心脏内科住院患者阻塞性睡眠呼吸暂停低通气综合征的患病风险及预后的关系
赵良平,王学斌,王莉,陈建昌,徐卫亭,佟光明,杨向军
心脏内科住院患者阻塞性睡眠呼吸暂停低通气综合征的患病风险及预后的关系
赵良平,王学斌,王莉,陈建昌,徐卫亭,佟光明,杨向军
目的通过柏林问卷筛查心脏内科住院患者阻塞性睡眠呼吸暂停低通气综合征(OSAHS)的高危人群,评价OSAHS高危与心血管疾病患者预后的关系。方法选取2013年1月—2014年1月苏州大学附属第二医院心脏内科住院患者618例为研究对象,入院病情稳定后进行柏林问卷调查,根据评分将患者分为OSAHS高危组(≥2分,274例)和OSAHS低危组(≤1分,344例)。收集患者既往病史、现病史资料和随访1年后再住院、心因性死亡发生情况。结果OSAHS高危组年龄、颈围、体质量、体质指数(BMI)、身高校正的颈围、既往脑血管意外及高血压、糖尿病、高脂血症、慢性肾功能不全患病率高于OSAHS低危组(P<0.05)。随访期间,OSAHS高危组患者再住院70例(25.5%),OSAHS低危组患者再住院52例(15.1%),OSAHS高危组再住院率高于OSAHS低危组(χ2= 10.470,P=0.002)。OSAHS高危组患者心因性死亡17例(6.2%),OSAHS低危组患者心因性死亡4例(1.2%),OSAHS高危组心因性病死率高于OSAHS低危组(χ2=11.810,P=0.001)。多因素Logistic回归分析结果显示,既往脑血管意外〔b=0.571,OR=1.763,95%CI(1.017,3.085),P=0.045〕和高危OSAHS〔b=0.560,OR=1.751,95%CI(1.084,2.828),P=0.022〕是心脏内科住院患者再住院的危险因素;高危OSAHS〔b=1.157,OR=3.182,95%CI(1.045,9.687),P=0.042〕是心脏内科住院患者心因性死亡的危险因素。结论心血管疾病患者OSAHS高危人群合并高血压的比例较高,发生不良预后的风险增加。
睡眠呼吸暂停,阻塞性;心血管疾病;影响因素分析;预后
赵良平,王学斌,王莉,等.心脏内科住院患者阻塞性睡眠呼吸暂停低通气综合征的患病风险及预后的关系[J].中国全科医学,2015,18(32):3918-3921.[www.chinagp.net]
Zhao LP,Wang XB,Wang L,et al.Relationship Between High Risk for Obstructive Sleep Apnea Hypopnea Syndrome and Prognosis of PatientsWith Cardiovascular Diseases[J].Chinese General Practice,2015,18(32):3918-3921.
阻塞性睡眠呼吸暂停低通气综合征(OSAHS)是以睡眠时反复部分或完全上呼吸道梗阻为特征,表现为反复发生的呼吸暂停或低通气,伴有间歇性低氧血症和高碳酸血症的疾病。据报道,成年人群OSAHS患病率低于5%[1-2],60岁以上人群OSAHS患病率高于30%[3]。OSAHS与心肌梗死、心绞痛、心律失常、心力衰竭等心血管疾病的发生有关,其机制可能为OSAHS间歇性低氧所致氧化应激、炎性反应、血管内皮细胞损伤等[4]。柏林问卷评估OSAHS简单、方便,与多导睡眠监测诊断OSAHS总符合率较高[5-6]。本研究采用柏林问卷筛查心脏内科住院患者发生OSAHS高危人群,并分析OSAHS与患者预后的关系。
1 对象与方法
1.1研究对象选取2013年1月—2014年1月苏州大学附属第二医院心脏内科住院患者618例为研究对象,其中男414例,女204例;年龄19~95岁,平均年龄(63.5±14.8)岁。排除标准:(1)不同意接受问卷调查;(2)意识丧失,无能力接受问卷调查;(3)合并恶性肿瘤。本研究经本院伦理委员会批准,患者均知情并同意。
1.2研究方法
1.2.1柏林问卷调查患者于入院病情稳定后自行填写柏林问卷[5],无法自行填写者由研究者询问。根据柏林问卷评分将患者分为OSAHS高危组(≥2分,274例)和OSAHS低危组(≤1分,344例)。
1.2.2临床资料测量患者颈围、身高、体质量,计算体质指数(BMI)和身高校正的颈围(颈围/身高)。记录患者临床特征,包括冠心病家族史,既往吸烟史,脑血管意外、心肌梗死病史,经皮冠状动脉介入治疗(PCI)史,合并高血压、糖尿病、高脂血症、慢性肾功能不全及主要诊断。
1.2.3随访问卷调查后对患者进行1年的随访,记录再住院和心因性死亡(猝死或死于心肌梗死、心力衰竭、恶性心律失常)发生情况。
1.3统计学方法采用SPSS 17.0软件进行统计分析,计量资料以(±s)表示,组间比较采用独立样本t检验;计数资料采用相对数表示,组间比较采用χ2检验;采用多因素Logistic回归模型分析再住院和心因性死亡的危险因素。以P<0.05为差异有统计学意义。
2 结果
2.1两组临床资料比较OSAHS高危组与OSAHS低危组性别、身高、冠心病家族史、吸烟、既往心肌梗死、PCI史及主要诊断比较,差异无统计学意义(P>0.05)。OSAHS高危组年龄、颈围、体质量、BMI、身高校正的颈围、既往脑血管意外及高血压、糖尿病、高脂血症、慢性肾功能不全患病率高于OSAHS低危组(P<0.05,见表1)。
2.2再住院率随访期间,OSAHS高危组患者再住院70例(25.5%),OSAHS低危组患者再住院52例(15.1%),OSAHS高危组再住院率高于OSAHS低危组(χ2=10.470,P=0.002)。以患者各临床特征为自变量,是否发生再住院为因变量行多因素Logistic回归分析,结果显示,既往脑血管意外〔b=0.571,OR= 1.763,95%CI(1.017,3.085),P=0.045〕、高危OSAHS〔b=0.560,OR=1.751,95%CI(1.084,2.828),P=0.022〕进入回归方程,是心脏内科住院患者再住院的危险因素。
2.3心因性病死率随访期间,OSAHS高危组患者心因性死亡17例(6.2%),OSAHS低危组患者心因性死亡4例(1.2%),OSAHS高危组心因性病死率高于OSAHS低危组(χ2=11.810,P=0.001)。以患者各临床特征为自变量,以是否发生心因性死亡为因变量行多因素Logistic回归分析,结果显示,高危OSAHS〔b= 1.157,OR=3.182,95%CI(1.045,9.687),P= 0.042〕进入回归方程,是心脏内科住院患者心因性死亡的危险因素。
3 讨论
调查显示,近年OSAHS患病率呈上升趋势。Gislason等[7]于1988年报道欧洲国家OSAHS患病率为1.0%~2.7%,高雪梅等[8]于1997年报道国内OSAHS患病率为1.2%~3.7%。而2009年美国睡眠医学协会报道成人OSAHS的患病率达2%~4%[9],我国近年不同地区的调查显示OSAHS患病率为4.2%~9.6%[2,10-11]。
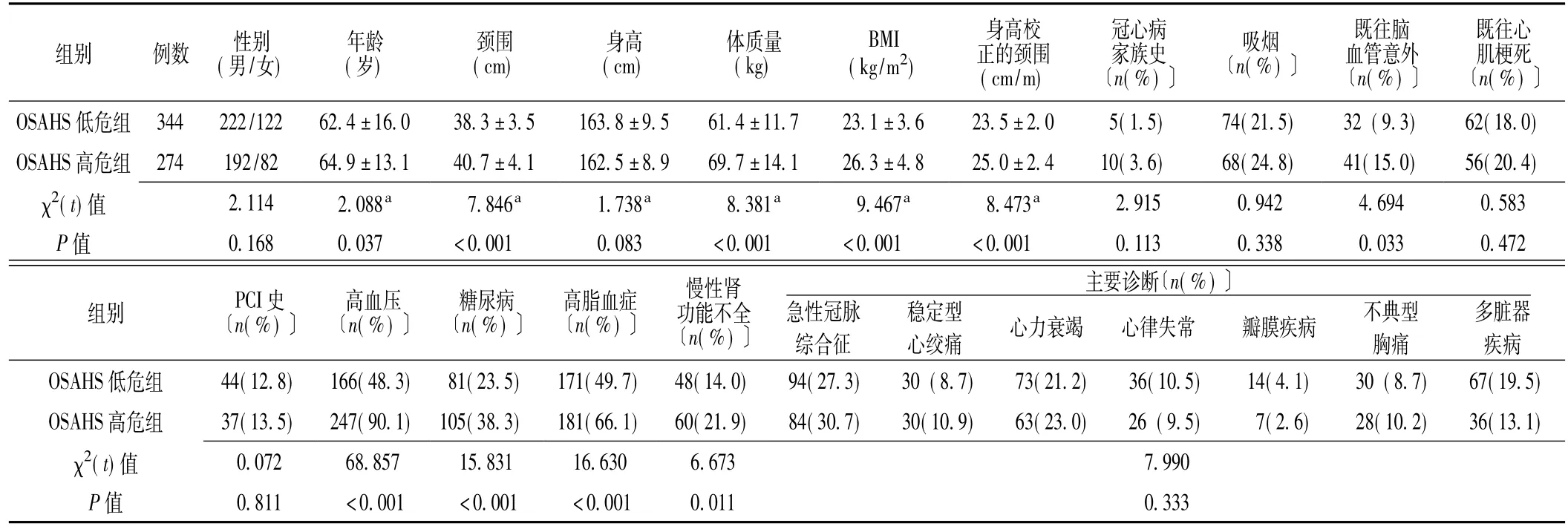
表1 两组患者临床资料比较Table 1 Comparison of clinical characteristics between the two groups
柏林问卷是筛查OSAHS简单、有效方法,多位学者分别对手术治疗患者[5]、诊室疑似OSAHS患者[6]和普通人群[12]进行柏林问卷评估和多导睡眠监测,柏林问卷均显示出较好的灵敏度和特异度。OSAHS是冠心病、心力衰竭、心律失常、高血压、肺动脉高压等心血管疾病发病与不良预后的重要危险因素[13-16]。美国心脏病学会基金会(ACCF)和美国心脏协会(AHA)《睡眠呼吸暂停与心血管疾病专家共识》指出,50%的OSAHS患者合并高血压,而至少30%的高血压患者伴有OSAHS[17]。Gus等[18]对难治性高血压患者调查显示,78%的患者合并OSAHS。本研究结果显示,心脏内科住院患者OSAHS高危占44.3%(274/618),OSAHS高危和OSAHS低危人群分别有90.1%、48.3%的患者合并高血压。
Correia等[19]研究显示,在非ST段抬高型急性冠脉综合征患者中,合并OSAHS的患者住院期间心血管事件发生率高于不合并OSAHS的患者。同时,合并OSAHS的冠心病患者5年病死率为38%,高于无OSAHS患者的9%[20]。OSAHS患者睡眠过程中反复发生呼吸暂停,形成间歇性低氧血症和高碳酸血症,引起夜间交感神经功能亢进,儿茶酚胺分泌增多;另外,OSAHS患者夜间反复的低氧、再氧和促使白细胞活化,炎性因子释放增加和超氧化物自由基产生过多,损伤血管内皮功能[4],从而对心血管疾病患者的预后产生不良影响。本研究多因素Logistic回归分析结果显示,高危OSAHS是心脏内科患者1年内再住院和心因性死亡的危险因素。
研究表明,普通人群男性OSAHS患病率高于女性,约为2∶1~3∶1[21]。分析其原因为:(1)女性孕激素和雌激素对上呼吸道扩张肌具有激活作用,避免睡眠时的气道塌陷;(2)女性体内瘦素水平高于男性,而瘦素具有刺激呼吸的作用;(3)男性咽旁脂肪垫较女性厚,颈部软组织较女性多,因此更易导致睡眠时气道受压迫而塌陷;(4)男性喉部面积大、脆弱、变化性大,易在睡眠时发生改变;而女性上呼吸道虽较男性窄,但硬度高,因此较男性不易发生塌陷[22]。本研究显示,OSAHS高危组和OSAHS低危组患者性别构成并无差异,可能为心脏内科女性患者年龄较高,多数已绝经,孕激素和雌激素对气道的保护作用丧失和气道硬性降低。
本研究为单中心研究,采用柏林问卷筛查OSAHS,准确性低于多导睡眠监测。在下一步的研究中,应纳入多中心的心血管疾病患者,采用多导睡眠监测筛查OSAHS人群,并延长随访时间,进一步分析OSAHS与心血管疾病预后的关系。
[1]Shepertycky MR,Banno K,Kryger MH.Differences between men and women in the clinical presentation of patients diagnosed with obstructive sleep apnea syndrome[J].Sleep,2005,28(3):309-314.
[2]虎迎春,张锦,程英.宁夏地区睡眠呼吸暂停低通气综合征的流行问卷调查[J].中国实用内科杂志,2011,31(2):119-121.
[3]Janssens JP,Pautex S,Hilleret H,et al.Sleep disordered breathing in the elderly[J].Aging(Milano),2000,12(6):417-429.
[4]Zhu LX,Tong GM,You T,et al.Clinical study on QT dispersion and cardiac arrhythmia in patientswith sleep apnea hypopnea syndrome[J].Chinese General Practice,2013,16(10):3551-3553.(in Chinese)朱凌霞,佟光明,尤涛,等.睡眠呼吸暂停低通气综合征患者QT离散度及心律失常临床研究[J].中国全科医学,2013,16(10):3551-3553.
[5]Chung F,Yegneswaran B,Liao P,et al.Validation of the Berlin questionnaire and American Society of Anesthesiologists checklist as screening tools for obstructive sleep apnea in surgical patients[J].Anesthesiology,2008,108(5):822-830.
[6]Lyu XP,Zhang C,Ma J,et al.Application of Berlin questionnaire in the screening of obstructive sleep apnea hypopnea syndrome[J].Chinese Journal of Tuberculosis and Respiratory Diseases,2011,34 (7):515-519.(in Chinese)吕向裴,张成,马靖,等.柏林问卷在阻塞性睡眠呼吸暂停低通气综合征筛查中的应用价值[J].中华结核和呼吸杂志,2011,34(7):515-519.
[7]Gislason T,Almqvist M,Eriksson G,et al.Prevalence of sleep apnea syndrome among Swedish men——an epidemiological study[J].JClin Epidemiol,1988,41(6):571-576.
[8]高雪梅,赵颖,曾祥龙,等.北京地区鼾症和睡眠呼吸暂停综合征的流行病学研究[J].口腔正畸学,1997,4(4):162-165.
[9]Epstein LJ,Kristo D,Strollo PJ Jr,et al.Clinical guideline for the evaluation,management and long-term care of obstructive sleep apnea in adults[J].JClin Sleep Med,2009,5(3):263-276.
[10]Zhao Y,Li JR,Wang LW,et al.Epidemiological investigation on snoring and obstructive sleep apnea-hypopnea syndrome among the adults in Chaoyang District of Beijing City[J].China Medical Herald,2013,10(27):108-111.(in Chinese)赵阳,李建瑞,王利伟,等.北京市朝阳区成人打鼾及阻塞性睡眠呼吸暂停低通气综合征流行病学调查[J].中国医药导报,2013,10(27):108-111.
[11]葛瑞锋,刘文君,梅栩彬,等.青岛地区阻塞性睡眠呼吸暂停低通气综合征的患病率及影响因素的相关性分析[J].中国耳鼻咽喉颅底外科杂志,2009,15(4):272-275.
[12]Netzer NC,Stoohs RA,Netzer CM,et al.Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome[J].Ann Intern Med,1999,131(7):485-491.
[13]睡眠呼吸暂停与心血管疾病专家共识组.睡眠呼吸暂停与心血管疾病专家共识[J].中华内科杂志,2009,48(12):1059-1067.
[14]Jesus EV,Dias-Filho EB,Mota Bde M,et al.Suspicion of obstructive sleep apnea by Berlin Questionnaire predicts events in patients with acute coronary syndrome[J].Arq Bras Cardiol,2010,95(3):313-320.
[15]Patidar AB,Andrews GR,Seth S.Prevalence of obstructive sleep apnea,associated risk factors,and quality of life among Indian congestive heart failure patients:a cross-sectional survey[J].J Cardiovasc Nurs,2011,26(6):452-459.
[16]Gami AS,Pressman G,Caples SM,et al.Association of atrial fibrillation and obstructive sleep apnea[J].Circulation,2004,110(4):364-367.
[17]Somers VK,White DP,Amin R,et al.Sleep apnea and cardiovascular disease:an American Heart Association/american College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee,Council on Clinical Cardiology,Stroke Council,and Council on Cardiovascular Nursing[J].JAm Coll Cardiol,2008,118(10):1080-1111.
[18]Gus M,Goncalves SC,Martinez D,et al.Risk for Obstructive Sleep Apnea by Berlin Questionnaire,but not daytime sleepiness,is associated with resistant hypertension:a case-control study[J].Am JHypertens,2008,21(7):832-835.
[19]Correia LC,Souza AC,Garcia G,et al.Obsructive sleep apnea affects hospital outcomes of patients with non-ST-elevation acute coronary syndrome[J].Sleep,2012,35(9):1241-1245.
[20]Peker Y,Hedner J,Kraiczi H,et al.Respiratory disturbance index:an independent predictor of mortality in coronary artery disease[J].Am JRespir Crit Care Med,2000,162(1):81-86.
[21]Jordan AS,McEvoy RD.Gender differences in sleep apnea: epidemiology,clinical presentation and pathogenic mechanisms[J].Sleep Med Rev,2003,7(5):377-389.
[22]Kapsimalis F,Kryger MH.Gender and obstructive sleep apnea syndrome,part 2:mechanisms[J].Sleep,2002,25(5): 499-506.
(本文编辑:吴立波)
Relationship Between High Risk for Obstructive Sleep Apnea Hypopnea Syndrome and Prognosis of Patients W ith Cardiovascular Diseases
ZHAO Liang-ping,WANG Xue-bin,WANG Li,et al.Department of Cardiology,the SecondAffiliated Hospital of Soochow University,Suzhou 215004,China
Objective To investigate the relationship between high risk for obstructive sleep apnea hypopnea syndrome (OSAHS)and prognosis of patientswith cardiovascular diseases,through the screening of high risk for OSAHSamong cardiology department inpatients by Berlin questionnaire.M ethods We enrolled 618 inpatients of the Department of Cardiology of the Second Affiliated Hospital of Soochow University from January 2013 to January 2014.After the illness got stable,the subjects were administrated with Berlin questionnaire.According to the scores,the subjects were divided into OSAHS high-risk group (≥2,n=274)and OSAHS low-risk group(≤1,n=344).We collected data concerning medical history,history of present illness,readmission after one-year follow-up and psychogenic death.Results The high-risk group was higher(P<0.05)than the low-risk group in age,neck circumference,body mass,BMI,neck circumference after height correction and the proportions of patients with previous cerebrovascular accidents,complicated hypertension,diabetes mellitus,hyperlipemia and chronic renal insufficiency.During the follow-up,70(25.5%)patients in high-risk group and 52 (15.1%)patients in low-risk group were readmitted into the hospital,the high-risk group having higher readmission rate thanthe low-risk group(χ2=10.470,P=0.002).Psychogenic death occurred in 17(6.2%)patients in high-risk OSAHS group and 4(1.2%)patients in low-risk group,the high-risk group having higher psychogenicmortality rate than low-risk group(χ2=11.810,P=0.001).Themultivariate Logistic regression analysis showed that previous cerebrovascular accidents〔b=0.571,OR=1.763,95%CI(1.017,3.085),P=0.045〕and high risk for OSAHS〔b=0.560,OR=1.751,95% CI(1.084,2.828),P=0.022〕were risk factors for the readmission of cardiology department inpatients;high risk for OSAHS〔b=1.157,OR=3.182,95%CI(1.045,9.687),P=0.042〕were risk factors for psychogenic death of cardiology department inpatients.Conclusion Patients with cardiovascular diseases and high risk for OSAHS have higher incidence of complicated hypertension and higher risk in adverse prognosis.
Sleep apnea,obstructive;Cardiovascular diseases;Root cause analysis;Prognosis
R 563.8
A
10.3969/j.issn.1007-9572.2015.32.006
苏州市科技发展计划项目(SYS201237)
215004江苏省苏州市,苏州大学附属第二医院心脏内科(赵良平,王学斌,王莉,陈建昌,徐卫亭,佟光明);苏州大学附属第一医院心脏内科(杨向军)
佟光明,215004江苏省苏州市,苏州大学附属第二医院心脏内科;E-mail:tgm1@sina.com
2015-03-10;
2015-06-11)

