腓骨远端巨细胞瘤合并同侧胫骨血管脂肪瘤一例报告
张增亮 陈秉耀 李南 宋光泽 韦兴
. 病例报告 Case report .
腓骨远端巨细胞瘤合并同侧胫骨血管脂肪瘤一例报告
张增亮 陈秉耀 李南 宋光泽 韦兴
青少年;骨骺;骨巨细胞瘤;脂肪瘤骨肿瘤
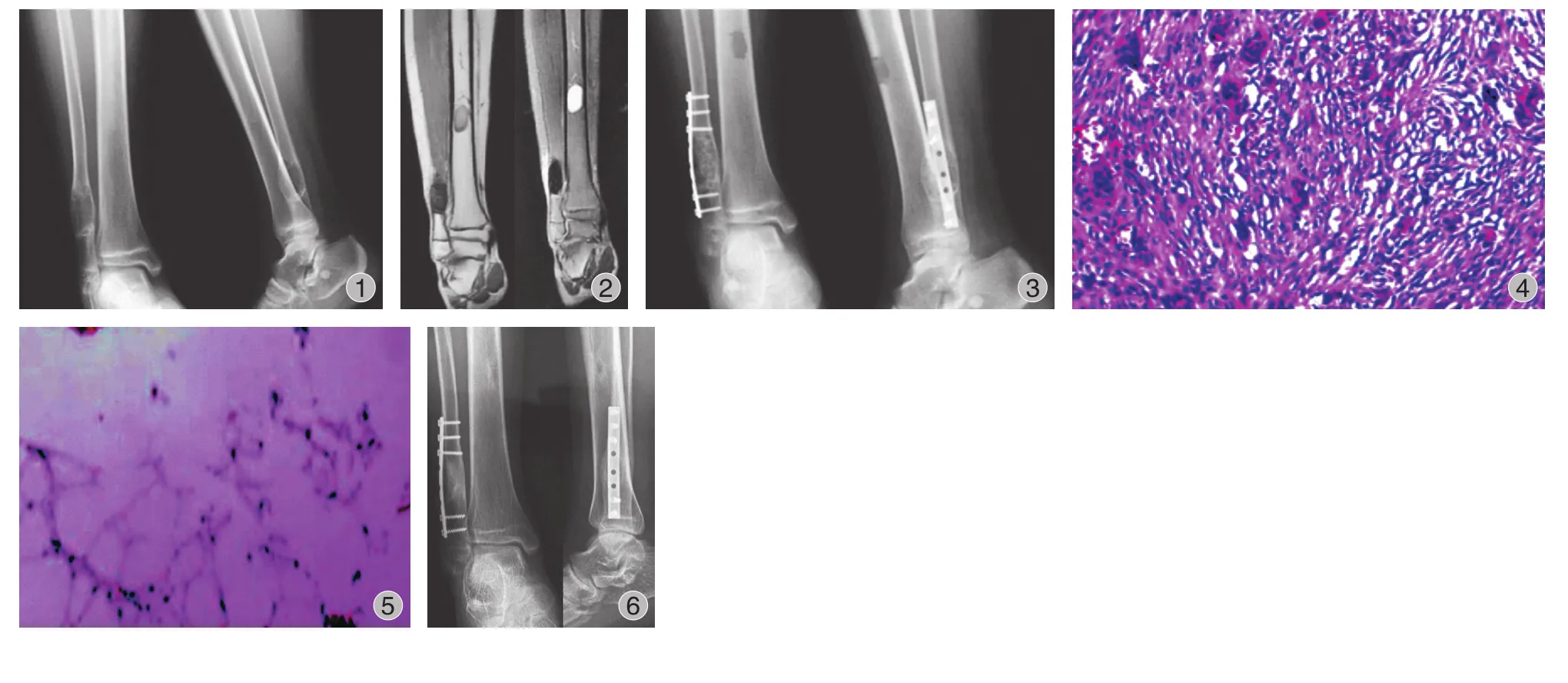
患儿,男,15 岁,右踝部间断疼痛 2 年,加重伴右踝部肿胀 1 周。查体:右外踝上 6 cm 处略肿胀,局部皮温正常,未触及包块,局部压痛明显,右踝关节活动度基本正常。右胫腓骨正侧位平片 ( 图 1 ):右腓骨远端干骺端膨胀性骨破坏,骨密度减低,骨皮质变薄,病灶内有分房,未见骨膜反应及周围软组织影。
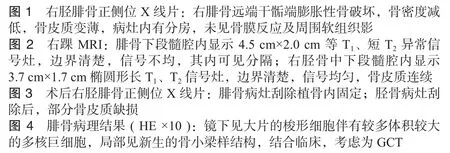
胫骨中下段髓腔内可见类圆形影,边界清楚,骨皮质无破坏。右踝 MRⅠ 示:腓骨下段髓腔内显示 4.5 cm× 2.0 cm 等 T1、短 T2异常信号灶,边界清楚,信号不均,其内可见分隔,病灶呈膨胀性生长,骨皮质变薄 ( 图 2 )。右胫骨中下段髓腔内显示 3.7 cm×1.7 cm 椭圆形长 T1、T2信号灶,边界清楚,信号均匀,边缘规则,骨皮质连续。结合病史及影像学表现考虑为良性病变,遂在硬膜外麻醉下行右腓骨远端病灶刮除、异体骨植骨、内固定术,右胫骨病灶刮除术。术中见:距外踝尖 10 cm 处病变,腓骨皮质局部隆起,切开骨膜,开窗,见骨皮质变薄,局部骨破坏,刮勺刮取褐色质软病变组织,术中考虑骨巨细胞瘤( giant cell tumor,GCT ) 可能性大,彻底刮除至骨质,电刀烧灼瘤腔,取异体骨,植入瘤腔内。选择合适长度钢板,行内固定重建腓骨稳定性。取右小腿内侧切口,见右胫骨中下段骨皮质未见破坏,透视定位下,卵圆形开窗,刮勺刮出黄色脂肪样质软组织。髓腔通畅,考虑骨皮质强度无影响,未植骨及内固定。术后右胫腓骨正侧位平片提示内固定位置良好 ( 图 3 )。
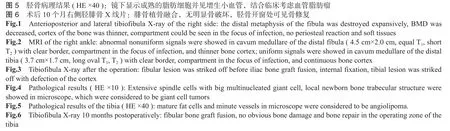
术后病理报告:( 1 ) 右腓骨远端髓腔内有 5.0 cm× 4.5 cm×1.3 cm 肿块。镜下见大片的梭形细胞伴有较多体积较大的多核巨细胞,局部见新生的骨小梁样结构,结合临床,考虑为 GCT ( 图 4 )。( 2 ) 右胫骨远端髓腔内见灰黄色结节肿物,总体积 3.5 cm×3.0 cm×1.0 cm,镜下显示成熟的脂肪细胞并见增生小血管,结合临床考虑血管脂肪瘤 ( 图 5 )。术后 2 周切口愈合良好,无红肿渗出现象,术后 3 个月患肢行走步态接近正常。术后 10 个月 X 线片见腓骨植骨融合,无明显骨破坏,胫骨开窗处可见骨修复( 图 6 )。
讨 论
GCT 是最常见的原发性骨肿瘤之一,占所有原发性骨肿瘤的 4%~5%,占所有良性肿瘤的 18%,多在 20~40 岁发病,女性较男性更为常见。本病 20 岁以下患者少见,其占 GCT 患者总数的 1.7%~5.7%[1],发生于骨骺未闭合患者仅占 1.8%~10.6%,多发生于骺端[3-6],邻近关节面,大部分呈偏心性。本例 GCT 发生于骨骺未闭患者,病灶主要位于长骨的干端,向骺端延伸,为非典型性 GCT[4]。GCT 的临床表现并无特异性,可以有局部的肿胀,疼痛,活动受限,部分患者可出现病理性骨折。影像学是诊断 GCT 的重要手段,但是确诊需要活检病理来证实。对于骨骺闭合前 GCT 的外科治疗,一方面要考虑肿瘤学的治疗,另一方面要考虑患者的生长发育,尽量降低畸形发生率。目前,GCT 的手术治疗方式主要包括:肿瘤囊内切除术和瘤段切除术。多数文献报道病灶刮除术后MTST 评分高于瘤段切除术,且在瘤段切除、关节重建术后的并发症要高于扩大切除术,包括骨折、骨不连、假体松动、假体感染等。徐立辉等[7]报道 8 例骨骺闭合前 GCT患者中有 6 例行扩大刮除术,其中没有出现肢体发育畸形或者肢体不等长,未出现转移病例,也提示扩大刮除术对于骨骺闭合前的患者是安全有效的手术方法。
血管脂肪瘤 ( angiolipoma ) 是一种少见的良性肿瘤[8],临床上青少年多发,国内也仅见少数的病例报道[2]。1960年,Howard 等[9]首先确定血管脂肪瘤作为病理诊断,其中包含了成熟的脂肪组织和血管。该病在临床缺乏特异性表现,MRⅠ 显示肿块多呈梭形,T1WⅠ 为中等偏高信号,较脂肪组织信号低,T2WⅠ 为高信号,肿物内有扭曲扩张的血管影为其特异性表现,本病若血管成分少,与脂肪瘤难鉴别[10]。治疗方面,本病以手术彻底切除为主[11],复发率较低。
肢体两个部位同时出现肿瘤,常被认为是转移或者多发。本例提示,当同一肢体影像学上显示不同的病灶,要想到可能是不同的疾病,进而选择不同的治疗方案。血管脂肪瘤和巨细胞瘤的同时出现并没有明确的原因,两者没有直接联系。本例青少年患者在骨骺闭合前发生腓骨远端GCT,合并同侧胫骨骨内血管脂肪瘤,比较罕见。
[1] Morgan JD, Eady JL. Giant cell tumor and the skeletally immature patient. J South Orthop Assoc, 1999, 8(4):275-284.
[2] 孙鹏飞, 贾玉华. 骶骨血管脂肪瘤一例. 中华外科杂志, 2006, 44(24):1682.
[3] 徐万鹏, 冯传汉. 骨科肿瘤学. 北京: 人民军医出版社. 2008: 265-268.
[4] Puri A, Agarwal MG, Shah M, et al. Giant cell tumor of bone in children and adolescents. J Pediatr Orthop, 2007, 27(6): 635-639.
[5] Picci P, Manfrini M, Zucchi V, et al. Giant-cell tumor of bone in skeletally immature patients. J Bone Joint Surg Am, 1983, 65(4):486-490.
[6] Schutte HE, Taconis WK. Giant cell tumor in children and adolescents. Skeletal Radiol, 1993, 22(3):173-176.
[7] 徐立辉, 张清, 郝林, 等. 骨骺闭合前骨巨细胞瘤的诊断和治疗. 中华外科杂志, 2013, 51(9):827-830.
[8] Dogan S, Arslan E, Sahin S, et al. Lumbar spinal extradural angiolipomas: two case reports. Neurol Med Chir (Tokyo), 2006, 46(3):157-160.
[9] Howard WR, Helwig EB. Angiolipoma. Arch Dematol, 1960, 82:924.
[10] Murphey MD, Carrol JF, Flemming DJ, et al. From the archives of the AFⅠP: benign musculoskeletal lipomatous lesions. Radiographics, 2004, 24(5):1433-1466.
[11] do Souto AA, Domingues FS, Chimelli L, et al. Lumbosacral angiolipoma: case report. Arq Neuropsiquiatr, 2003, 61(2A): 269-273.
( 本文编辑:李贵存 )
Giant cell tumor of the distal fibula combined with ipsilateral angiolipoma in the tibia: 1 case report
ZHANG Zeng-liang, CHEN Bing-yao, LI Nan, SONG Guang-ze, WEI Xing.
Musculoskeletal Tumor Center, Department of Orthopedics, the first Affiliated Hospital of PLA General Hospital, Beijing, 100048, PRC
WEⅠ Xing, Email: 87032038@qq.com
Objective To report a case of giant cell tumor of the distal fibula combined with ipsilateral angiolipoma in the tibia. Methods A male patient ( 15 years old ) complained with the intermittent pain in the right ankle for 2 years which was aggravated in one week. Physical examination: swelling of 6cm to the right lateral superior condyle, normal local temperature, no mass, no local tenderness, no limitations of the ankle function. Tibiofibula X-ray of right side: distal metaphysis of the fibula was destroyed expansively, bone mineral density ( BMD ) was decreased, cortex of the bone was thinner, compartment could be seen in the focus of infection, no periosteal reaction or soft tissues. MRⅠ of the right ankle: abnormal nonuniform signals were showed in cavum medullare of the distal fibula ( 4.5 cm×2.0 cm, equal T1, short T2) with clear border, compartment in the focus of infection, and thinner bone cortex; uniform signals were showed in cavum medullare of the distal tibia ( 3.7 cm×1.7 cm, long oval T1, T2) with clear border, compartment in the focus of infection, and continuous bone cortex. Curettage of foci in the right distal fibula and tibia, allograft bone transplant and internal fixation were conducted under epidural anesthesia. Results Pathological results: ( 1 ) 5.0 cm×4.5 cm×1.3 cm mass in the cavum medullare of the distal fibula. Extensive spindle cells with big multinucleated giant cell, local newborn bone trabecular structure were showed in microscope, which were considered to be giant cell tumors. ( 2 ) 3.5 cm×3.0 cm×1.0 cm drab yellow nodule mass in the cavum medullare of the distal tibia. Mature fat cells and minute vessels in microscope were considered to be angiolipoma. Tibiofibula X-ray 10 months postoperatively: fibular bone graft fusion, no obvious bone damage and bone repair in the operating zone of the tibia. Conclusions Giant cell tumor of the distal fibula combined with ipsilateral angiolipoma in the tibia was rare in adolescent patients before the epiphyseal closure.
Adolescent; Epiphyses; Giant cell tumor of the bone; Lipoma, bone neoplasms
sn.2095-252X.2015.10.016
R738.1
100048 北京,解放军总医院第一附属医院骨科、北京市骨科植入医疗器械工程技术研究中心
韦兴,Email: 87032038@qq.com
2015-01-19 )

