颈椎椎管成形术治疗多节段颈椎管狭窄
卓成龙 丁立祥
颈椎椎管成形术治疗多节段颈椎管狭窄
卓成龙 丁立祥
丁立祥 教授
多节段颈椎管狭窄的原因有很多,其中最为常见的是颈椎病或后纵韧带骨化(ossification of posterior longitudinal ligament, OPLL)。椎管减压既可以前路进行,也可以选择后路进行。对于多节段病变,尤其伴有OPLL患者,由于手术安全性的考虑,其手术方案倾向于采用后路减压。后路颈椎减压手术包括椎板切除术和椎管成形术,其中以椎管成形术最为常用,根据椎管成形减压方式差异,其主要术式分为2大类:单开门与双开门椎管成形术[1-2]。而此2种基本术式又衍生出诸多手术术式,并于临床或基础方面又有了新的研究。
1 手术适应证
椎管成形术可以在不用去除前方病变的条件下,间接解除脊髓和神经根管的压迫。通过保留后方结构,该术式可以维持脊柱稳定和力线,减少因椎板切除引起的后凸和不稳[3]。绝大部分学者均认为后路手术的指征是[4-5]:(1)≥3 个节段的脊髓型颈椎病或影像学提示多节段脊髓腹背侧受压者;(2)发育性和退变性颈椎管狭窄所致颈脊髓病(包括颈椎管狭窄合并无骨折脱位型颈脊髓损伤);(3)多节段受累的颈椎OPLL所致颈脊髓病;(4)黄韧带肥厚或骨化压迫脊髓背侧所致颈脊髓病;(5)颈前路术后疗效不佳者。Braly等[5]认为禁忌证是既往颈椎后路手术病史、黄韧带骨化、硬膜外纤维化患者。
Hirabayashi等[6]通过CT比较单开门和双开门颈椎椎管在C5、C6扩大的程度,确定两者的手术适应证。单开门适应证是脊髓型颈椎病(CSM)伴单侧神经根病变、重度凸出的OPLL、棘突太小无法行双开门者,双开门适应证是通常的CSM、小和轻微凸出的OPLL、CSM伴双侧神经根病变、颈椎管狭窄伴不稳定(必须后路脊柱内固定手术)者。
2 术式的近期发展
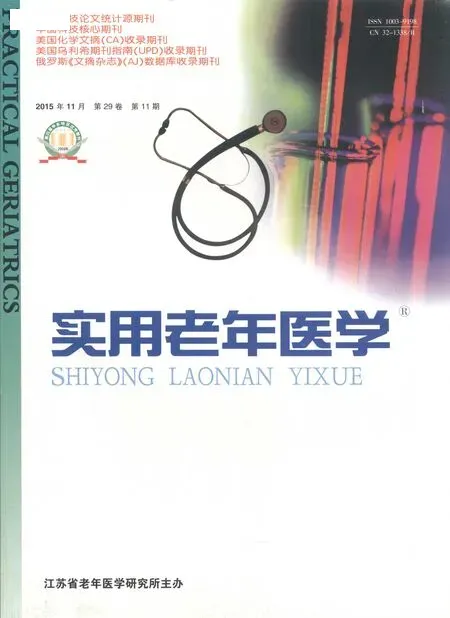
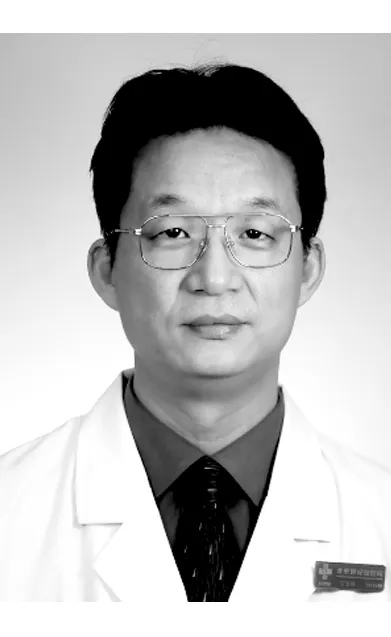
2.1 单开门椎管成形术 Hirabayashi术式影响深远,并不断涌现出不同的改良方法,如全(en-bloc)椎管成形术(Ito和Tsuji’s方法)(图1)。近期Ding等[7]对CSM伴发黄韧带肥厚患者施行C3、C5、C7椎板切除术并咬除肥厚的黄韧带,用Centerpiece钢板与棘突自体骨移植组装,对C4、C6椎板弓重建,铰链侧骨碎屑填充。Arantes Júnior等[8]对86例多节段脊髓型颈椎病(MCSM)患者采用一种新型的双开门术式(图2)。该术式对C3~C4椎板一侧单开门,而C5~C6椎板对侧单开门,这可对C5神经根双侧减压,C2/C7可行部分椎扳切除术,C2棘突与C3椎板、C4椎板与C5椎板、C6椎板与C7棘突分别进行缝线固定,首先和最重要的缝线固定是C4椎板与C5棘突。该术式疗效满意,不需要异体骨或其他固定材料,建议用于老年人。
Tabaraee等[9]发现金属微型板较结构性肋骨同种异体支柱手术时间短、术后制动少。Park等[10]发现只用钢板在早期骨愈合中不能提供足够的稳定,铰链侧会发生延迟的再骨折(9%,1周)。Chen等[11]认为Centerpiece微型板固定组较缝合悬挂组未增加完全骨折率,可能促进Ⅰ型完全铰链骨折的骨融合。
2.2 双开门椎管成形术 Kurokawa双开门术式也不断涌现出新的改良方法。近期Mehdain等[12]设计一种改良的Kurokawa术式,对C4、C5、C6棘突间置入骨块后,用3条颌面部钛板(16~18孔)、2 mm螺钉固定,术中共出血200 ml,2.5 h完成。钛板和骨块的组合不仅极大限度的增加椎管面积,且无“弹性回弹”,这种钛板廉价、速效,扩大后方骨性神经根管,保护骨肌肉组织便于术后运动。Oh等[13]在咬除棘突后,将PEEK板(MAXPACER°R)用2枚8 mm钛钉固定在撑开的椎板上。Harshavardhana等[14]将自体髂嵴骨填充在分开的棘突(C2、C7保留肌肉附着)间隙,微型钛板与前侧的移植骨锚定、用螺钉与后侧的结构固定,术后未使用外固定支具。
Park等[15]采用箱型椎管扩大成形术(图3)对36例OPLL和12例CSM患者进行减压,微型钢板置于两椎板之间,用8 mm的椎板间螺钉固定,箱型椎管扩大成形术可创造出最大程度的椎管扩大,椎板间螺钉固定良好且未造成神经功能缺损。Kim等[16]认为90°箱型椎管成形术可能会引起硬膜瘢痕组织形成、后凸,仍需长期随访。Tani等[17]使用钛质箱型棘突间隔物,两侧各有一臂便于螺钉固定。
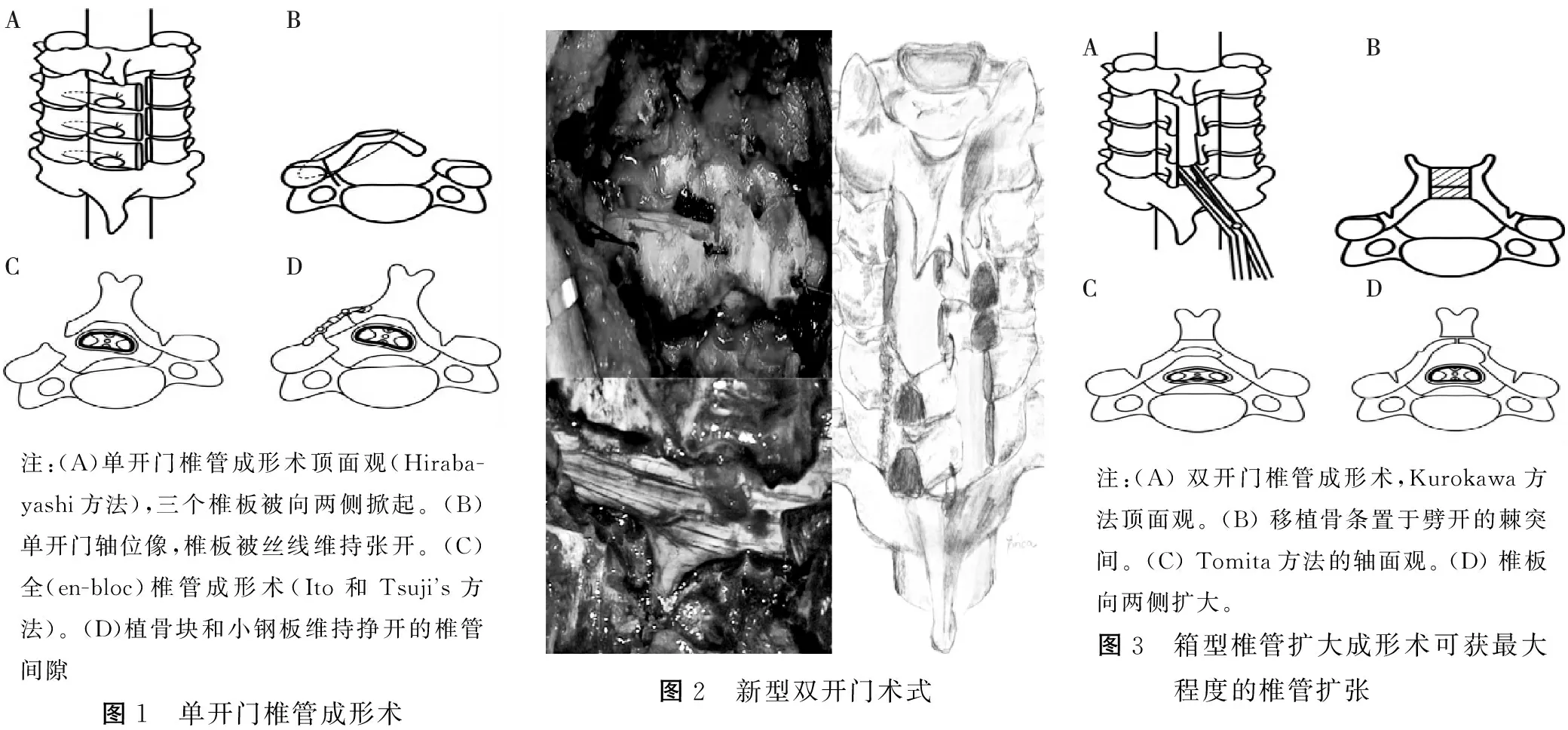
注:(A)单开门椎管成形术顶面观(Hiraba-yashi方法),三个椎板被向两侧掀起。(B)单开门轴位像,椎板被丝线维持张开。(C)全(en-bloc)椎管成形术(Ito和Tsujis方法)。(D)植骨块和小钢板维持挣开的椎管间隙图1 单开门椎管成形术图2 新型双开门术式注:(A)双开门椎管成形术,Kurokawa方法顶面观。(B)移植骨条置于劈开的棘突间。(C)Tomita方法的轴面观。(D)椎板向两侧扩大。图3 箱型椎管扩大成形术可获最大程度的椎管扩张
2.3 保留肌肉附着,重建复合体 在保留肌肉附着方面,Sakaura等[18]对保留C2、C7棘突的C3~C6椎管成形术随访平均9年,长期疗效满意。 Kotani等[19]保留颈多裂肌、颈半棘肌的附着,对减压节段已切除的棘突再缝合固定,术后在轴性痛、生活质量评分(QOL)、预防深部伸肌萎缩较传统术式表现出巨大优势。Shiraishi等[20]报道了几种新的术式,选择性单一椎管成形术、保留肌肉的椎间孔切开术、保留肌肉的后路寰枢椎内固定术。Umeda等[21]对C4~C6予以椎管成形术(用羟磷灰石间隔物),C3和C7部分椎板切除术,或C3椎板全切、C7部分椎板切除术。
在后方韧带复合体方面,Lin等[23]明确证实椎管成形术严重影响颈椎矢状位平衡,术后颈椎易于前倾,随着对复合体的破坏度增加,矢状位平衡的缺失增大。Sinha等[24]使用单侧后路中线路径予以双开门,保留后张力带和椎旁深层伸肌的附着,且未损伤附着在棘突上的对侧椎旁肌肉。Abdullah等[25]使用微型板伴异体支柱骨移植重建椎板,保留后方复合体。
2.4 椎管成形术联合内固定 在侧块固定方面,Jiang等[26]对CSM伴多节段椎管狭窄患者采用单开门联合侧块钢板螺钉固定,Chen等[27]对OPLL伴颈椎不稳予以后路椎管成形术联合侧块螺钉固定。刘永皑等[28]发现单开门联合侧块螺钉固定术后有较低的轴性症状(AS)发生率(6.0%)。
Miyamoto等[29]首次研究对CSM伴后凸畸形(>5°)患者予以单独椎管成形术(laminoplasty alone,LP)与使用椎弓根螺钉或侧块螺钉矫正后凸畸形的后路重建手术(posterior reconstruction surgery,PR)之间的差异,PR组、LP组JOA评分回复率分别为44.5%、32.6%,术后后凸角度分别为(4.0±8.6)°、(8.0±6.0)°,C2-7角度PR组改善至(-11.6±6.2)°、LP组恶化至(0.5±12.7)°。
Kim等[30]首次报道经关节突螺钉(transarticular screw,TAS)联合含HA间隔物的生物可吸收左旋聚丙交酯螺钉对C4/C5内固定,随访1年后确认C4/C5融合,生物活性螺钉被新生骨填充、HA促进骨诱导。
3 术后主要并发症
3.1 术后AS AS是指椎管成形术后遗留或发生颈肩背部疼痛、僵硬、颈项活动受限等症状,1999年Kawaguchi等[31]称为AS。Wang等[32]统计1996~2009年的26篇纳入1297例患者,AS的发生率为5.2%~61.5%。但也有文献发现术后有无轴性痛与术前即有轴性痛无关。认为椎管成形术可能不是造成AS的主要原因,但可被其加剧。轴性痛的潜在来源包括颈椎间盘、肌肉组织、关节突关节、脊髓和神经根。Sakaura等[33]证实保留枢椎下深部肌肉无异于减轻AS,认为椎管成形术后不良反应主要源于剥离C2、C7棘突的附着肌肉。在减少AS方面,Mesfin等[34]认为对C3施行椎板切除术而不是椎管成形术来保留颈半棘肌在C2的附着、尽量避免对C7施行椎管成形术以保留斜方肌和菱形肌的附着、对颈半棘肌及其筋膜予以精致的多层缝合以减少死腔和肌萎缩。Wang等[35]建议一些更加微创的椎管成形术、术后早期颈椎活动度(ROM)锻炼、使用短的或不使用外固定器、尽量少的手术暴露。
3.2 ROM减少 Duetzmann等[36]综述2390例患者术后仍有50%的ROM减少,并不优于椎板切除术和融合。Hyun等[37]观察术后颈椎活动,认为ROM的减少与时间有关。Nagamoto等[38]第1次记录了椎管成形术后3D节段性动态改变,尽管6月后C2~C7 ROM屈伸显著降低,但代表颈椎总ROM的 枕骨-T1 ROM 在屈伸、旋转方面未显著降低,认为由枕骨-C2 的节段性运动增加所致部分代偿。他认为其他绝大部分人研究的ROM是侧位片2D的屈伸,而不是精准的3D改变。
Machino等[39]报道了520例椎管成形术后颈椎矢状序列和ROM,矢状序列改变轻微(只增加1.8°的前凸),ROM保留率达87.9%,这与早期移除颈支具、术后颈肌锻炼、一些操作改良有关。Uehara等[40]对13例不稳定性CSM患者的受压节段予以单开门成形术,不稳定节段联合颈椎椎弓根螺钉内固定,不稳定椎最大屈位与最大伸位的滑脱角从术前(9.0±5.5)°(2°~20°) 变化到最后随访的(1.6±1.9)°(0°~5°),滑脱角差异有显著性提高(P=0.043),且无神经血管并发症。因此,术中减少小关节损伤,保护韧带肌肉的附着,减少减压节段,必要时予以脊柱内固定,术后较短的使用支具和较早的功能锻炼,加快神经功能恢复,从而减少ROM的丢失和后凸畸形的发生。
3.3 C5神经根麻痹 表现为三角肌瘫痪、肩部感觉减退,以C5神经根麻痹最为常见。Gu等[41]选择25篇文献的综述认为,单开门、双开门椎管扩大成形术的术后C5麻痹发生率分别为4.5%、3.1%,认为过度的脊髓漂移、术前椎间孔狭窄、OPLL、男性等术后有较高的发生率。Sakaura等[42]总结绝大多数C5麻痹的病理学机制包括术中神经根损伤、神经根牵拉、脊髓缺血、节段性脊髓损伤、脊髓再灌注损伤。Yamanaka等[43]发现椎管成形术联合脊柱融合术术后C5麻痹发生率较高,矫正脊柱后凸和脊柱滑脱使用后路内固定可能是医源性椎间孔狭窄所致C5麻痹的一种危险因素。
Kaneyama等[44]明确证实单开门术后较双开门术后C5麻痹风险高,认为OPLL与单开门一样是C5麻痹的危险因素,单开门造成的不对称减压可能导致脊髓不平衡的旋转运动,建议对OPLL施行双开门。
Katsumi等[45]报道141例单开门伴预防性双侧C4/C5椎间孔减压术,141例只行单开门,术后C5麻痹发生率分别为1.4%(2例)和6.4%(9例)。预防性双侧C4/C5椎间孔减压术显著减少术后C5麻痹,并认为C5麻痹的主要病因是C5神经根损伤,次要病因可能是颈椎管狭窄急性减压所致的脊髓损伤,作者强烈建议单开门术中施行预防性双侧C4/C5椎间孔减压术。Ohashi等[46]证实术中预防性双侧C4/C5椎间孔减压术对术后影像学和临床表现没有负面作用,可有效预防C5麻痹。
以上的所有术式各有优缺点,随着器械、工具更加精密,微创手术理念更加深入、普及,相信术后并发症会更少,在获得相同的疗效同时对患者的创伤更小,术后恢复更快。
[1] Hirabayashi K, Watanabe K, Wakano K, et al. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy[J]. Spine(Phila Pa 1976), 1983, 8(7): 693-699.
[2] Kurokawa T, Tsuyama N, Tanaka H. Enlargement of spinal canal by the sagittal splitting of the spinous process[J]. Bessatsu Seikeigeka, 1982, 2(2): 234-240.
[3] Mitsunaga LK, Klineberg EO, Gupta MC. Laminoplasty techniques for the treatment of multilevel cervical stenosis[J]. Adv Orthop, 2012, 2012:307916.
[4] Ito M, Nagahama K. Laminoplasty for cervical myelopathy[J]. Global spine J, 2012, 2(3): 187-194.
[5] Braly BA, Lunardini D, Cornett C, et al. Operative treatment of cervical myelopathy: cervical laminoplasty[J]. Adv Orthop, 2012, 2012:508534.
[6] Hirabayashi S, Yamada H, Motosuneya T, et al. Comparison of enlargement of the spinal canal after cervical laminoplasty: open-door type and double-door type[J]. Eur Spine J, 2010, 19(10): 1690-1694.
[7] Ding H, Yuan X, Tang Y, et al. Laminoplasty and laminectomy hybrid decompression for the treatment of cervical spondylotic myelopathy with hypertrophic ligamentum flavum: a retrospective Study[J]. PLoS One, 2014, 9(4): e95482.
[8] Arantes Júnior AA, Silva Junior GA, Malheiros JA, et al. A new expansive two-open-doors laminoplasty for multilevel cervical spondylotic myelopathy: technical report and follow-up results[J]. Arq Neuropsiquiatr, 2014, 72(1): 49-54.
[9] Tabaraee E, Mummaneni P, Abdul-Jabbar A, et al. A comparison of implants used in open-door laminoplasty: structural rib allografts versus metallic mini-plates[J]. J Spinal Disord Tech, 2014.
[10]Park YK, Lee DY, Hur JW, et al. Delayed hinge fracture after plate-augmented, cervical open-door laminoplasty and its clinical significance[J]. Spine J, 2014, 14(7): 1205-1213.
[11]Chen H, Liu H, Zou L, et al. Effect of mini-plate fixation on hinge fracture and bony fusion in unilateral open-door cervical expansive laminoplasty[J]. J Spinal Disord Tech, 2014.
[12]Mehdain H, Stokes OM. Cervical laminoplasty[J]. Eur Spine J, 2014, 23 (12): 2759-2762.
[13]Oh CH, Ji GY, Hur JW, et al. Preliminary experiences of the combined midline-splitting french door laminoplasty with polyether ether ketone (peek) plate for cervical spondylosis and OPLL[J]. Korean J Spine, 2015, 12(2): 48-54.
[14]Harshavardhana NS, Dabke HV, Mehdian H. A new fixation technique for french door cervical laminoplasty: Surgical Results With A Minimum Follow-up Of Six Years[J]. J Spinal Disord Tech, 2014.
[15]Park HG, Zhang HY, Lee SH. Box-shape cervical expansive laminoplasty: clinical and radiological outcomes[J]. Korean J Spine, 2014, 11(3): 152-156.
[16]Kim JH, Zhang HY, Park YM. Cervical expansive laminoplasty with 90° box-shape double door method[J]. Korean J Spine, 2012, 9(3): 193-196.
[17]Tani S, Suetsua F, Mizuno J, et al. New titanium spacer for cervical laminoplasty: initial clinical experience.Technical note[J]. Neurol med chir (Tokyo), 2010, 50(12): 1132-1136.
[18]Sakaura H, Hosono N, Mukai Y, et al. C3-6 laminoplasty for cervical spondylotic myelopathy maintains satisfactory long-term surgical outcomes[J]. Global Spine J, 2014, 4(3): 169-174.
[19]Kotani Y, Abumi K, Ito M, et al. Impact of deep extensor muscle-preserving approach on clinical outcome of laminoplasty for cervical spondylotic myelopathy: comparative cohort study[J]. Eur Spine J, 2012, 21(8): 1536-1544.
[20]Shiraishi T, Kato M, Yato Y, et al. New techniques for exposure of posterior cervical spine through intermuscular planes and their surgical application[J]. Spine(Phila Pa 1976), 2012, 37(5): E286-E296.
[21]Umeda M, Sasai K, Kushida T, et al. A less-invasive cervical laminoplasty for spondylotic myelopathy that preserves the semispinalis cervicis muscles and nuchal ligament [J]. J Neurosurgery Spine, 2013, 18(6): 545-552.
[23]Lin S, Zhou F, Sun Y, et al. The severity of operative invasion to the posterior muscular-ligament complex influences cervical sagittal balance after open-door laminoplasty[J]. Eur Spine J, 2015, 24(1): 127-135.
[24]Sinha S, Jagetia A. Bilateral open-door expansive laminoplasty using unilateral posterior midline approach with preservation of posterior supporting elements for management of cervical myelopathy and radiculomyelopathy—analysis of clinical and radiological outcome and surgical technique[J]. Acta Neurochir(Wien), 2011, 153(5): 975-984.
[25]Abdullah KG, Yamashita T, Steinmetz MP, et al. Open-door cervical laminoplasty with preservation of posterior structures[J]. Global Spine J, 2012, 2(1): 15-20.
[26]Jiang L, Chen W, Chen Q, et al. Clinical application of a new plate fixation system in open-door laminoplasty[J]. Orthopedics, 2012, 35(2): e225-e231.
[27]Chen Y, Chen D, Wang X, et al. Significance of segmental instability in cervical ossification of the posterior longitudinal ligament and treated by a posterior hybrid technique[J]. Arch Orthop Trauma Surg, 2013, 133(2): 171-177.
[28]刘永皑,刘永恒,华诚峰. 颈椎椎板成形侧块螺钉内固定术的并发症分析及防治[J]. 中国骨伤, 2013, 26(3): 201-204.
[29]Miyamoto H, Maeno K, Uno K, et al. Outcomes of surgical intervention for cervical spondylotic myelopathy accompanying local kyphosis (comparison between laminoplasty alone and posterior reconstruction surgery using the screw-rod system)[J]. Eur Spine J, 2014, 23(2): 341-346.
[30]Kim K, Isu T, Omura T, et al. Transarticular fixation with a bioabsorptive screw for cervical spondylolisthesis[J]. World Neurosurg, 2014, 81(5/6): 843.e5-9.
[31]Kawaguchi Y, Matsui H, Ishihara H, et al. Axial symptoms after en bloc cervical laminoplasty[J]. J Spinal Disord, 1999, 12(5): 392-395.
[32]Wang SJ, Jiang SD, Jiang LS, et al. Axial pain after posterior cervical spine surgery: a systematic review[J]. Eur Spine J, 2011, 20(2): 185-194.
[33]Sakaura H, Hosono N, Mukai Y, et al. Preservation of muscles attached to the C2 and C7 spinous processes rather than subaxial deep extensors reduces adverse effects after cervical laminoplasty[J]. Spine(Phila Pa 1976), 2010, 35(16):E782-E786.
[34]Mesfin A, Park M S, Piyaskulkaew C, et al. Neck Pain following Laminoplasty[J]. Global Spine J, 2015, 5(1): 17-22.
[35]Wang L, Wei F, Liu S, et al. Can Modified Kurokawa’s Double-Door laminoplasty reduce the incidence of axial symptoms at long-term follow-up?: a prospective study of 152 patients with cervical spondylotic myelopathy[J]. J Spinal Disord Techn, 2015, 28(4):E186-E193.
[36]Duetzmann S, Cole T, Ratliff JK. Cervical laminoplasty developments and trends, 2003-2013: a systematic review[J]. J Neurosurg Spine, 2015, 23(1):24-34.
[37]Hyun SJ, Riew KD, Rhim SC. Range of motion loss after cervical laminoplasty: a prospective study with minimum 5-year follow-up data[J]. Spine J, 2013, 13(4): 384-390.
[38]Nagamoto Y, Iwasaki M, Sugiura T, et al. In vivo 3D kinematic changes in the cervical spine after laminoplasty for cervical spondylotic myelopathy[J]. J Neurosurg Spine, 2014, 21(3): 417-424.
[39]Machino M, Yukawa Y, Hida T, et al. Cervical alignment and range of motion after laminoplasty: radiographical data from more than 500 cases with cervical spondylotic myelopathy and a review of the literature[J]. Spine (Phila Pa 1976), 2012, 37(20): E1243-E1250.
[40]Uehara M, Takahashi J, Ogihara N, et al. Cervical pedicle screw fixation combined with laminoplasty for cervical spondylotic myelopathy with instability[J]. Asian Spine J, 2012, 6(4): 241-248.
[41]Gu Y, Cao P, Gao R, et al. Incidence and risk factors of C5 palsy following posterior cervical decompression: a systematic review[J]. PLoS One,2014,9(8):e101933.
[42]Sakaura H, Hosono N, Mukai Y, et al. C5 palsy after decompression surgery for cervical myelopathy: review of the literature[J]. Spine (Phila Pa 1976), 2003, 28(21): 2447-2451.
[43]Yamanaka K, Tachibana T, Moriyama T, et al. C-5 palsy after cervical laminoplasty with instrumented posterior fusion [J]. J Neurosurg Spine, 2014, 20(1): 1-4.
[44]Kaneyama S, Sumi M, Kanatani T, et al. Prospective study and multivariate analysis of the incidence of C5 palsy after cervical laminoplasty[J]. Spine, 2010, 35(26): E1553-E1558.
[45]Katsumi K, Yamazaki A, Watanabe K, et al. Can prophylactic bilateral C4/C5 foraminotomy prevent postoperative C5 palsy after open-door laminoplasty?: a prospective study[J]. Spine (Phila Pa 1976), 2012, 37(9): 748-754.
[46]Ohashi M, Yamazaki A, Watanabe K, et al. Two-year clinical and radiological outcomes of open-door cervical laminoplasty with prophylactic bilateral C4-C5 foraminotomy in a prospective study[J]. Spine(Phila Pa 1976), 2014, 39(9): 721-727.
100038北京市,北京世纪坛医院脊柱外科
丁立祥,Email:dinglixiang@medmail
R 681.5
A
10.3969/j.issn.1003-9198.2015.11.003
2015-09-24)
——壮肾