysticercosis in Tanzania:clinical characteristics and diagnostic approaches.PLoS Negl Trop Dis 2011;5(6):e1185.
[22]Parija SC,Raman GA.Anti-Taenia solium larval stage IgG antibodies in patients with epileptic seizures.Trop Parasitol 2011;1: 20-5.
[23]Sahu PS,Patro S,Jena PK,Swain SK,Das BK.Imaging and serological-evidence of neurocysticercosis among patients with seizures in Odisha,an unexplored eastern coastal province in India. J Clin Diagn Res 2015;9:DC06-10.
[24]Sutisna IP,Fraser A,Kapti IN,Rodriguez-Canul R,Puta Widjana D,Craig PS,et al.Community prevalence study of taeniasis and cysticerosis in Bail,Indonesia.Trop Med Int Health 1999;4:288-94.
[25]Kotokey RK,Lynrah KG,De A.A clinico-serological study of neurocysticercosis in patients with ring enhancing lesions in CT scan of brain.J Assoc Physicians India 2006;54:366-70.
[26]Rottbeck R,Nshimiyimana JF,Tugirimana P,D¨ull UE,Sattler J,Hategekimana JC,et al.High prevalence of cysticercosis in people with epilepsy in Southern Rwanda.PLoS Negl Trop Dis 2013;7(11):e2558.
[27]Elliott I,Jerome A,Angwafor SA,Smith ML,Takougang I,Noh J,et al.Epilepsy and cysticercosis in North-West Cameroon:a serological study.Seizure 2013;22:283-6.
[28]Kirmani S,Khan HM,Khalid M,Urfi.Sensitivity of IgG ELISA for diagnosing neurocysticercosis in a tertiary care hospital of North India.Int J Curr Microbiol Appl Sci 2014;3:673-9.
[29]Ishida MM,Peralta RH,Livramento JA,Hoshino-Shimizu S,Peralta JM,Vaz AJ.Serodiagnosis of neurocysticercosis in patients with epileptic seizure using ELISA and immunoblot assay.Rev Inst Med Trop Sao Paulo 2006;48:343-6.
[30]Bueno EC,Vaz AJ,Machado LR,Livramento JA,Avila SL,Ferreira AW.Antigen-specific suppression of cultured lymphocytes from patients with neurocysticercosis.Clin Exp Immunol 2001;126:304-10.
[31]Gulati S,Jain P,Sachan D,Chakrabarty B,Kumar A,Pandey RM,et al.Seizure and radiological outcomes in children with solitary cysticercous granulomas with and without albendazole therapy:a retrospective case record analysis.Epilepsy Res 2014;108:1212-20.
[32]Sahu PS,Romano N,Lim YAL,Rohela M.Serological evidence of possible Taenia solium larval infection in Orang Asli communities of Malaysia.Trop Biomed 2016;33:170-9.
[33]Meena M,Bhatia K.Smart phone as an adjunctive imaging tool to visualize scolex in orbital myocysticercosis.Int Ophthalmol 2013;33(3):319-21.
[34]Narra R,Jukuri JN,Kamaraju SK.Retrobulbar optic nerve cysticercosis.J Glob Infect Dis 2015;7(3):122-3.
[35]Singhi P.Neurocysticercosis.Ther Adv Neurol Disord 2011;4(2): 67-81.
[36]Amudhan S,Gururaj G,Satishchandra P.Epilepsy in India I: epidemiology and public health.Ann Indian Acad Neurol 2015;18(3):263-77.
7 Jan 2016
inrevisedform23Feb2016
Original article http://dx.doi.org/10.1016/j.apjtb.2016.09.001
Dr.PriyadarshiSoumyaranjan Sahu,Assistant Professor,Division of Pathology,School of Medicine,International Medical University,57000 Kuala Lumpur,Malaysia.
 Asian Pacific Journal of Tropical Biomedicine2016年11期
Asian Pacific Journal of Tropical Biomedicine2016年11期
- Asian Pacific Journal of Tropical Biomedicine的其它文章
- Human and animal sarcocystosis in Malaysia∶A review
- Therapeutic applications of collagenase(metalloproteases)∶A review
- Cytotoxic activity and phytochemical standardization of Lunasia amara Blanco wood extract
- Antiacanthamoebic properties of natural and marketed honey in Pakistan
- GC-MS analysis of bioactive compounds present in different extracts of an endemic plant Broussonetia luzonica(Blanco)(Moraceae)leaves
- Anti-nitric oxide production,anti-proliferation and antioxidant effects of the aqueous extract from Tithonia diversifolia
