不同肝癌分期系统预测混合型肝细胞-胆管细胞癌患者手术预后的比较
李 昊,王曦滔,张爱群,孟翔飞,余 强,吕文平,段伟东,董家鸿
中国人民解放军总医院肝胆外科 全军肝胆外科研究所,北京 100853
·论著·
不同肝癌分期系统预测混合型肝细胞-胆管细胞癌患者手术预后的比较
李昊,王曦滔,张爱群,孟翔飞,余强,吕文平,段伟东,董家鸿
中国人民解放军总医院肝胆外科全军肝胆外科研究所,北京 100853
摘要:目的比较不同原发性肝癌分期系统对混合型肝细胞-胆管细胞癌(cHCC-CC)手术治疗患者的预后预测能力。方法将2005年5月至2013年8月在中国人民解放军总医院行手术治疗、有术后病理确诊结果、临床资料和随访资料完备的54例cHCC-CC纳入研究。利用8种肝癌分期系统对该组病例分期,采用病例构成比、生存曲线、受试者工作特征曲线分别比较各分期系统的病例分层能力、预后区分能力及预后结果预测能力。结果肝内胆管癌肿瘤-淋巴结-转移[TNM(ICC)]分期及日本集成分期评分病例构成相对均衡。本组病例术后12和24个月累计生存率分别为65.5%、56.3%。各期生存曲线差异有统计学意义(P<0.05)的分期有TNM(ICC)分期(Ⅰ期比Ⅱ期,P=0.012;Ⅱ 期比 Ⅲ&Ⅳ期,P=0.002)、奥田邦雄分期(Ⅰ期比Ⅱ期,P=0.025)、法国分期(A期 比 B期,P=0.045)。术后12和24个月各分期系统受试者工作特征曲线下面积由大到小分别为TNM(ICC)分期(0.836、0.847)、巴塞罗那临床肝癌分期(0.744、0.780)、日本集成分期评分(0.723、0.764)、意大利肝癌评分(0.710、0.786),其余分期系统的受试者工作特征曲线下面积差异无统计学意义。结论TNM(ICC)分期对cHCC-CC病例分层能力、预后区分能力及预后结果预测能力均优于其他7种分期系统。
关键词:原发性肝癌;混合型肝细胞-胆管细胞癌;分期系统;预后
ActaAcadMedSin,2016,38(2):175-181
混合型肝细胞-胆管细胞癌(combined hepatocellular-cholangiocellular carcinoma,cHCC-CC)是一种同时具有肝细胞及胆管细胞分化特征的原发性肝癌(primary liver cancer,PLC),临床少见,占原发性肝癌的1.0%~4.7%[1]。由于发病率较低且术前鉴别诊断困难,不同中心对该病的致病机制、临床及预后特征的研究结果不甚一致[2- 5]。目前,手术切除是唯一可以治愈此类肿瘤的治疗措施,但早期接受肿瘤根治性切除的患者预后仍不理想[6]。肿瘤的临床分期可以作为决定治疗方案及预测患者预后的依据,目前被广泛认可的PLC分期系统有:日本奥田邦雄(Okuda)分期系统[7]、日本集成分期(Japan Integrated Staging,JIS)[8]、美国巴塞罗那临床肝癌(Barcelona Clinic Liver Cancer,BCLC)分期系统[9]、意大利肝癌(Cancer of the Liver Italian Program,CLIP)评分系统[10]、法国(French)分期系统[11]、香港中文大学预后系数(Chinese University Prognostic Index,CUPI)评分系统[12]、国际抗癌联盟(Union for International Cancer Control,UICC)—美国癌症联合会(American Joint Committee on Cancer,AJCC)制定的肿瘤-淋巴结-转移(tumor-node-metastasis,TNM)分期系统[13]。以上分期系统大都是以原发性肝细胞癌(hepatocellular carcinoma,HCC)为研究对象制定的。2010年,UICC-AJCC制定的第7版TNM分期将肝内胆管癌(intrahepatic cholangiocarcinoma,ICC)分期从肝癌分期中独立出来,提示ICC与HCC预后的差异,并推荐cHCC-CC纳入肝内胆管癌TNM分期标准中[14]。哪种分期更适用于cHCC-CC患者的诊治和预后判别尚无定论。在对比以上8种分期系统对cHCC-CC患者预后的指导作用,评估不同分期系统对cHCC-CC的临床价值。
对象和方法
对象收集2005年5月至2013年8月中国人民解放军总医院收治的cHCC-CC手术治疗患者资料81例。排除临床资料不全或失访患者27例,剩余54例纳入本研究。cHCC-CC确诊依据术后病理检查结果。并发症分级标准采用Clavien分级[15]。所有患者均签署由中国人民解放军总医院医学伦理委员会批准的知情同意书,符合伦理学规定。
病例随访所有患者通过门诊或电话进行定期随访,术后前6个月,每1~2个月随访1次;以后每3~6个月随访1次。每次随访均收集临床、实验室及影像学资料等。随访终止于2015年8月。
统计学处理本研究生存率是评估不同分期系统效能的唯一指标。生存期被定义为cHCC-CC首次确诊到死亡或最后一次随访之间的时间间隔。采用SPSS 22.0软件进行数据分析,Kaplan-Meier法绘制生存曲线,并行 Log-rank检验。比较各分期系统生存率预测能力采用受试者工作特征(receiver operating characteristic,ROC)曲线法[16]。检验水准α=0.05。P<0.05为差异有统计学意义。
结果
患者特征54例患者中男性43例(79.6%)、女性11例(20.4%),年龄中位数为51岁(28~78岁);乙肝表面抗原阳性34例(63%),未见丙肝抗体阳性患者,肝硬化45例(83.3%);无症状25例(46.3%),有症状29例(53.7%),其中腹痛21例(38.9%),纳差、体质量减轻4例,恶心2例,发热2例,黄疸2例,呕血1例;Child-Pugh分期:A期49例(90.7%),B期5例(9.3%),未见C期;术前诊断:肝占位5例(9.3%),原发性肝癌34例(63%),肝内胆管癌7例(13%),肝细胞癌6例(11.1%),肝脏局灶性结节增生、肝门胆管癌各1例(1.9%);肿瘤标志物异常:甲胎蛋白≥20 ng/ml 28例(51.9%),癌胚抗原≥5 ng/ml 7例(13%),糖链抗原19- 9≥37 U/ml 31例(57.4%);手术方式:局部不规则肝切除25例(46.3%),解剖性肝段(叶)切除27例(50%),同种异体原位肝移植(背驮式)2例(3.7%),5例(9.3%)患者联合行淋巴结切除术;术后并发症分级:Ⅰ级31例(57.4%),Ⅱ级19例(35.2%),Ⅲ-a级4例(7.4%)。
肿瘤特征54例患者肿瘤特征主要依据术后常规病理结果及术中探查,辅以术前影像学检查。单发肿瘤34例(63%),多发肿瘤结节不超过3个12例(22.2%),超过3个8例(14.8%);肿瘤大小以最大肿瘤直径为标准,<2 cm 4例(7.4%),2~5 cm 23例(42.6%),>5 cm 27例(50%);门静脉癌栓形成10例(18.5%);邻近器官浸润7例(13%),其中侵犯膈肌2例,侵犯胃小弯、结肠肝曲、胆囊、胆总管、大网膜各1例,区域淋巴结定义为肝门、肝十二指肠韧带、膈下及腔静脉旁淋巴结,术后病理证实区域淋巴结转移4例(7.4%);肿瘤远处转移3例(5.6%),包含2例腹膜后转移及1例骨转移;术后病理:肝细胞癌成分为主11例(20.4%),胆管细胞癌成分为主12例(22.2%),两者相当4例(7.4%),其余不详。
各分期患者构成比按照8种分期系统进行分类,病例构成比为Okuda分期Ⅰ、Ⅱ期各为0.67、0.33,Ⅲ期未见;CLIP分期0、1、2分及3分以上各为0.37、0.33、0.15、0.15;French分期A、B期各为0.37、0.63,C期未见;BCLC分期0-A、B、C期各为0.46、0.19、0.35,D期未见;TNM(HCC)分期Ⅰ、Ⅱ、Ⅲ、IV期各为0.35、0.17、0.37、0.11;TNM(ICC)分期Ⅰ、Ⅱ期及Ⅲ期以上各为0.41、0.39、0.20;CUPI分期低危组、中危组各为0.87、0.13,高危组未见;JIS评分0和1分、2分、3分以上各为0.44、0.31、0.24(图1)。
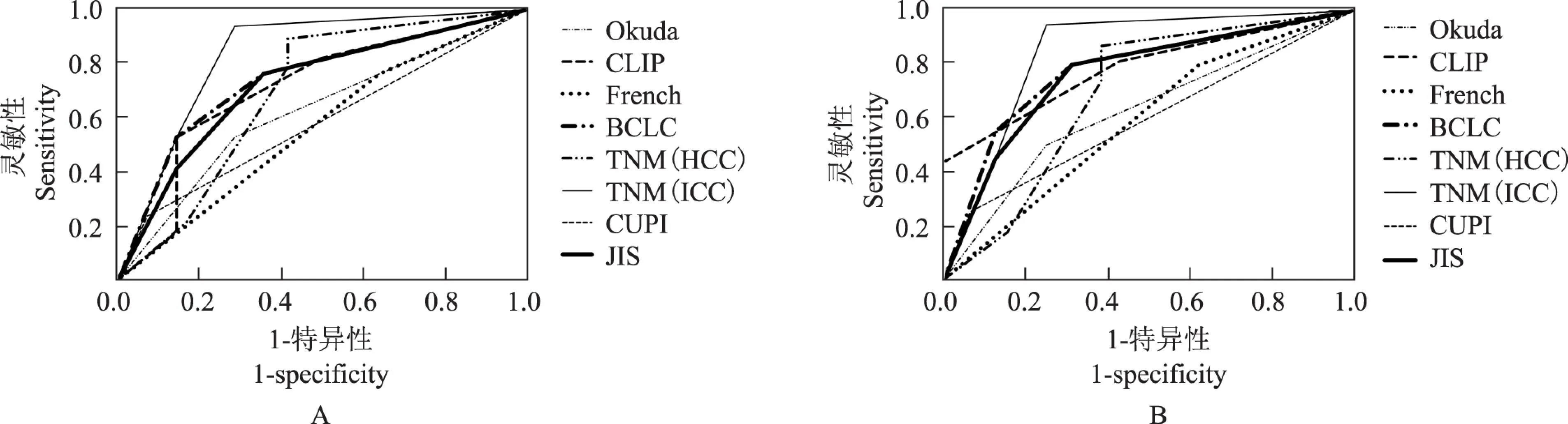
Kaplan-Meier生存曲线8种分期系统Kaplan-Meier生存曲线显示,术后12及24个月的累积生存率分别为65.5%、56.3%。经Log-rank检验可知TNM(ICC)分期、Okuda分期、French分期中各生存曲线差异均有统计学意义(P<0.05)。其中TNM(ICC)分期差异最显著,将该组54例患者显著分为3期,Okuda分期与French分期系统将该组病例分为2期。其余分期除CLIP评分中1分和2分生存曲线之间的差异有统计学意义外,其余差异均无统计学意义(图2)。
不同分期系统对cHCC-CC术后患者预后预测价值的比较术后12及24个月的生存率ROC曲线和曲线下面积(area under curve,AUC)评价各分期对术后患者预后的预测能力显示:CLIP评分、BCLC分期、TNM(ICC)分期、JIS评分术后12和24个月的AUC比较差异均有统计学意义(P<0.05),其中TNM(ICC)分期术后12和24个月AUC最大,分别为0.836、0.847,之后由大到小依次为BCLC分期(0.744、0.780)、JIS评分(0.723、0.764)和CLIP评分(0.710、0.786)。Okuda分期、French分期、TNM(HCC)分期、CUPI分期术后12和24个月的AUC比较差异均无统计学意义(P>0.05)(图3、表1)。
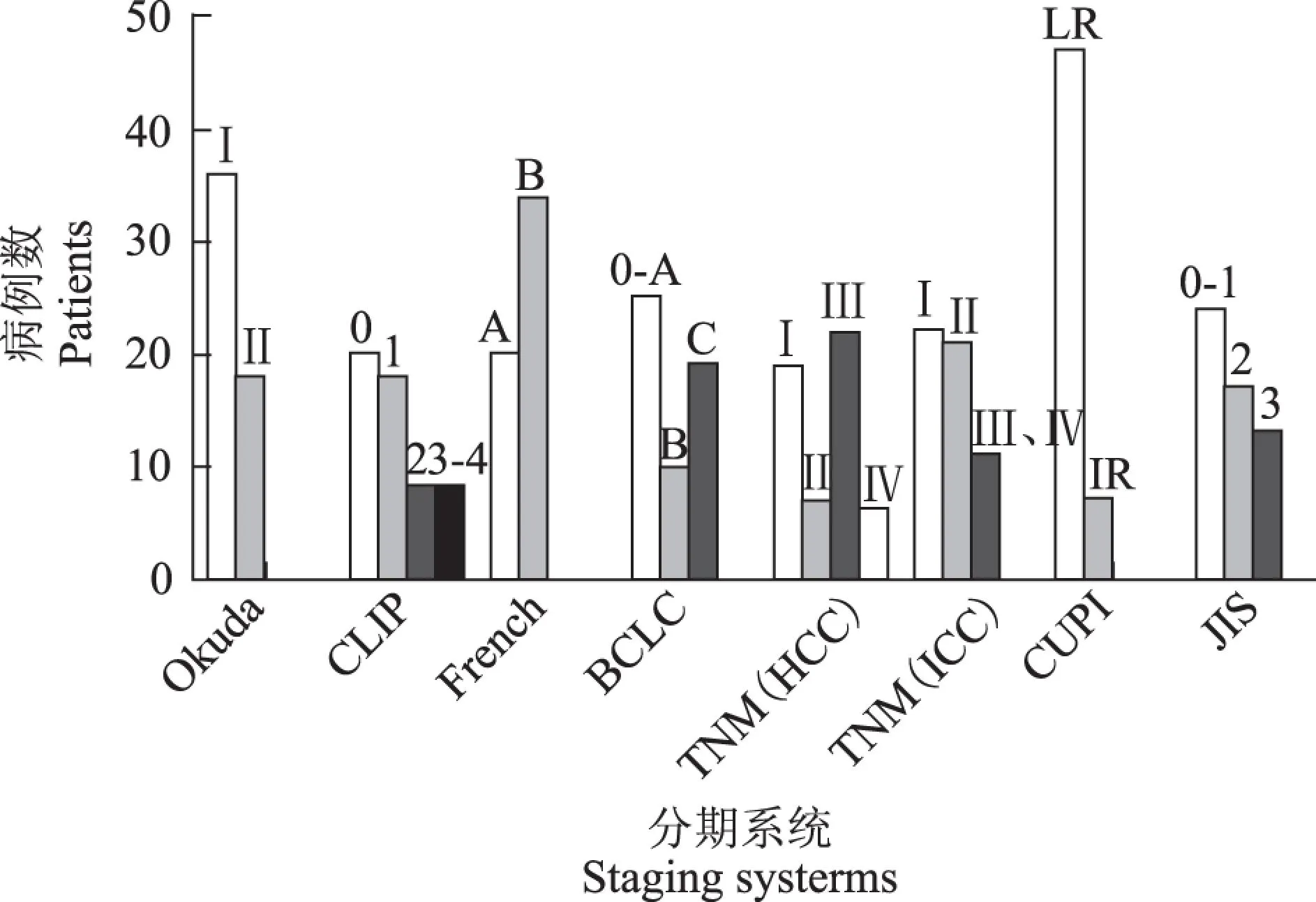
Okuda:奥由邦雄分期;CLIP:意大利肝癌评分系统;French:法国分期;BCLC:巴塞罗那临床肝癌分期;TNM(HCC):美国癌症联合会肿瘤-淋巴结-转移分期肝细胞癌分期;TNM(ICC):美国癌症联合会第7版肿瘤-淋巴结-转移分期肝内胆管癌分期;CUPI:香港中文大学预后系数评分;JIS:日本集成分期;LR:低危;IR:中危
Okuda:Okuda staging system;CLIP:Cancer of the Liver Italian Program scoring system;French:French staging system; BCLC:Barcelona Clinic Liver Cancer staging system;TNM(HCC):American Joint Committee on Cancer of tumor-node-metastasis staging for hepatocellular carcinoma;TNM(ICC):American Joint Committee on Cancer 7th edition of tumor-node-metastasis staging for intrahepatic cholangiocarcinoma;CUPI:Chinese University Prognostic Index;JIS:Japan Integrated Staging;LR:low risk;IR:intermediate risk
图 18种分期系统的病例分布
Fig 1Patients data categorized using eight staging systems
OS:总体生存率
OS:overall survival rate
图 28种分期系统的Kaplan-Meier生存曲线图
Fig 2Kaplan-Meier survival curves of eight staging systems
cHCC-CC:混合型肝细胞-胆管细胞癌;ROC:受试者工作特征
cHCC-CC:combined hepatocellular-cholangiocellular carcinoma;ROC:receiver operating characteristic
图 38种分期系统预测cHCC-CC手术治疗后12(A)和24个月(B)生存率的ROC曲线图
Fig 3ROC curves of eight staging systems on predicting 12(A)and 24 months(B)of survival rates after surgical treatment for cHCC-CC patients
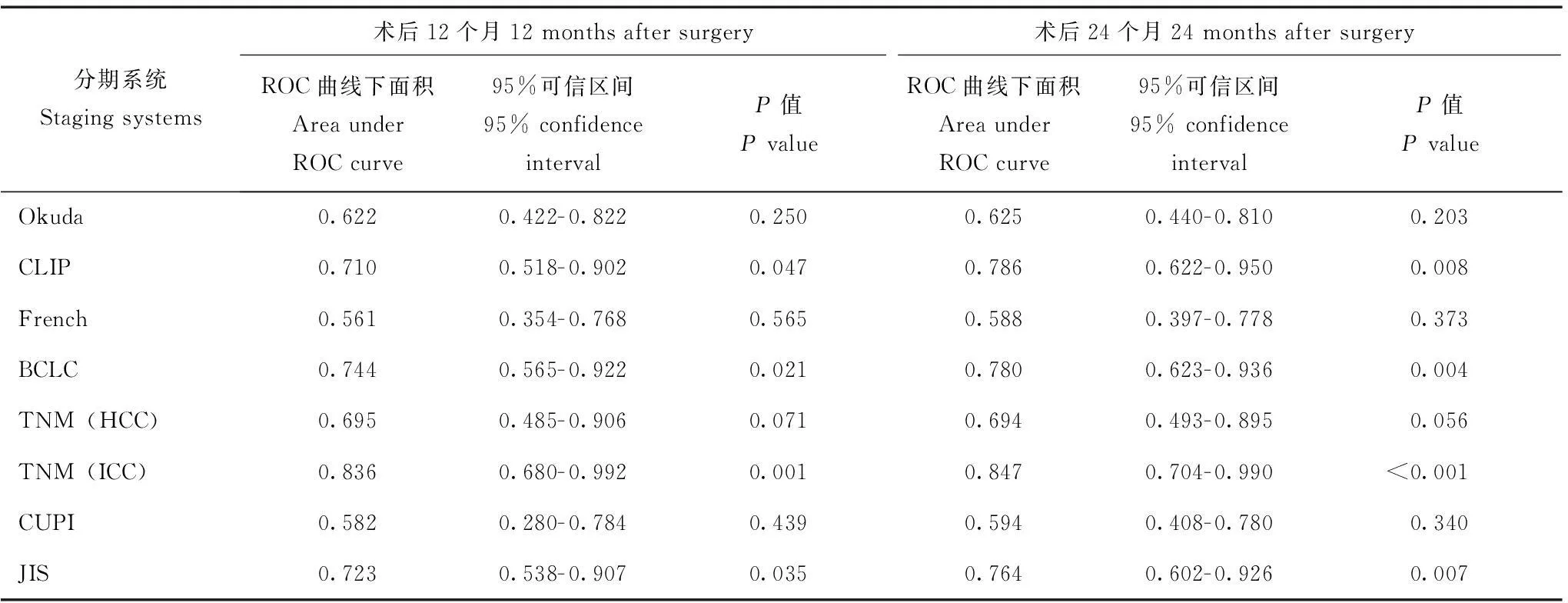
表 1 8种分期系统预测cHCC-CC术后12和24个月生存率ROC曲线下面积比较
讨论
cHCC-CC是除HCC和ICC之外的一种罕见的原发性肝癌,由于临床相对少见,目前对此类肿瘤尚缺乏深刻认识。WHO分类将其定义为肿瘤含有明确的HCC和CC成分,并区别于单独的HCC和ICC在同一肝脏产生的情况[17]。目前该病发病机制仍不明确,可能与肝脏中有肝细胞和胆管细胞双向潜能的肝前体细胞或肿瘤干细胞有关[18- 19]。此类肿瘤恶性程度高,有报道称其预后介于HCC和ICC之间[4],但也有研究指出可能较HCC和ICC都差[20]。不同文献报道手术预后危险因素略有差异,主要有乙肝背景、低分化、癌结节≥2个、最大肿瘤直径>5 cm、大血管侵犯、肝被膜侵犯、淋巴结转移、术前低蛋白血症、安全切缘<2 cm、糖链抗原19- 9升高、肿瘤内胆管细胞癌成分为主等[17,21]。
流行病学上,cHCC-CC的高危因素与HCC相似,如本研究病例多数合并乙肝病毒感染、肝硬化及甲胎蛋白升高,与国内外报道[5- 6,21]一致。不典型的临床症状、影像学表现使cHCC-CC诊断极为困难。本研究多数患者因体检发现或近期腹痛前来就诊,经术前检查大多患者可诊断为肝脏恶性肿瘤。尽管部分患者甲胎蛋白水平异常伴有癌胚抗原或糖链抗原19- 9升高,提示可能含有两种肿瘤成分,但其术前诊断无法对肿瘤进一步分型。cHCC-CC患者的确诊往往依赖于术后的常规病理结果。由于术前诊断困难,此类患者在术后病理结果确诊之前常按照HCC的治疗原则处理,本研究仅5例术前或术中怀疑为cHCC-CC或肝门周围淋巴结肿大的cHCC-CC联合进行了淋巴结切除术。术前诊断会影响手术方式的选择,进而可能影响患者的预后结果。
分期系统对指导肿瘤患者的治疗及判断患者的预后有重要意义,而目前哪种分期适合HCC-CC尚无定论。利用8种分期系统对本研究54例HCC-CC患者资料进行分类,根据各分期的病例分布情况,可间接推测出各分期的病例分层能力[22]。本研究对象为经手术治疗的cHCC-CC患者,除2例患者因肝硬化失代偿期行肝移植手术外,其他均属较早期患者,因而在各分期上晚期病例数稀少。TNM(ICC)分期及JIS评分各期病例构成相对均衡,提示两者分层能力较其他分期好。本组54例患者术后12及24个月的累积生存率分别为65.5%、56.3%,Kaplan-Meier生存曲线显示TNM(ICC)分期的各生存曲线之间的差异较其他分期系统的差异更显著,提示TNM(ICC)分期对术后cHCC-CC患者区分能力较其他分期系统强。在ROC曲线中,TNM(ICC)分期曲线下面积最大,提示其预后判别能力最佳,其后依次为BCLC分期、JIS评分、CLIP评分,其他分期因AUC差异无统计学意义而对预后的预测价值不大。
日本Okuda分期[7]、JIS评分[8],意大利CLIP评分[10],法国French分期[11]及香港CUPI评分[12]制定时的研究对象即为晚期病例居多,主要用于预测晚期不可手术肝癌患者的短期生存率。这可能影响到这些分期系统在本研究(早中期病例为主)中的表现。而美国TNM分期[13]、BCLC分期[23]对较早期包括经手术治疗的肝癌患者的预后预测能力相对较好。Kim等[24]的研究显示胆管细胞癌成分是决定cHCC-CC患者预后的主要因素,一项法国的研究也显示cHCC-CC的分子致病通路更接近于ICC[2],这与本研究TNM(ICC)分期系统表现一致。
对于有慢性肝炎病毒感染、肝硬化背景的PLC而言,一个好的预后分期系统应兼顾肿瘤本身相关因素和肝脏功能储备。虽然本研究TNM(ICC)分期在cHCC-CC病例分层能力、术后的预后区分能力及预后预测能力方面均优于其他7种分期系统,但并未顾及到肝功能储备方面的因素,因此可能会将不同病理状态的患者归于同一期。目前各种PLC的临床分期系统都有其不足之处,缺乏普适性,对于cHCC-CC这种特殊病理亚型可能存在更多问题。制定一种更加合理的cHCC-CC临床分期系统亟需更多大样本的多中心临床研究支持,同时术前检测外周血循环肿瘤细胞或血浆核酸水平可能对HCC-CC术前精准分子分型具有重要参考价值。
参考文献
[1]Yeh MM. Pathology of combined hepatocellular-cholangiocarcinoma [J]. J Gastroenterol Hepatol,2010,25(9):1485.
[2]Cazals-Hatem D,Rebouissou S,Bioulac-Sage P,et al. Clinical and molecular analysis of combined hepatocellular-cholangiocarcinomas [J]. J Hepatol,2004,41(2):292- 298.
[3]Koh KC,Lee H,Choi MS,et al. Clinicopathologic features and prognosis of combined hepatocellular cholangiocarcinoma[J]. Am J Surg,2005,189(1):120- 125.
[4]Tang D,Nagano H,Nakamura M,et al. Clinical and pathological features of Allen’s type C classification of resected combined hepatocellular and cholangiocarcinoma:a comparative study with hepatocellular carcinoma and cholangiocellular carcinoma[J]. J Gastrointest Surg,2006,10(7):987- 998.
[5]Portolani N,Baiocchi GL,Coniglio A,et al. Intrahepatic cholangiocarcinoma and combined hepatocellular-cholangiocarcinoma:a Western experience[J]. Ann Surg Oncol,2008,15(7):1880- 1890.
[6]Park SE,Lee SH,Yang JD,et al. Clinicopathological characteristics and prognostic factors in combined hepatocellular carcinoma and cholangiocarcinoma[J]. Korean J Hepatobiliary Pancreat Surg,2013,17(4):152- 156.
[7]Okuda K,Ohtsuki T,Obata H,et al. Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Study of 850 patients[J]. Cancer,1985,56(4):918- 928.
[8]Kudo M,Chung H,Osaki Y. Prognostic staging system for hepatocellular carcinoma (CLIP score):its value and limitations,and a proposal for a new staging system,the Japan Integrated Staging Score (JIS score)[J]. J Gastroenterol,2003,38(3):207- 215.
[9]Marrero JA,Fontana RJ,Barrat A,et al. Prognosis of hepa-tocellular carcinoma:comparison of 7 staging systems in an American cohort[J]. Hepatology,2005,41(4):707- 716.
[10]Llovet JM,Bruix J. Prospective validation of the Cancer of the Liver Italian Program (CLIP) score:a new prognostic system for patients with cirrhosis and hepatocellular carcinoma[J]. Hepatology,2000,32(3):679- 680.
[11]Chevret S,Trinchet JC,Mathieu D,et al. A new prognostic classification for predicting survival in patients with hepato- cellular carcinoma. Groupe d’Etude et de Traitement du Carcinome Hepatocellulaire[J]. J Hepatol,1999,31(1):133- 141.
[12]Leung TW,Tang AM,Zee B,et al. Construction of the Chinese University Prognostic Index for hepatocellular carcinoma and comparison with the TNM staging system,the Okuda staging system,and the Cancer of the Liver Italian Program staging system:a study based on 926 patients[J]. Cancer,2002,94(6):1760- 1769.
[13]Edge SB,Compton CC. The American Joint Committee on Cancer:the 7th edition of the AJCC cancer staging manual and the future of TNM[J]. Ann Surg Oncol,2010,17(6):1471- 1474.
[14]Farges O,Fuks D,Le TYP,et al. AJCC 7th edition of TNM staging accurately discriminates outcomes of patients with resectable intrahepatic cholangiocarcinoma:by the AFC-IHCC- 2009 study group[J]. Cancer,2011,117(10):2170- 2177.
[15]Clavien PA,Barkun J,de Oliveira ML,et al. The Clavien-Dindo classification of surgical complications:five-year experience[J]. Ann Surg,2009,250(2):187- 196.
[16]Hanley JA,McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases[J]. Radiology,1983,148(3):839- 843.
[17]Chu KJ,Lu CD,Dong H,et al. Hepatitis B virus-related combined hepatocellular-cholangiocarcinoma:clinicopathological and prognostic analysis of 390 cases[J]. Eur J Gastroenterol Hepatol,2014,26(2):192- 199.
[18]Ikeda H,Harada K,Sato Y,et al. Clinicopathologic signifi-cance of combined hepatocellular-cholangiocarcinoma with stem cell subtype components with reference to the expression of putative stem cell markers[J]. Am J Clin Pathol,2013,140(3):329- 340.
[19]罗贤武,袁磊,王义,等. 混合型肝癌和胆管癌的临床病理特点及预后分析[J]. 中国临床医学,2013,20(3):839- 843.
[20]O’Connor K,Walsh JC,Schaeffer DF. Combined hepatocellular-cholangiocarcinoma (cHCC-CC):a distinct entity[J]. Ann Hepatol,2014,13(3):317- 322.
[21]黄振,张业繁,阎涛,等. 肝细胞-胆管细胞混合型肝癌患者临床特点及预后分析[J]. 中华肿瘤防治杂志,2013,20(11):866- 870.
[22]吕文平,董家鸿,李智华,等. 肝细胞癌手术后应用不同分期评估预后的临床研究[J]. 中华普通外科杂志,2007,22(7):514- 517.
[23]Llovet JM,Bru C,Bruix J. Prognosis of hepatocellular carcinoma:the BCLC staging classification[J]. Semin Liver Dis,1999,19(3):329- 338.
[24]Kim KH,Lee SG,Park EH,et al. Surgical treatments and prognoses of patients with combined hepatocellular carcinoma and cholangiocarcinoma[J]. Ann Surg Oncol,2009,16(3):623- 629.
Comparison of the Predictive Values of Eight Staging Systems for Primary Liver Cancer in Prognosis of Combined Hepatocellular-cholangiocellular Carcinoma Patients after Surgery
LI Hao,WANG Xi-tao,ZHANG Ai-qun,MENG Xiang-fei,YU Qiang,LÜ Wen-ping,DUAN Wei-dong,DONG Jia-hong
Department of Hepatobiliary Surgery & Hepatobiliary Surgical Institute,Chinese PLA General Hospital,Beijing 100853,China
ABSTRACT:ObjectiveTo compare the predictive values of eight staging systems for primary liver cancer in the prognosis of combined hepatocellular-cholangiocellular carcinoma(cHCC-CC) patients after surgery. MethodsThe clinical data of 54 cHCC-CC patients who underwent hepatectomy or liver transplantation from May 2005 to Augest 2013 in Chinese PLA General Hospital were collected. We evaluated the prognostic value of the Okuda staging system,Cancer of the Liver Italian Program (CLIP) score,French staging system,Barcelona Clinic Liver Cancer (BCLC) staging system,7th edition of tumour-node-metastasis (TNM) staging system for hepatocellular carcinoma and intrahepatic cholangiocarcinoma (ICC),Japan Integrated Staging (JIS) score,and Chinese University Prognostic Index. The distribution,Kaplan-Meier method,Log-rank test,and area under a receiver operating characteristic curve were used to compare the prognosis-predicting ability of these different staging systems in 54 cHCC-CC patients after surgery. ResultsThe TNM staging system for ICC and JIS score had a better distribution of cases. The 12-and 24-month survivals of the entire cohort were 65.5% and 56.3%,respectively. A Log-rank test showed that there was a significant difference existing in the cumulative survival rates of different stage patients when using TNM staging system for ICC(stage Ⅰ vs. stage Ⅱ,P=0.012;stage Ⅱ vs. stage Ⅲ-Ⅳ,P=0.002),Okuda staging system(stage Ⅰ vs. stage Ⅱ,P=0.025),and French staging system(stage A and stage B,P=0.045). The 12-and 24-month area under curve of TNM staging system for ICC,BCLC staging system,JIS score,and CLIP score were 0.836 and 0.847,0.744 and 0.780,0.723 and 0.764,and 0.710 and 0.786,respectively. ConclusionThe 7th edition of TNM staging system for ICC has superior prognostic value to other seven staging systems in cHCC-CC patients undergoing surgical treatment.
Key words:primary liver cancer;combined hepatocellular-cholangiocellular carcinoma;staging system;prognosis
(收稿日期:2015- 10- 20)
Corresponding author:DONG Jia-hongTel:010- 56118888,E-mail:dongjh301@163.com
DOI:10.3881/j.issn.1000- 503X.2016.02.009
中图分类号:R657.3
文献标志码:A
文章编号:1000- 503X(2016)02- 0175- 07
通信作者:董家鸿电话:010- 56118888,电子邮件:dongjh301@163.com
基金项目:国家科技部支撑计划项目(2012BAI06B01)和国家传染病科技重大专项(2012ZX10002- 017) Supported by the National Key Technology R&D Program of China(2012BAI06B01)and National S&T Major Project for Infectious Diseases of China(2012ZX10002- 017)

