中性粒细胞/淋巴细胞比值与高血压患者左心室舒张功能不全的关系研究
黄南和,林润杰,孔倩文,谭志发
·论著·
中性粒细胞/淋巴细胞比值与高血压患者左心室舒张功能不全的关系研究
黄南和,林润杰,孔倩文,谭志发
528400广东省中山市小榄人民医院心血管内科(黄南和,林润杰,孔倩文),超声科( 谭志发)
【摘要】目的探究中性粒细胞/淋巴细胞比值(NLR)与高血压患者左心室舒张功能不全的关系。方法选取2013年1月—2015年10月在中山市小榄人民医院心血管内科住院的高血压患者46例,根据是否合并左心室舒张功能不全分为对照组(未合并左心室舒张功能不全,n=30)和观察组(合并左心室舒张功能不全,n=16)。比较两组患者实验室检查指标〔包括低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C)、三酰甘油(TG)、纤维蛋白原(FIB)及C反应蛋白(CRP)〕及超声心动图检查结果〔包括左心室射血分数(LVEF)、左心室舒张末期内径(LVEDd)、左心室收缩末期内径 (LVESd)、室间隔厚度(IVS)、左心室后壁厚度(LVPW)、舒张早期E峰峰速/舒张晚期A峰峰速(E/A)比值、E峰减速时间(EDT)、左房室瓣舒张早期血流峰速度/左房室瓣环舒张早期运动峰速度(E/Ea)〕,比较不同左心室舒张功能不全分级患者NLR、E/A比值、E/Ea及EDT,并分析NLR与E/A比值、E/Ea及EDT的相关性。结果观察组患者HDL-C和TG水平低于对照组(P<0.05);两组患者LDL-C、FIB、CRP水平比较,差异均无统计学意义(P>0.05)。两组患者LVEF、LVEDd及LVESd比较,差异无统计学意义(P>0.05);观察组患者IVS、LVPW、E/Ea及NLR大于对照组,EDT短于对照组,E/A比值小于对照组(P<0.05)。根据左心室舒张功能不全分级标准将观察组患者分为Ⅰ级9例,Ⅱ级4例,Ⅲ级3例。Ⅲ级患者NLR、E/A比值、E/Ea大于Ⅰ级和Ⅱ级患者,EDT短于Ⅰ级和Ⅱ级患者(P<0.05);Ⅱ级患者NLR、E/A比值、E/Ea大于Ⅰ级患者,EDT短于Ⅰ级患者(P<0.05)。Pearson直线相关性分析结果显示,NLR与E/A比值(r=0.395,P<0.05)、E/Ea(r=0.419,P<0.05)呈正相关,与EDT呈负相关(r=-0.17,P<0.05)。结论NLR与高血压患者左心室舒张功能不全严重程度有关,可作为高血压患者左心室舒张功能不全的预测指标。
【关键词】高血压;舒张功能不全;中性粒细胞;淋巴细胞
黄南和,林润杰,孔倩文,等.中性粒细胞/淋巴细胞比值与高血压患者左心室舒张功能不全的关系研究[J].实用心脑肺血管病杂志,2016,24(6):19-22.[www.syxnf.net]
HUANG N H,LIN R J,KONG Q W,et al.Relationship between neutrophils/lymphocyte ratio and left ventricular diastolic dysfunction of patients with hypertension[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2016,24(6):19-22.
高血压对左心室舒张功能的影响早于收缩功能,且左心室舒张功能不全是射血分数正常的心力衰竭(HF-NEF)患者潜在的病理生理改变[1],故评估左心室舒张功能对预测高血压患者早期心功能不全具有重要的临床意义。目前,临床诊断左心室舒张功能不全主要依据超声心动图,但因其缺乏特异性表现而常造成漏诊,故寻找预测左心室舒张功能不全的可靠生化指标是目前的研究热点之一。大量研究表明,中性粒细胞/淋巴细胞比值(neutrophil to lymphocyte ratio,NLR)是外周血管病变、钙化性主动脉瓣狭窄及冠状动脉疾病严重程度、危险分层、预后的预测指标[2-6],其不仅可以预测心血管疾病,还可以预测非心脏疾病(包括肿瘤、血液系统疾病、免疫系统疾病、感染性疾病等),但目前国内关于NLR与高血压患者左心室舒张功能不全相关性的研究报道较少。本研究旨在探讨NLR与高血压患者左心室舒张功能不全的关系,为高血压患者左心室舒张功能不全的诊断提供帮助。
1资料与方法
1.1一般资料选取2013年1月—2015年10月在中山市小榄人民医院心血管内科住院的高血压患者46例,均为新近诊断为高血压或已诊断为高血压但未进行药物治疗者。患者入院后即刻行超声心动图检查,根据是否合并左心室舒张功能不全分为对照组(未合并左心室舒张功能不全,n=30)和观察组(合并左心室舒张功能不全,n=16)。观察组中男10例,女6例;平均年龄(50.2±4.3)岁。对照组中男18例,女12例;平均年龄(49.5±7.3)岁。两组患者性别(χ2=0.027)、年龄(t=0.351)比较,差异无统计学意义(P>0.05),具有可比性。排除标准:(1)正在进行药物治疗的高血压患者;(2)合并脑血管疾病、肿瘤、肝肾功能不全、急慢性感染、血液系统疾病、内分泌系统疾病、免疫系统疾病、慢性阻塞性肺疾病、心房颤动、结缔组织疾病、风湿性心脏瓣膜病、心肌病、先天性心脏病患者;(3)瓣膜移植术后患者。
1.2左心室舒张功能不全诊断标准[7](1)有典型的心力衰竭症状和体征;(2)左心室射血分数(LVEF)正常或轻度下降(≥45%),且左心室不大;(3)有相关结构性心脏病存在的证据(如左心室肥厚、左心房扩大)和/或舒张功能不全;(4)经超声心动图检查证实无心脏瓣膜疾病,并排除心包疾病、肥厚型心肌病、限制型(浸润性)心肌病等。
1.3方法
1.3.1血液标本收集及检测方法所有患者于入院当天静息状态下卧位抽取肘静脉血,采用血细胞分析仪(日本希斯美康Sysmex XE2100+Sp-1000i)检测中性粒细胞、淋巴细胞,并计算NLR;同时检测低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C)、三酰甘油(TG)、纤维蛋白原(FIB)及C反应蛋白(CRP)等。
1.3.2超声心动图检查所有患者入院后由中山市小榄人民医院经验丰富的超声科医师行超声心动图检查,仪器为美国GE公司生产的Vivid E9彩色多普勒超声诊断仪,配备频率为1.7~3.3 MHz的M5S探头、TDI软件及Echopac内置工作站。检测LVEF、左心室舒张末期内径(LVEDd)、左心室收缩末期内径 (LVESd)、室间隔厚度(IVS)、左心室后壁厚度(LVPW)、舒张早期E峰峰速/舒张晚期A峰峰速(E/A)比值、E峰减速时间(EDT)、左房室瓣舒张早期血流峰速度/左房室瓣环舒张早期运动峰速度(E/Ea)。
1.4左心室舒张功能不全分级Ⅰ级(松弛受损型):年龄<55岁者左房室瓣E/A比值<1或EDT>240 ms,年龄>55岁者E/A比值<0.8、EDT>240 ms;E/A比值正常和/或EDT>240 ms者等容舒张时间(IVRT)>90 ms。Ⅱ级(假性正常化):左房室瓣E/A比值为1.0~1.5、EDT>240 ms;出现以下任一情况者:IVRT<90 ms或经Valsalva动作证实E/A比值<1。Ⅲ级(限制性充盈):EDT<60 ms,并出现以下一种以上情况者:左心房内径>50 mm,E/A比值>1.5,IVRT<70 ms。
1.5观察指标比较两组患者实验室检查指标及超声心动图检查结果,比较不同左心室舒张功能不全分级患者NLR、E/A比值、E/Ea及EDT,并分析NLR与E/A比值、E/Ea及EDT的相关性。

2结果
2.1两组患者实验室检查指标比较观察组患者HDL-C和TG水平低于对照组,差异有统计学意义(P<0.05);两组患者LDL-C、FIB、CRP水平比较,差异均无统计学意义(P>0.05,见表1)。

Table1Comparisonoflaboratoryexaminationresultsbetweenthetwogroups
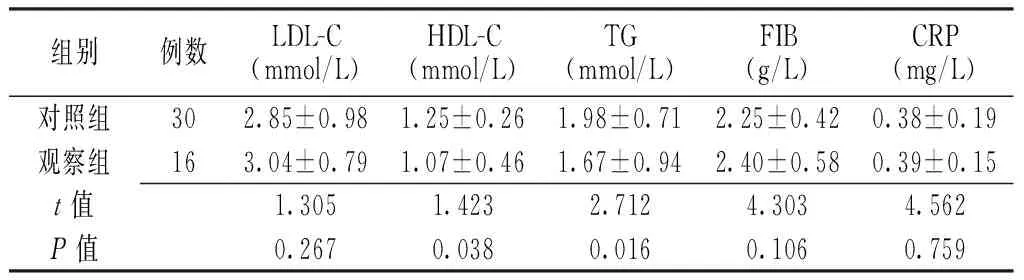
组别例数LDL-C(mmol/L)HDL-C(mmol/L)TG(mmol/L)FIB(g/L)CRP(mg/L)对照组302.85±0.981.25±0.261.98±0.712.25±0.420.38±0.19观察组163.04±0.791.07±0.461.67±0.942.40±0.580.39±0.15t值1.3051.4232.7124.3034.562P值0.2670.0380.0160.1060.759
注:LDL-C=低密度脂蛋白胆固醇,HDL-C=高密度脂蛋白胆固醇,TG=三酰甘油,FIB=纤维蛋白原,CRP=C反应蛋白;1 mm Hg=0.133 kPa
2.2两组患者超声心动图检查结果及NLR比较两组患者LVEF、LVEDd及LVESd比较,差异无统计学意义(P>0.05);观察组患者IVS、LVPW、E/Ea及NLR大于对照组,EDT短于对照组,E/A比值小于对照组,差异有统计学意义(P<0.05,见表2)。
2.3不同左心室舒张功能不全分级患者NLR、E/A比值、E/Ea及EDT比较根据左心室舒张功能不全分级标准将观察组患者分为Ⅰ级9例,Ⅱ级4例,Ⅲ级3例。不同左心室舒张功能不全分级患者间NLR、E/A比值、E/Ea及EDT比较,差异有统计学意义(P<0.05);其中Ⅲ级患者NLR、E/A比值、E/Ea大于Ⅰ级和Ⅱ级患者,EDT短于Ⅰ级和Ⅱ级患者,差异有统计学意义(P<0.05);Ⅱ级患者NLR、E/A比值、E/Ea大于Ⅰ级患者,EDT短于Ⅰ级患者,差异有统计学意义(P<0.05,见表3)。

Table 3Comparison of NLR,E/A ratio,E/Ea and EDT in hypertension patients with different grades of left ventricular diastolic dysfunction
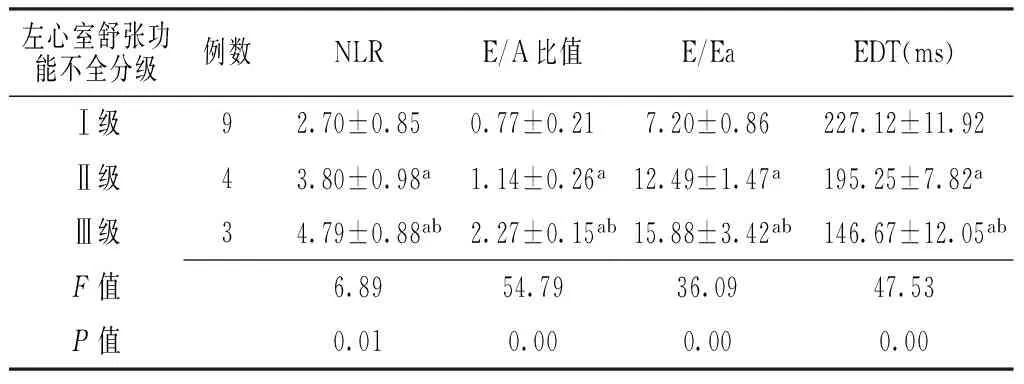
左心室舒张功能不全分级例数NLRE/A比值E/EaEDT(ms)Ⅰ级92.70±0.850.77±0.217.20±0.86227.12±11.92Ⅱ级43.80±0.98a1.14±0.26a12.49±1.47a195.25±7.82aⅢ级34.79±0.88ab2.27±0.15ab15.88±3.42ab146.67±12.05abF值6.8954.7936.0947.53P值0.010.000.000.00
注:与Ⅰ级比较,aP<0.05;与Ⅱ级比较,bP<0.05
2.4相关性分析Pearson直线相关性分析结果显示,NLR与E/A比值(r=0.395,P<0.05)、E/Ea(r=0.419,P<0.05)呈正相关,与EDT呈负相关(r=-0.170,P<0.05)。
3讨论
充血性心力衰竭是心血管疾病患者死亡的主要原因之一,而高血压是心力衰竭的主要病因[8]。高血压可引起左心室向心性肥厚和心室重构,导致左心室松弛和充盈受损,即舒张功能不全,且舒张功能不全常发生在收缩功能不全之前。临床研究显示,左心室舒张功能不全患者初期可无明显的临床症状,而一旦出现心力衰竭症状及体征则可能已发展为舒张期心力衰竭,但采用组织多普勒成像技术测定左心室壁心肌纵向运动时发现,单纯舒张功能不全患者存在左心室壁心肌纵向运动异常,因此临床常根据LVEF将充血性心力衰竭分为收缩期心力衰竭和舒张期心力衰竭,而舒张期心力衰竭又称为HF-NEF或收缩功能保留的心力衰竭(HF-PSF)[9]。

表2 两组患者超声心动图检查结果及NLR比较±s)
注:LVEF=左心室射血分数,LVEDd=左心室舒张末期内径,LVESd=左心室收缩末期内径,IVS=室间隔厚度,LVPW=左心室后壁厚度,E/A=舒张早期E峰峰速/舒张晚期A峰峰速,E/Ea=左房室瓣舒张早期血流峰速度/左房室瓣环舒张早期运动峰速度,EDT=E峰减速时间,NLR=中性粒细胞/淋巴细胞比值
与左心室收缩功能不全相比,左心室舒张功能不全常被临床医生忽略,但其对患者预后却具有重要影响。研究表明,左心室舒张功能不全是心力衰竭和心血管不良事件的重要潜在病理生理基础[10],且其临床诊断相对困难[11],故常出现漏诊。为了提高左心室舒张功能不全已的诊断准确率,积极寻找可靠的生化指标预测左心室舒张功能不全已成为目前的研究热点之一。
NLR是新近发现的能预测心血管疾病的临床标志物,已广泛应用于临床。研究表明,NLR在评估冠心病患者病死率、ST抬高型心肌梗死患者发病率及支架内血栓形成发生风险等方面均具有重要的指导意义[12-14],且NLR异常常被认为是轻度促炎反应所致。促炎反应可引起舒张功能不全和HF-PEF患者早期各种炎性标志物水平升高[15],故NLR异常可能与舒张功能不全有关。临床研究显示,E/A比值、E/Ea及EDT是反映心室舒张功能的常用指标,其中E/A比值与左心室舒张功能不全分级有关;E/Ea与左心室充盈压及肺毛细血管契压高度相关,能反映早期舒张功能减退情况;当心肌松弛性减弱时EDT延长,心肌顺应性减弱时EDT缩短。
本研究结果显示,观察组患者IVS、LVPW、E/Ea及NLR大于对照组,EDT短于对照组,E/A比值小于对照组,提示高血压患者在心室肥厚现象;且随着左心室舒张功能不全分级增加患者NLR、E/A比值、E/Ea逐渐增大,EDT逐渐缩短,提示NLR、E/A比值、E/Ea增大及EDT缩短与高血压患者左心室舒张功能不全有关。本研究进行的相关性分析发现,NLR与E/A值、E/Ea呈正相关,与EDT呈负相关,提示NLR越高,高血压患者左心室舒张功能减退程度越严重。
综上所述,NLR与高血压患者左心室舒张功能不全严重程度有关,且检测NLR简单易行、费用少,可作为高血压患者左心室舒张功能不全的预测指标,可在基层医院推广应用。
作者贡献:黄南和进行实验设计与实施、资料收集整理、撰写论文、成文并对文章负责;林润杰、谭志发进行实验实施、评估、资料收集;孔倩文进行质量控制及审校。
本文无利益冲突。
参考文献
[1]AZIZ F,THAZHATAUVEETIL-KUNHAHAMED L A,ENWELUZO C,et al.Heart failure with preserved EF:abird eye view[J].J Nepal Med Assoc,2013,52(190):405-412.
[3]AÇAR G,FIDAN S,USLU Z A,et al.Relationship of neutrophIL-lymphocyte ratio with the presence,severity,and extent of coronary atherosclerosis detected by coronary computed tomography angiography[J].Angiology,2015,66(2):174-179.
[4]ARBEL Y,FINKELSTEIN A,HALKIN A,et al.Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography[J].Atherosclerosis,2012,225(2): 456-460.
[5]AVCI A,ELNUR A,GÖKSEL A,et al.The relationship between neutrophil/lymphocyte ratio and calcific aortic stenosis[J].Echocardiography,2014,31(9):1031-1035.
[6]SHAH N,PARIKH V,PATEL N,et al.Neutrophil lymphocyte ratio significantly improves the Framingham risk score in prediction of coronary heart disease mortality:insights from the National Health and Nutrition Examination Survey-Ⅲ[J].Int J Cardiol,2014,171(3):390-397.
[7]中华医学会心血管病学分会.中华医学会心血管病杂志编辑委员会.慢性心力衰竭诊断治疗指南[J].中华心血管病杂志,2007,5(12):1076-1095.
[8]PELA G,REGOLISTI G,COBASSI A,et al.Effects of the reduction of preload on left and right ventricular myocardial velocities analyzed by Doppler tissue echocardiography in healthy subjects[J].Eur J Echocardiogr,2004,5(4):262-271.
[9]GIORGI D,BELLO V D,PEDRINELLI R,et al.Ultrasonic tissue characterization and Doppler tissue imaging in the analysis of left ventricular function in essential arterial hypertension:a preliminary study[J].Echocardiography,2002,19(3):187-198.
[10]SHAH A M,CLAGGETT B,SWEITZER N K,et al.Cardiac structure and function and prognosis in heart failure with preserved ejection fraction:findings from the echocardiographic study of the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist (TOPCAT) Trial[J].Circ Heart Fail,2014,7(5):740-751.
[11]BORBELY A,VAN DER VELDEN J,PAPP Z,et al.Cardiomyocyte stiffness in diastolic heart failure[J].Circulation,2005,111(5):774-781.
[12]PARK J J,JANG H J,OH I Y,et al.Prognostic value of neutrophil to lymphocyte ratio in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention[J].Am J Cardiol,2013,111(5):636-642.
[13]AYÇA B,AKIN F,CELIK O,et al.Neutrophil to Lymphocyte ratio is related to stent thrombosis and high mortality in patients with acute myocardial infarction[J].Angiology,2014,66(6):545-552.
[14]Ayca B,Akin F,Celik O,et al.The relationship between the neutrophIL-lymphocyte ratio and the coronary collateral circulation in patients with chronic total occlusion[J].Angiology,2015,29(4): 360-366.
[15]O′MEARA E,DE DENUS S,ROULEAU J L,et al.Circulating biomarkers in patients with heart failure and preserved ejection fraction[J].Curr Heart Fail Rep,2013,10(4):350-358.
(本文编辑:谢武英)
【中图分类号】R 544.1
【文献标识码】A
DOI:10.3969/j.issn.1008-5971.2016.06.005
(收稿日期:2016-02-15;修回日期:2016-05-31)
Relationship Between Neutrophils/Lymphocyte Ratio and Left Ventricular Diastolic Dysfunction of Patients With Hypertensio
HUANGNan-he,LINRun-jie,KONGQian-wen,TANZhi-fa.
DepartmentofCardiology,XiaolanPeople′sHospitalofZhongshan,Zhongshan528400,China
【Abstract】ObjectiveTo investigate the relationship between neutrophils/lymphocyte ratio(NLR)and left ventricular diastolic dysfunction of patients with hypertension.MethodsFrom January 2013 to October 2015 in the Department of Cardiology,Xiaolan People′s Hospital of Zhongshan,a total of 46 patients with hypertension were selected,and they were divided into control group(did not complicated with left ventricular diastolic dysfunction,n=30)and observation group(complicated with left ventricular diastolic dysfunction,n=16).Laboratory examination results(including LDL-C,HDL-C,TG FIB and CRP)and echocardiography examination results(including LVEF,LVEDd,LVESd,IVS,LVPW,E/A ratio,EDT and E/Ea)were compared between the two groups;NLR,E/A ratio,E/Ea,and EDT were compared in hypertension patients with different grades of left ventricular diastolic dysfunction,and correlation between NLR and E/A ratio,and E/Ea and EDT was respectively analyzed.ResultsHDL-C and TG of observation group were statistically significantly lower than those of control group(P<0.05),while no statistically significant differences of LDL-C,FIB or CRP was found between the two groups(P>0.05).No statistically significant differences of LVEF,LVEDd or LVESd was found between the two groups(P>0.05);IVS,LVPW,E/Ea and NLR of observation group were statistically significantly larger than those of control group,EDT of observation group was statistically significantly shorter than that of control group,while E/A ratio of observation group was statistically significantly smaller than that of control group(P<0.05).According to the grades of left ventricular diastolic dysfunction,patients of observation groups were divided into three subgroups:A group(with Ⅰ-grade left ventricular diastolic dysfunction,n=9),B group(with Ⅱ-grade left ventricular diastolic dysfunction,n=4)and C group(with Ⅲ-grade left ventricular diastolic dysfunction,n=3).NLR,E/A ratio and E/Ea of C group were statistically significantly larger than those of A group and B group,while EDT of observation group was statistically significantly shorter than that of A group and B group,respectively(P<0.05);NLR,E/A ratio and E/Ea of B group were statistically significantly larger than those of A group,while EDT of B group was statistically significantly shorter than that of A group(P<0.05).Pearson linear correlation analysis showed that,NLR was positively correlated with E/A ratio(r=0.395,P<0.05),with E/Ea(r=0.419,P<0.05),respectively,was negatively correlated with EDT(r=-0.17,P<0.05).ConclusionNLR is correlated with left ventricular diastolic dysfunction of patients with hypertension,can be used as predictive index of left ventricular diastolic dysfunction of patients with hypertension.
【Key words】Hypertension;Diastolic dysfunction;Neutrophils;Lymphocytes

