VEGF基因多态性及吸烟在诱发非酒精性脂肪肝中的交互作用
王倩,吴鹏波,李明,罗和生,余媛洁,谭诗云,舒泳翔(武汉大学人民医院,武汉430060)
VEGF基因多态性及吸烟在诱发非酒精性脂肪肝中的交互作用
王倩,吴鹏波,李明,罗和生,余媛洁,谭诗云,舒泳翔(武汉大学人民医院,武汉430060)
摘要:目的观察非酒精性脂肪肝(NAFLD)患者血管内皮生长因子(VEGF)基因rs833061、rs3025039位点多态性,并探讨其多态性及吸烟在诱发NAFLD中的交互作用。方法选择NAFLD患者341例(NAFLD组)、健康体检者246例(对照组),采用PCR-RFLP法分析VEGF基因rs833061、rs3025039位点基因型,非条件Logistic回归分析法分析各基因型与NAFLD易感性的关系,非条件Logistic回归分析法和广义多因子降维法分析VEGF基因多态性及吸烟在诱发NAFLD中的交互作用。结果VEGF基因rs833061位点C基因携带者(CC+CT)罹患NAFLD的风险较非C基因携带者(TT)升高(P均<0.01),rs3025039位点T基因携带者(TT+CT)患病风险较非T基因携带者(CC)风险升高(P均<0.01)。VEGF基因rs833061位点多态性与吸烟可能在 NAFLD发病过程中存在相加作用(P<0.01),rs833061位点CC/CT基因型吸烟个体罹患NAFLD风险是携带TT基因型非吸烟个体的4.93倍。结论VEGF基因多态性与NAFLD发病有关,VEGF基因rs833061位点多态性与吸烟在诱发NAFLD过程中具有协同效应。
关键词:非酒精性脂肪肝;血管内皮生长因子;基因多态性;易感性;交互作用
非酒精性脂肪肝(NAFLD)不仅可进展为肝硬化甚至肝癌,同时还可增加高血压、糖尿病等的罹患风险[1,2]。现已明确,遗传因素在NAFLD发病过程中具有重要作用[3]。血管内皮生长因子(VEGF)可促进血管内皮细胞增殖、分化,增加血管通透性。此外,VEGF还具有调节能量代谢、胰岛素抵抗以及炎症反应等生物学效应[4,5]。研究发现,吸烟不仅加剧胰岛素抵抗,还可导致向心性肥胖[6]。而胰岛素抵抗及向心性肥胖是NAFLD发病的重要危险因素。本研究探讨NAFLD患者VEGF基因rs833061、rs3025039位点多态性及吸烟在诱发NAFLD中的交互作用。
1资料与方法
1.1临床资料选择2012年2月~2014年8月本院收治的NAFLD患者341例(NAFLD组),诊断标准符合《非酒精性脂肪性肝病诊疗指南(2010年修订版)》[7]。其中,男210例、女131例,年龄(46.69±9.87)岁。同期另选在该院体检健康者246例(对照组),男170例、女76例,年龄(47.65±11.36)岁。两组基本资料比较见表1。

表1 两组基本资料比较
注:HOMA-IR为胰岛素抵抗指数;与对照组比较,*P<0.05,△P<0.01。
1.2VEGF基因rs833061、rs3025039位点多态性检测采用PCR-RFLP法。所有研究对象抽取空腹静脉血,采用酚-氯仿法提取基因组DNA。根据VEGF-9及VEGF-2基因的核苷酸序列设计引物,采用PCR扩增目的基因片段。VEGF基因rs833061位点引物序列:上游引物:5′-CTCTTTAGCCAGAGCCGGGG-3′,下游引物:5′-TGGCCTTCTCCCCGCTCCGAC-3′;VEGF基因rs3025039位点引物序列:上游引物5′-AGGGTTCGGGAACCAGATC-3′,下游引物5′-CTCGGTGATTTAGCAGCAAG-3′。PCR反应体系25 μL,包括DNA 100 ng、1.0 U Taq酶、2 μL上下游引物、2×PCR buffer;PCR反应条件:94 ℃ 5 min,94 ℃ 30 s、60 ℃ 30 s、72 ℃ 45 s,30个循环,最后72 ℃延伸10 min。限制性内切酶BsaHⅠ、NlaⅢ酶切。酶切产物经3%琼脂糖凝胶电泳,EB染色成像,判定酶切基因型。

2结果
2.1VEGF基因rs833061、rs3025039位点基因型VEGF基因rs833061位点TT基因型片段长度为230、75 bp(75 bp片段太小,跑出胶外),CT基因型片段长度为290、230 bp,CC基因型片段长度为290 bp。VEGF基因rs3025039位点TT基因型片段长度为195 bp(25 bp片段太小,跑出胶外),CC基因型片段长度为195、170 bp,CT基因型片段长度为170 bp。
2.2两组VEGF基因rs833061、rs3025039位点基因型分布及其与NAFLD易感性的关系两组VEGF基因rs833061、rs3025039位点基因型分布见表2。相关分析显示,VEGF基因rs833061位点C基因携带者(CC+CT)罹患NAFLD的风险是非C基因携带者(TT)的1.56倍(95%CI为1.12~2.15,P<0.05);校正吸烟、腰围、血糖等因素后,C基因携带者(CC+CT)是非C基因携带者(TT)的1.71倍(95%CI为1.42~2.22,P<0.01)。VEGF基因rs3025039位点T基因携带者(TT+CT)罹患NAFLD的风险是非T基因携带者(CC)的1.61倍(95%CI为1.15~2.26,P<0.05);校正吸烟、腰围、血糖等因素后,T基因携带者(TT+CT)罹患NAFLD的风险是非T基因携带者(CC)的1.83倍(95%CI为1.35~2.71,P<0.01)。
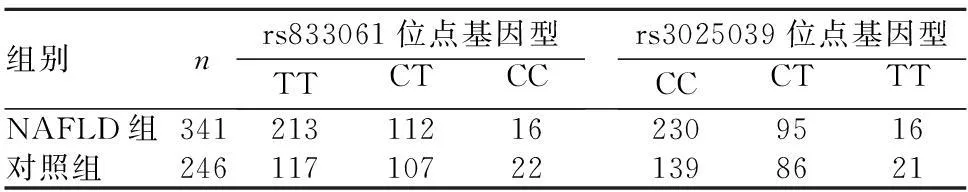
表2 两组VEGF基因rs833061、rs3025039
2.3VEGF基因rs833061、rs3025039位点多态性与吸烟对诱发NAFLD的交互作用VEGF基因rs833061位点多态性+吸烟模型具有最大的预测正确率(0.668 8)和最高的交叉验证一致性(10/10),为最优模型。说明二者存在交互作用。与携带VEGF基因rs833061位点TT基因型不吸烟者相比,携带VEGF基因rs833061位点CT/CC基因型不吸烟者罹患NAFLD的风险增加2.22倍(P<0.01),携带VEGF基因rs833061位点TT基因型吸烟者罹患NAFLD风险增加1.82倍(P<0.01),携带VEGF基因rs833061位点CT/CC基因型吸烟者罹患NAFLD风险增加4.93倍(P<0.01) ;VEGF基因rs833061位点多态性与吸烟对诱发NAFLD存在相加作用(P<0.01)。
3讨论
近年研究证实,遗传因素在NAFLD发病中发挥重要作用[3]。人类VEGF基因位于染色体6p21.3,其蛋白表达水平在不同个体间有一定差异,这可能与VEGF基因多态性有关[9]。VEGF基因多态性位点主要位于5′非翻译区和3′非翻译区。研究发现,VEGF基因多态性与肥胖、多囊卵巢综合症易感性相关[10,11],而肥胖及多囊卵巢综合症与脂肪肝在易感基因方面存在一定相似性[12,13]。因此,VEGF基因多态性可能与NAFLD发病有关。
本文通过病例对照分析发现,以TT为参照,VEGF基因rs833061位点携带CT、CC基因型个体罹患NAFLD的风险增加;以CC为参照,VEGF基因rs3025039位点携带CT、TT基因型个体罹患NAFLD的风险增加。Logistic回归校正腰围、血糖、HDL-C、HOMA-IR及吸烟等因素后,仍发现rs833061、rs3025039位点多态性对NAFLD易感性有显著影响。
NAFLD发病是个体遗传因素与外界环境因素共同作用的结果。吸烟是NAFLD发生的危险因素,吸烟个体罹患NAFLD的风险增加25%[11]。本研究采用GMDR法分析VEGF基因rs833061、rs3025039位点多态性与吸烟对诱发NAFLD的交互作用。GMDR法是研究基因-基因以及基因-环境交互作用的一种可靠方法[12]。结果提示,rs833061位点多态性和吸烟在NAFLD发病中存在交互作用,而rs3025039位点多态性与吸烟则无交互作用。进一步采用非条件Logistic回归分析法及Bootstrap法[14]对上述结果加以验证,结果提示rs833061位点多态性和吸烟存在相加作用,但二者相加作用的机制目前尚不清楚。Fesinmeyer等[15]研究认为,吸烟可能是通过改变rs833061位点多态性协同增加NAFLD易感性。
综上所述, VEGF基因rs833061、rs3025039位点多态性与NAFLD发病有关,VEGF基因rs833061位点多态性与吸烟在诱发NAFLD过程中具有相加作用,但上述结果仍需扩大样本量进一步证实。
参考文献:
[1] Yoon HJ, Cha BS. Pathogenesis and therapeutic approaches for non-alcoholic fatty liver disease[J]. World J Hepatol, 2014,6(11):800-811.
[2] 周歆,侯冬青,段佳丽,等.北京市387名肥胖中学生非酒精性脂肪肝等代谢异常罹患状况调查[J].中华流行病学杂志,2013,34(5):446-450.
[3] Li L, Wang SJ, Shi K, et al. Correlation between MTP -493G>T polymorphism and non-alcoholic fatty liver disease risk: a meta-analysis[J]. Genet Mol Res, 2014,13(4):10150-10161.
[4] Elias I, Franckhauser S, Bosch F. New insights into adipose tissue VEGF-A actions in the control of smoking and insulin resistance[J]. Adipocyte, 2013,12(2):109-112.
[5] Amarapurkar AD, Amarapurkar DN, Vibhav S, et al. Angiogenesis in chronic liver disease[J]. Ann Hepatol, 2007,6(3):170-173.
[6] Chiolero A, Faeh D, Paccaud F, et al. Consequences of smoking for body weight, body fat distribution, and insulin resistance[J]. Am J Clin Nutr, 2008,87(4):801-809.
[7] 中华医学会肝脏病学分会脂肪肝和酒精性肝病学组.非酒精性脂肪性肝病诊疗指南(2010年1月修订版)[J].中华内科杂志,2010,49(3):275-278.
[8] 陈卿,唐迅,胡永华,等.应用广义多因子降维法分析数量性状的交互作用[J].中华流行病学杂志,2010,31(8):938-941.
[9] Rahoui J, Sbitti Y, Touil N, et al. The single nucleotide polymorphism +936 C/T VEGF is associated with human epidermal growth factor receptor 2 expression in Moroccan breast cancer women[J]. Med Oncol, 2014,31(12):336.
[10] Belo VA, Souza-Costa DC, Luizon MR, et al. Vascular endothelial growth factor haplotypes associated with childhood smoking[J]. DNA Cell Biol, 2011,30(9):709-714.
[11] Lee EJ, Oh B, Lee JY, et al. Association study between single nucleotide polymorphisms in the VEGF gene and polycystic ovary syndrome[J]. Fertil Steril, 2008,89(6):1751-1759.
[12] Kuliczkowska Plaksej J, Laczmanski L, Milewicz A, et al. Cannabinoid receptor 1 gene polymorphisms and nonalcoholic Fatty liver disease in women with polycystic ovary syndrome and in healthy controls[J]. Int J Endocrinol, 2014,2014:232975.
[13] Bohdanowicz-Pawlak A, Lenarcik-Kabza A, Brona A, et al. Non-alcoholic fatty liver diseasein women with polycystic ovary syndrome-clinical and metabolic aspects and lipoprotein lipase gene polymorphism [J]. Endokrynol Pol, 2014,65(6):416-421.
[14] Zhang LW, Li JP, Duan FF, et al. Interaction of type 2 diabetes mellitus with chromosome 9p21 rs10757274 polymorphism on the risk of myocardial infarction: a case-control study in Chinese population[J]. BMC Cardiovasc Disord, 2014(14):170.
[15] Fesinmeyer MD, North KE, Lim U, et al. Effects of smoking on the genetic risk of smoking: the population architecture using genomics and epidemiology study[J]. BMC Med Genet, 2013(14):6.
Gene polymorphism of VEGF and its interaction with smoking in patients with non-alcoholic fatty liver disease
WANGQian,WUPengbo,LIMing,LUOHesheng,YUYuanjie,TANShiyun,SHUYongxiang
(RenminHospitalofWuhanUniversity,Wuhan430060,China)
Abstract:ObjectiveTo observe the gene polymorphisms of vascular endothelial growth factor (VEGF) rs833061 and rs3025039 and to investigate their interaction with smoking in patients with non-alcoholic fatty liver disease (NAFLD). MethodsGenotypes of VEGF rs833061 and rs3025039 in 341 patients with NAFLD (NAFLD group) and 246 control subjects (control group) were examined by polymerase chain reaction-based restriction fragment length polymorphism (PCR-RFLP). The unconditional logistic regression (ULR) was performed to analyze the relationships between the genotypes and susceptibility to NAFLD. The interactions between genotypes of VEGF rs833061 and rs3025039 and smoking in inducing NAFLD were explored by generalized multifactor dimensionality reduction (GMDR) and unconditional Logistic regression method. ResultsThe risk of NAFLD in VEGF rs833061 with genotype C (CC+CT) was higher than that of carriers without C (TT) (all P<0.01), and the risk of NAFLD in rs3025039T gene carriers (TT+CT) was higher than that of carriers without genotype T (CC) (all P<0.01). Gene polymorphism of VEGF rs833061 had interactions with smoking in the process of NAFLD (P<0.01). The risk of NAFLD in rs833061 CC/CT genotype of smoking individuals was 4.93 times higher than that of TT genotype of non-smoking individuals. ConclusionsVEGF gene polymorphism is associated with the risk of NAFLD. VEGF rs833061 and smoking have synergistic effects in the process of inducing NAFLD.
Key words:non-alcoholic fatty liver disease; vascular endothelial growth factor; gene polymorphisms; susceptibility; interaction
(收稿日期:2015-07-24)
中图分类号:R575.5
文献标志码:A
文章编号:1002-266X(2016)08-0007-03
doi:10.3969/j.issn.1002-266X.2016.08.003
通信作者简介:谭诗云(1962-),男,主任医生,教授,研究方向为肝脏相关疾病的基础与临床。E-mail: tanshiyun@126.com
作者简介:第一王倩(1989-),女,硕士在读,研究方向为非酒精性脂肪肝的诊治。E-mail: 1028578861@qq.com
基金项目:湖北省自然科学基金重点项目(2014CFA045)。