沧州地区儿童乳糖酶缺乏现状与体格发育关系的研究
吴 昱,岳 彬
(沧州市中心医院儿内一科,河北 沧州 061000)
沧州地区儿童乳糖酶缺乏现状与体格发育关系的研究
吴昱,岳彬
(沧州市中心医院儿内一科,河北 沧州 061000)
[摘要]目的探讨沧州地区儿童乳糖酶缺乏的现状及其与体格发育的关系。方法选取2015年1月至2016年2月来沧州市中心医院门诊体检的210名3~14岁儿童为研究对象,按年龄段分为3~5岁组(125例,男性32例,女性93例)、6~10岁组(49例,男性38例,女性11例)以及11~14岁组(36例,男性24例,女性12例)。乳糖酶采用JY-po-color Gal尿半乳糖测定方法,分析不同年龄段乳糖酶缺乏的检出率,并对同年龄段组间的骨密度和骨钙蛋白进行比较。结果在210名儿童中乳糖酶缺乏检出率3~5岁组为52.0%,6~10岁组为65.3%,10~14岁组为83.3%,不同年龄组间检出率存在显著性差异,随着年龄的增长检出率呈逐渐升高趋势(χ2=32.984,P<0.05);农村儿童乳糖酶缺乏检出率显著高于城市儿童(χ2=29.621,P<0.05);不同性别间儿童乳糖酶缺乏检出率未见显著性差异(χ2=0.144,P>0.05)。乳糖缺乏与正常儿童每日饮奶量、饮奶率比较均有显著性差异(t值分别为15.845、11.363,均P<0.05)。与同年龄组乳糖酶正常儿童相比,乳糖酶缺乏者的骨钙蛋白和骨密度均显著降低(χ2值分别为4.354、5.041、4.861;2.836、3.845、2.983,均P<0.05)。结论乳糖酶缺乏症会造成儿童规避饮奶或饮奶后出现腹泻、腹痛等症状,造成奶制品中营养物质流失,对儿童生长发育带来不良影响。
[关键词]沧州;儿童;乳糖酶缺乏;体格发育
牛奶是儿童断母乳后的重要食物,几乎含有除膳食纤维外人体所需要的全部营养物质。乳糖是牛奶和奶制品中一种特有的双糖,进入机体内可被水解为半乳糖及葡萄糖而被吸收。肠道乳糖酶活性低下或含量减少称为乳糖酶缺乏(laetasedefieieney,LD)[1]。正常人群中普遍存在LD,此时会造成乳糖代谢障碍,可产生多种气体及短链脂肪酸,引发乳糖不耐受反应,如腹胀、腹鸣、排气增多等表现,是婴幼儿难治性腹泻病因之一,对患儿生长发育带来影响[2]。本研究通过观察沧州地区健康体检儿童饮奶后尿半乳糖检测结果及有无腹部症状,以了解该地儿童乳糖酶缺乏情况,并对乳糖酶缺乏与儿童体格发育关系进行分析。
1对象与方法
1.1一般资料
选取2015年1月至2016年2月来沧州市中心医院门诊体检的210名3~14岁儿童为研究对象,所有对象均无明显急性胃肠道症状。排除1周内有服药史及胃肠道疾病史。将210名儿童按年龄段分为3~5岁组(125例,男性32例,女性93例)、6~10岁组(49例,男性38例,女性11例)及11~14岁组(36例,男性24例,女性12例)。
1.2方法
通过自制问卷调查了解儿童基本情况、健康状况、既往病史、饮奶种类和数量及饮奶后有无胃肠道不适症状,比较不同年龄段儿童饮奶量。按儿童体重给予饮用市售纯牛奶10mL/kg(最多250mL),收集饮用牛奶后2~3小时尿液样本,采用JY-po-color Gal尿半乳糖测定方法,分析不同年龄段乳糖酶缺乏的检出率,并对同年龄段组间的骨密度和骨钙蛋白进行比较。试剂盒由北京中生金域诊断技术有限公司提供。
1.3统计学方法
2结果
2.1儿童饮奶量情况
随着年龄段的增长,农村和城市儿童每日饮奶量均显著下降(均P<0.05);且城市儿童饮奶量均显著高于农村儿童(均P<0.05),见表1。

Table 1 Comparison of daily average milk intake among children in Cangzhou ±S)
2.2儿童乳糖酶缺乏情况
在210名儿童中,乳糖酶缺乏检出人数127名,占60.5%;3~5岁年龄组检出率为52.0%,6~10岁年龄组检出率为65.3%,10~14岁年龄组检出率为83.3%;不同年龄组间检出率存在显著性差异,随年龄增长检出率呈逐渐升高趋势(P<0.05);农村儿童检出率显著高于城市儿童(P<0.05);不同性别间儿童乳糖酶缺乏检出率未见显著性差异(P>0.05),见表2。
2.3乳糖缺乏和正常儿童每日饮奶量及饮奶率情况
乳糖缺乏者每日饮奶量平均为(83.8±21.9)mL,饮奶率为(1.8±0.6)次/日;正常者每日饮奶量平均为(142.3±31.6)mL,饮奶率为(2.9±0.8)次/日。乳糖缺乏与正常儿童每日饮奶量、饮奶率比较有显著性差异(t值分别为15.845、11.363,均P<0.05)。
2.4乳糖酶缺乏与儿童骨代谢之间的关系
与同年龄组乳糖酶正常儿童相比,乳糖酶缺乏者的骨钙蛋白和骨密度均显著降低(均P<0.05),见表3。
表2不同区域、性别、年龄儿童乳糖酶缺乏的检出率比较结果[n(%)]
Table 2 Comparison of the detection rate of lactase deficiency among different regions, genders, and age groups [n(%)]
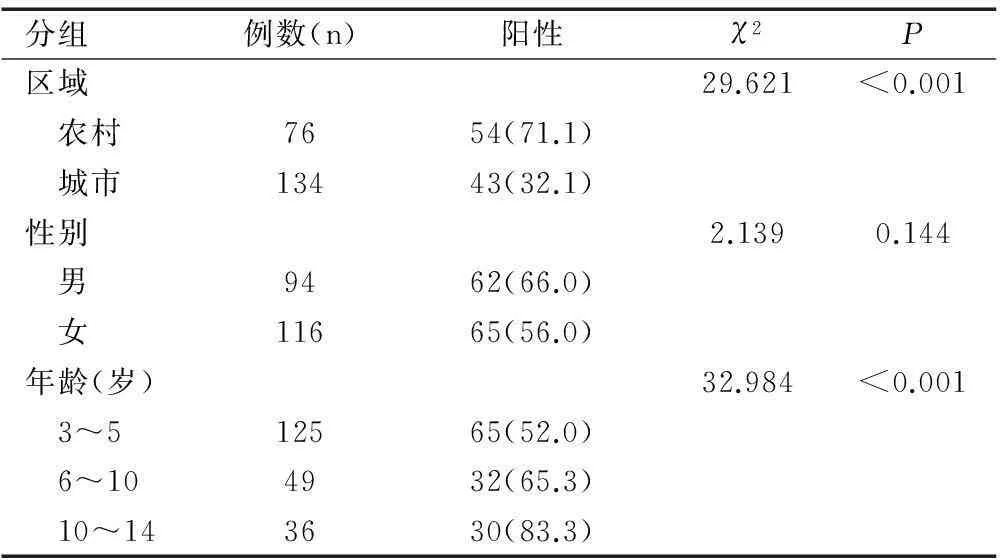
分组例数(n)阳性χ2P区域29.621<0.001 农村7654(71.1) 城市13443(32.1)性别2.1390.144 男9462(66.0) 女11665(56.0)年龄(岁)32.984<0.001 3~512565(52.0) 6~104932(65.3) 10~143630(83.3)

表3 乳糖酶缺乏与儿童骨代谢之间关系比较结果±S)
3讨论
3.1我国学龄前儿童乳糖酶缺乏情况
随着我国经济发展和生活水平的提高,每天喝1杯牛奶己被人们所接受。然而由于乳糖酶缺乏症的高发病率造成了许多儿童饮用牛奶或使用奶制品后出现腹泻、消化不良、腹痛、腹胀等消化道症状,造成营养物质的流失,牛奶的利用率下降,甚至很多人为此规避牛奶及奶制品,造成许多营养问题[3]。尤其对儿童而言,乳糖酶缺乏会给其体格发育带来严重的影响。有报道显示,不同民族中学生的乳糖缺乏发生率不同,藏族中学生乳糖酶缺乏发生率为70%,而汉族中学生则为96.7%,二者存在显著性差异[4]。乳糖酶缺乏的发生亦随年龄的不同而存在差异。据报道,随着年龄的增长,我国儿童乳糖酶缺乏的发生率逐渐升高,二者呈正相关关系[5]。在调查北京、上海、广州和哈尔滨年龄为3~13岁的1 168名儿童后,得到7~13岁儿童乳糖酶缺乏发生率为88%,而3~5岁者为38%,存在明显差异性。儿童乳糖酶的消失或降低多发生于7~8岁[6]。据报道上海地区0~6岁儿童乳糖吸收不良的发生率为47.4%,乳糖不耐受发生率16.5%,其发生率随着儿童年龄增加而上升,且乳糖酶的缺乏与儿童体格发育及营养性疾病的发生有一定的关系[7]。以上结果均提示,我国学龄儿童多数存在乳糖酶缺乏。本研究中,210名儿童乳糖酶缺乏检出人数为127名,占60.5%;3~5岁年龄组检出率为52.0%,6~10岁年龄组检出率为65.3%,10~14岁年龄组检出率为83.3%;不同年龄组间检出率存在显著性差异,且随年龄增长检出率呈逐渐升高趋势(P<0.05);农村儿童检出率显著高于城市儿童(P<0.05),与之前报道相一致。
3.2乳糖酶缺乏的危害性
本研究发现,乳糖缺乏儿童每日平均饮奶量和饮奶率均低于正常儿童,两组比较均有显著性差异(均P<0.05)。乳糖酶缺乏与儿童骨代谢及体格发育有相关性。本研究显示,与同年龄组乳糖酶正常儿童相比,乳糖酶缺乏者的骨钙蛋白与骨密度均显著降低(均P<0.05)。乳糖不耐受症儿童会刻意避免饮用牛奶及奶制品,从而影响了儿童营养物质及钙的摄取。乳糖酶缺乏儿童虽然不会刻意避免饮奶及奶制品,但乳糖酶缺乏导致牛奶营养成分不能充分消化吸收,乳糖在肠管内堆积,引起肠道排空加快,渗透压增加,进一步影响其他营养物质的消化吸收,造成钙、锌、铁等重要元素吸收障碍,对儿童营养状况及体格发育带来不良影响。
综上所述,乳糖酶缺乏症会造成儿童规避饮奶,或饮奶后出现腹泻、腹痛等症状,造成营养物质流失,不利于儿童的生长发育。因此,早期诊断儿童乳糖酶缺乏,及早进行有效干预,采用适当的饮奶方法,对我国儿童的体格健康发展具有重要意义。
[参考文献]
[1]Kuchay R A,Anwar M,Thapa B R,etal.Correlation of G/A -22018 single-nucleotide polymorphism with lactase activity and its usefulness in improving the diagnosis of adult-type hypolactasia among North Indian children[J].Genes and Nutrition,2013,8(1):145-151.
[2]杨欢欢,李菁.早产儿乳糖不耐受的诊疗进展[J].中国新生儿科杂志,2013,28(3):209-212
[3]Choi B J, Yoon J H, Choi Y J,etal.No association of LCT-13910 single nucleotide polymorphism with gastroenteritis in Korean children[J].Molecular & Cellular Toxicology,2013,9(1):23-28.
[4]陆茹,刁志英,徐小祥.乳糖酶治疗婴幼儿急性腹泻继发乳糖不耐受疗效观察[J].儿科药学杂志,2013,19(2):23-25.
[5]曹秀莉.乳糖不耐受患儿的营养干预临床观察[J].山西医药杂志,2011,40(4):417-418.
[6]Malek A J, Klimentidis Y C, Kell K P,etal.Associations of the lactase persistence allele and lactose intake with body composition among multiethnic children[J].Genes and Nutrition,2013,8(5):487-494.
[7]Hill I D.50 years ago in the journal of pediatrics:disaccharidase deficiencies with steatorrhea[J]. Journal of Pediatrics,2014,164(1):71.
[专业责任编辑:潘凯丽]
[收稿日期]2016-03-18
[作者简介]吴昱(1977-),男,主治医师,硕士,主要从事儿童消化系统疾病及儿童内分泌疾病的研究。
[通讯作者]岳彬,主任医师。
doi:10.3969/j.issn.1673-5293.2016.07.003
[中图分类号]R725.8
[文献标识码]A
[文章编号]1673-5293(2016)07-0796-03
Correlation between children’s lactase deficiency and their physical development in Cangzhou district
WU Yu, YUE Bin
(First Medical Department, Cangzhou Central Hospital, Hebei Cangzhou 061000, China)
[Abstract]Objective To explore the correlation between children’s lactase deficiency (LD) and their physical development in Cangzhou district. Methods A total of 210 children aged from 3 to 14 were chosen as research objects. All these children received physical examination at Cangzhou Central Hospital from January 2015 to February 2016. They were divided into 3-5 year-old group (125 cases including 32 males and 93 females), 6-10 year-old group (49 cases, including 38 males and 11 females) and 11-14 years old group (36 cases including 24 males and 12 females). As for LD patients, JY-po-color Gal of urinary galactose method was adopted and the detection rate of LD at different age groups was analyzed. Besides, comparison of bone mineral density and osteocalcin of patients within same age group was conducted. Results Among 210 children, the detection rate of LD in 3-5 year-old group, 6-10 year-old age group and 10-14 year-old group was 52.0%, 65.3% and 83.3%, respectively. Significant differences were identified in the detection rate among different age groups. With the increase of age, the detection rate increased (χ2=32.984, P<0.05). The detection rate of LD was significantly higher in children living in rural areas than that of the children in urban areas (χ2=29.621, P<0.05). No significant difference was found in the detection rate of LD between children of different genders (χ2=0.144,P>0.05). Remarkable differences were noticed between children with LD and healthy children in the volume and frequency of daily milk intake (t value was 15.845 and 11.363, respectively, both P<0.05). The osteocalcin and bone mineral density of LD children were significantly lower than those of healthy children (χ2 value was 4.354, 5.041, 4.861; 2.836, 3.845 and 2.983, respectively, all P<0.05).Conclusion Lactase deficiency will make children avoid drinking milk or cause symptoms like diarrhea and abdominal pain after drinking milk. Consequently, it will lead to the loss of nutrient substance in diary product and bring adverse effects to children’s physical development.
[Key words]Cangzhou; children; lactase deficiency (LD); physical development

