Lesson Sixty-six "Classical"response in a pre-excited tachycardia:What are the pathways involved?
●心电学英语
Lesson Sixty-six "Classical"response in a pre-excited tachycardia:What are the pathways involved?
Introduction
A 24-year-old patient presented with history of recurrent palpitation and was diagnosed as wide QRS tachycardia which was cardioverted.The sinus rhythm ECG and the tachycardia ECG are shown in Figure 1. During the electrophysiological study,2 morphologies of tachycardia were inducible,1 with right bundle branch block(RBBB)morphology(Figure 2A)and another with left bundle branch block(LBBB)morphology(Figure 2B),which was her clinical tachycardia.The LBBB type wide QRS tachycardia was faster(Figure 2B).DuringtheRBBBmorphologytachycardia, ventricular entrainment showed a V-A-V response and a His refractory ventricular extrastimulation1advanced the retrograde atrial activation,resetting the tachycardia.
TheLBBBmorphologytachycardiashowed variation in cycle length with a constant Ventriculo-Atrial(VA)interval.Atrial entrainment did not change the QRS morphology or VA relationship.An early premature atrial extrastimulation from the lateral right atrium showed an interesting finding(Figure 3).Very late atrial extrastimulus from the same location did not advance the V without affecting the septal A.What are the mechanisms of the two tachycardias?
Commentary
The baseline ECG showed features typical of an accessory pathway,in the right posterior location.The clinical tachycardia was a regular wide QRS tachycardia(Figure 1B),with LBBB morphology and left axis deviation.The 12-lead ECG of the tachycardia gives certain clues to the underlying pathways.The typical antidromic tachycardia would have resulted in a wider QRS and predominantly positive complexes in the lateral precordial leads because of ventricular activation solely through the accessory pathway.A fast conducting AVN-His bundle may,however,result in relatively narrower QRS.When the tachycardia morphology does not correspond to the pre-excitation pattern in sinus rhythm,multiple pathways should be considered.The wide QRS tachycardia shows left axis deviation and LBBB and has a sharp rapid component of the initial part and has no precordial transition.These features are moretypicalofanatriofascicular(Mahaim)tachycardia,although the sinus rhythm ECG is not typical for a Mahaim fiber.
Intracardiac recording in Figure 2shows an orthodromic tachycardia([ORT]with RBBB aberrancy)with antegrade conduction through the His bundle,and retrograde conduction through a right-sided pathway(Figure 2A);earliest atrial activity was noted in the distal HALO electrodes in the posterolateral tricuspid annulus.An atrial tachycardia with aberrancy was ruled out by a VAV response to ventricular entrainment.A short postpacing interval and atrial pre-excitation2by a Hisrefractoryventricularstimulusconfirmedthe diagnosis.
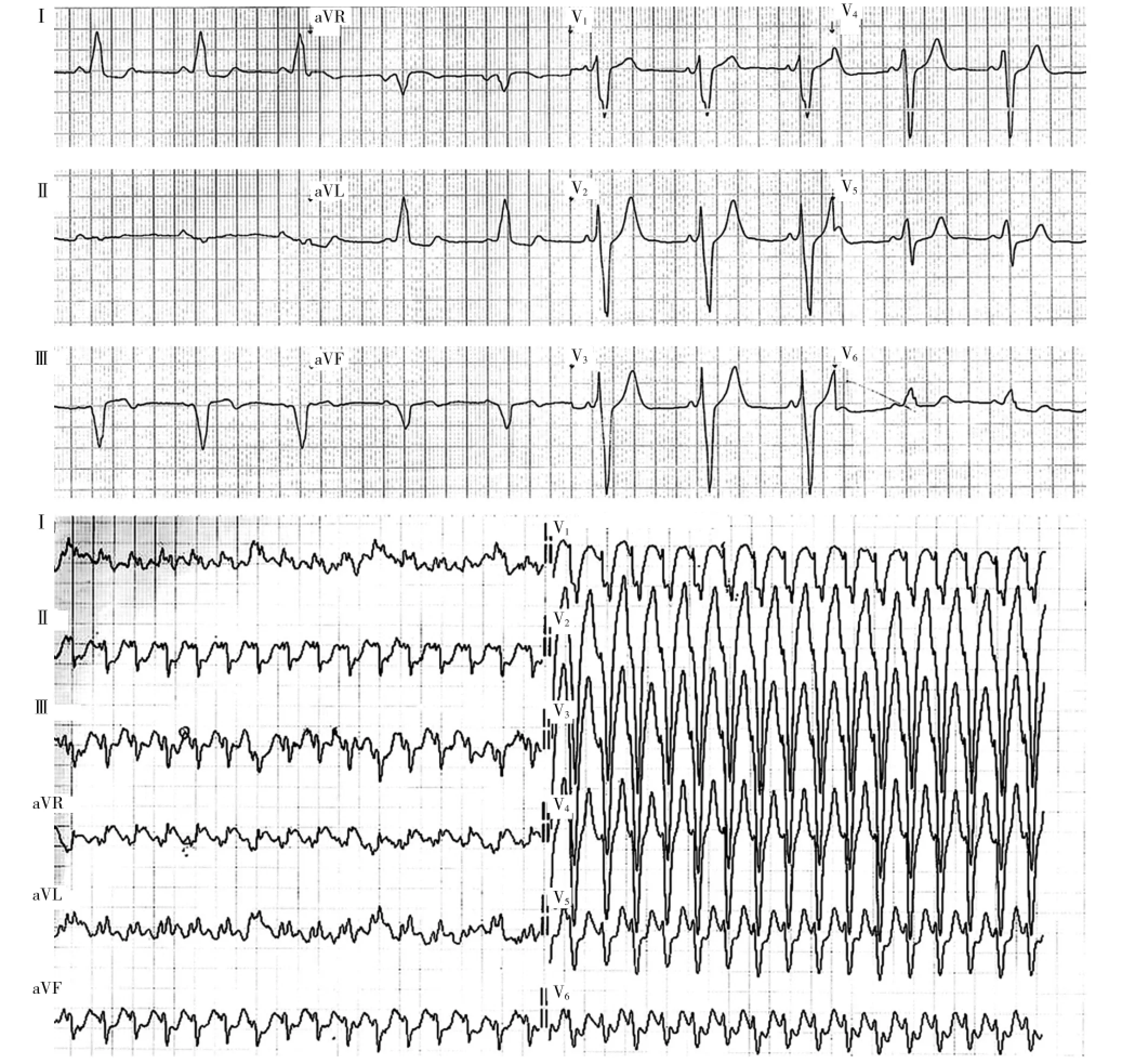
Figure 1Twelve-lead electrocardiograms of the patient in sinus rhythm(A)and during clinical tachycardia(B).
The wide QRS tachycardia with LBBB morphology(Figure 2B)has a shorter cycle length but has the same eccentric retrograde activation sequence.It was initiated by catheter-induced ventricular ectopics during the ORT.The HV was negative(ventricular-His[VH] =80ms)showing that it is a truly pre-excited long VH tachycardia.At this point,it can be assumed that the H is a retrograde H(further confirmed by observations mentioned below).Two additional points should be noted in Figure 2B∶(1)the retrograde activation sequence is same as during the ORT(tachycardia 1)and(2)the cycle length is considerably shorter during the wide QRS LBBB morphology rhythm.These essentially rule out a classic antidromic tachycardia mediated by the same AV connection.However,thepresenceofRBBBor incorporation of the slow pathway during the ORT alone may cause it to be slower than antidromic tachycardia. Orthodromic reentry with aberrancy is ruled out by the negative HV.AVNRT with bystander accessory pathway is excluded because of eccentric atrial activation and because the retrograde activation did not change between the tachycardias.Further,in AVNRT with bystander activation,the VH is usually short and the H recorded is an antegrade H.A late atrial extrastimulus during the tachycardia when the AV junction is refractory can be used to diagnose AVNRT with bystander pathway(see below).A His refractory ventricular stimulus can also exclude AVNRT if it resets the tachycardia with the same activation sequence in atria-this was demonstrated in this case.The possibility then we have to consider is thatthesecondtachycardiaisbecauseofa pathway-to-pathway conduction-antegrade conduction through a right-sided accessory pathway(LBBB,left axis),with a negative VH as noted in the figure and retrogradeconductionthroughthesameright posterolateral pathway mediating the ORT,with earliest atrial activation in HALO 1,2.Pathway-to-pathway tachycardia are usually possible only when the pathways are at a considerable distance anatomically.When 2 pathways are close by,like in this case,tachycardia can be sustained more easily if at least one of the pathways has decremental conduction property.In such a scenario, the AVN can conduct retrogradely and activate part of the atria.The rare possibility of ORT with bystander pathway was previously reported;however,they are associated with minimal QRS widening and a short rather than negative HV.
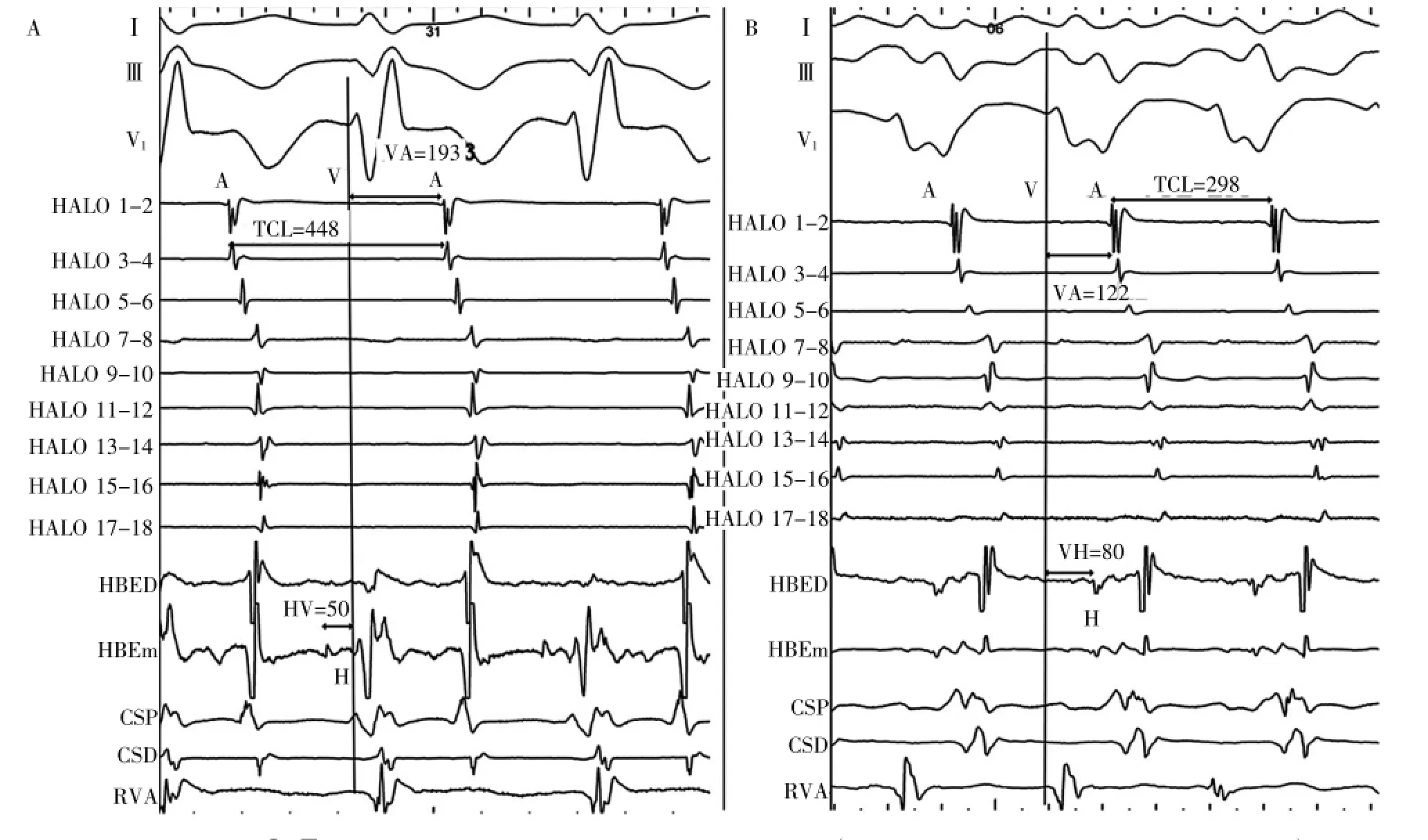
Figure 2Surface leadsⅠ,Ⅲ,and V1and intracardiac electrograms from right atrium(HALO 1,2 at lateral right atrium to HALO 17,18),His bundle(His bundle distal[HBED]and His bundle middle[HBEm]),the coronary sinus(coronary sinus distal[CSD]and coronary sinus proximal [CSP])and right ventricular apex(RVA).A,The orthodromic tachycardia with right bundle branch block aberrancy.B,The left bundle branch block tachycardia of shorter cycle length and long ventricular-His of 80 ms with the same retrograde eccentric atrial activation as in the initial tachycardia.
Atrialentrainmentshowedresettingofthe tachycardia without alteration of the QRS morphology or VH interval,thus confirming atria as necessary part of the circuit and also making AVNRT or ORT with bystanderpathwayunlikely.Iftheatriofascicular pathway was merely a bystander,QRS morphology and the VH relationship would change with resetting of the tachycardia.This also rules out a myocardial VT. Coupled atrial premature stimuli also showed advancing of the V.A relatively early coupled atrial stimulus produced an interesting finding as noted in Figure 3, which shows a coupled atrial extrastimuli during the pre-excited rhythm,which delayed the ventricular activation through the pathway and reset the tachycardia withoutchangingtheVHorVAinterval.This demonstrates the decremental nature of the anterograde pathway during tachycardia.It also demonstrates that the H is a retrograde H related to V.If His bundle activation contributed to activation of septal atrium,this resetting would have been expected to at least slightly alter the atrial activation pattern.Even very late atrial extrastimuli(delivered from the presumed site of antegrade pathway)advanced the septal A making it likely that atrium in the vicinity of the His is activated through the retrograde accessory pathway and there is Hto A block during the LBBB tachycardia.Further,the atrialactivationduringboththeORTandthe pre-excited tachycardia is the same showing that there is no retrograde activation of atrium through the AVN. During cycle length changes in the LBBB tachycardia the VH and VA interval remained constant.Thus,a diagnosis of pathway-to-pathway tachycardia,mediated by a Mahaim fiber and a closely located nondecremental pathway was made.
Patientsubsequentlydevelopedanatrial tachycardia with 2∶1 AV conduction through both accessory AV connection(Figure 4A).Figure 4A shows thecharacteristicMahaimpotentialat9o′clocktricuspid location with a short M to QRS interval.This short M to QRS interval is not typical for Mahaim conduction.It shows that the QRS is also contributed by antegrade conduction through the right posterior nondecremental pathway-a case of pre-excited Mahaim conduction. Successful ablation of the Mahaim fiber resulted in change in QRS morphology.The right posterior pathway was mapped during ORT and successfully ablated at the posterior tricuspid annulus region(Figure 4B).Post ablation of both pathways there was persistent RBBB and no VA conduction at 500 ms showing a poor retrograde conduction through the AV node.
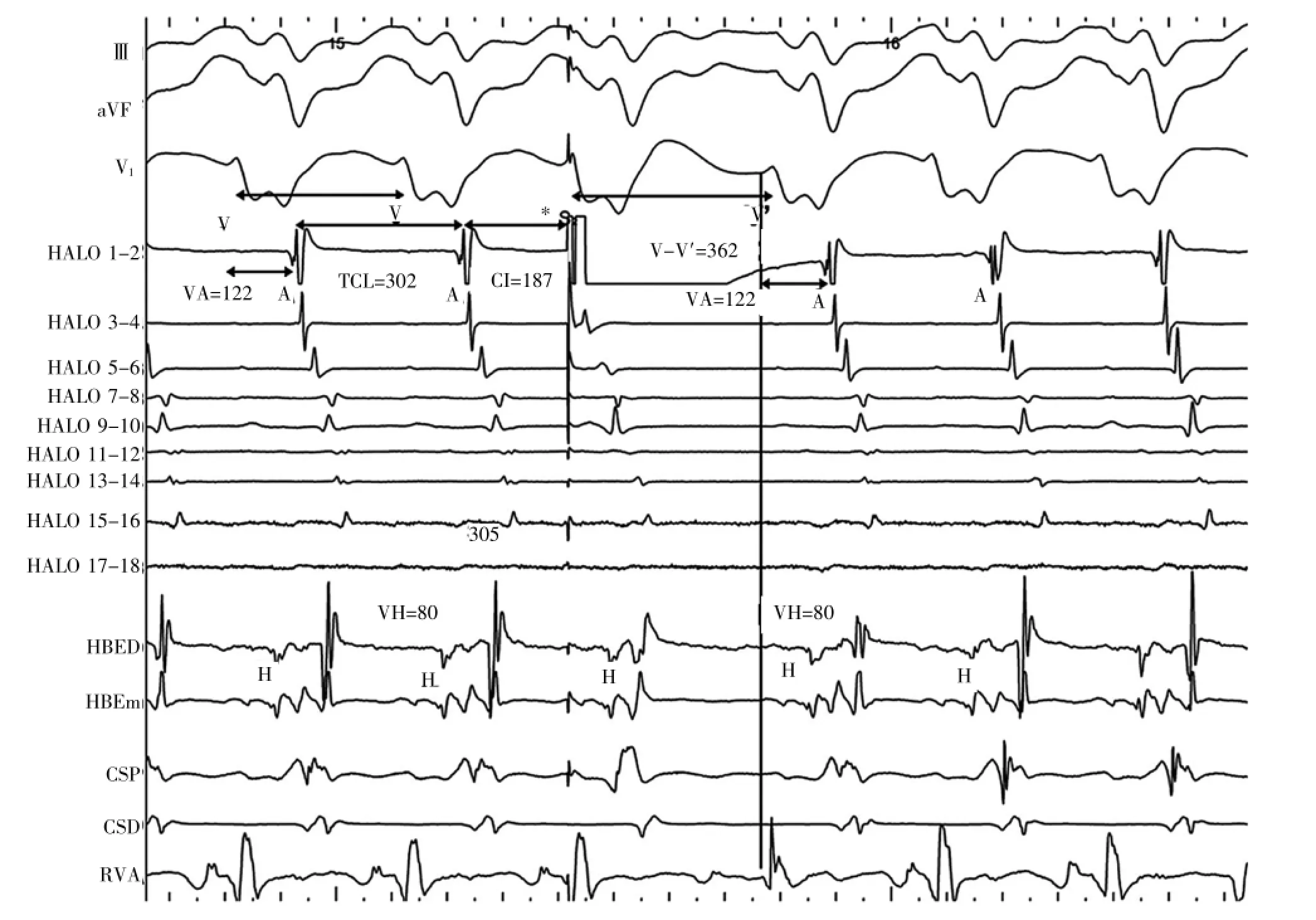
Figure 3Surface leadsⅠ,Ⅲ,and V1and intracardiac electrograms from right atrium,His bundle,the coronary sinus and right ventricular apex.The effect of an early coupled atrial stimulus(asterisk)during tachycardia is shown.CI indicates coupling interval of atrial stimulus;TCL,tachycardia cycle length;and V-V',interval between surface QRS following the extrastimulus.
词汇
aberrancy n.偏离正路,差异
eccentric adj.&n.古怪,古怪的,偏心;偏心轮,偏心圆
incorporation n.包含,公司,混合
anatomically adv.在解剖学上
decremental adj.减少的,递减的
注释
1.His refractory ventricular extrastimulation指“希氏束不应期间的心室期外刺激”,通常在室上性心动过速时,略短于心动过速周长(<40ms)的心室起搏即是。2.atrial pre-excitation指“心房提前激动”或“心房预激”。室上性心动过速时心室起搏,使得心房频率加快,心动周期缩短15ms或以上,即为心房预激。希氏束不应期间心室起搏引起心房预激,要考虑顺传型房室折返性心动过速。

Figure 4Fluoroscopic left anterior oblique projections of location and electrograms from the following catheters∶the duo-decapolar catheter along the tricuspid annulus(HALO 1,2 to 17,18),the decapolar coronary sinus(CS),the mapping and ablation catheter(shown with asterisk.RFd and RFp)and quadripolar catheters in the His(His bundle distal[HBED],His bundle middle[HBEm],and His bundle proximal[HBEp])and right ventricular apex(RVA).A.Atrial tachycardia with 2∶1 conduction and M potentials at the ablation catheter at the site of successful ablation of the Mahaim fiber.Note the short M-Local V interval and simultaneous activation of the RVA and ventricular annulus(RFd)because of antegrade conduction through both pathways.B.The recording during orthodromic tachycardia,ablation at the posterolateral tricuspid annulus results in local separation of VA and termination of tachycardia(solid down arrow).
参考译文
第66课预激心动过速的“经典”反应——涉及哪些旁道?
购买蔬菜、水果时,不买异常气味的蔬菜和水果。有些商贩为了蔬菜更好看,用化学药剂进行浸泡,这些物质有异味,不容易被冲洗掉。不买颜色异常的蔬菜和水果,不买形状异常的蔬菜和水果。有的蔬菜使用了激素物质,会长成畸形。尽量不要食用“新奇”“野味”等不常食用或从未食用过的食物。
患者女性,24岁,因反复心悸而就诊,诊断为宽QRS波群心动过速并得到复律。图1为窦性节律心电图和心动过速心电图。电生理检查中,诱发出两种形态的心动过速,一为右束支传导阻滞(RBBB)图形(图2A),另一为左束支传导阻滞(LBBB)图形(图2B),与她临床发作的心动过速一样。LBBB型宽QRS波群心动过速较快(图2B)。RBBB图形心动过速时,心室拖带显示V-A-V反应,希氏束不应期心室期外刺激使逆传心房激动提前,重整心动过速。
LBBB图形心动过速显示周长变化而室-房(VA)间期恒定。心房拖带不能改变QRS形态或VA关系。右心房外侧壁早期房性期外刺激显示令人感兴趣的发现(图3)。同一部位很晚的心房期外刺激不能提前V而不影响间隔A。这两种心动过速的机制是什么呢?
评析
基础心电图显示旁道特征,位于右后部位。临床心动过速是一规则的宽QRS波群心动过速,呈LBBB图形和心电轴左偏(图1B)。心动过速12导联心电图对所涉径路提供一定线索。典型的逆传型心动过速因完全通过旁道激动心室理应产生较宽的QRS波群,且侧胸导联以正向波为主,而快速传导的房室结-希氏束可产生相对较窄的QRS波群。当心动过速图形与窦性节律时的预激图形不一致时,应考虑多径路。本例宽QRS波群心动过速呈心电轴左偏和LBBB,起始部分尖锐急速,且无胸前移行。这些是房-束(Mahaim)心动过速较为典型的特征,尽管窦性节律心电图不典型。
图2心内记录显示顺传型心动过速[(ORT)伴RBBB差异],经希氏束顺传和右侧旁道逆传(图2A);最早心房激动见于三尖瓣环后外侧HALO电极的远端。心室拖带呈V-A-V反应排除了房性心动过速伴差异。起搏后短间期和希氏束不应期心室刺激时心房预激证实这一诊断。
LBBB图形的宽QRS波群心动过速(图2B)周长较短,但有相同的偏心性逆传激动顺序,系ORT时导管刺激的心室异位激动所引发。HV是负向的[心室-希氏束(VH)=80ms],表明这确实是预激长VH心动过速。就这一点,可以推测H是逆行H。图2B上另外两点值得注意∶(1)逆行激动顺序与ORT(心动过速1)时相同,(2)宽QRS波群LBBB图形节律时心动周长较短。这些基本排除了由同一AV连接介导的典型逆传型心动过速。然而,ORT时单一RBBB或合并慢径路传导即可使其慢于逆传型心动过速。负向HV排除了顺传型折返伴差异。因为心房激动呈偏心性及两种心动过速之间逆传激动并无变化,可排除AVNRT合并旁观旁道。此外,AVNRT伴旁观旁道激动时,通常VH短且H是顺传H。心动过速房室交界不应期时晚期房性期外刺激可用于AVNRT合并旁观旁道的诊断。希氏束不应期室性刺激如能重整心动过速而心房激动顺序不变也可排除AVNRT,这在本例得以证实。我们必须考虑的可能情况是第二种心动过速属于旁道-旁道传导,即经右侧旁道顺传(LBBB,心电轴左偏),伴有图示的负向VH,经介导ORT相同的右后外侧旁道逆传,最早激动位于HALO电极1-2。通常,只有当两条旁道解剖上有相当距离时,旁道-旁道心动过速才有可能。两条旁道靠近时,如本病例,只在至少其中一条旁道具有递减传导特性时,心动过速才较易维持。在此情况下,AVN能逆传并激动部分心房。以前报道过ORT伴旁观旁道可能性极小,伴随QRS波群轻微增宽、短HV而非负向HV。
心房拖带显示重整心动过速而不改变QRS形态或VH间期,证实心房是折返环的必需部分,不可能是AVNRT或ORT伴旁观旁道。如果房-束旁道只是旁观者,那么,随着心动过速的重整,QRS形态和VH的相互关系应发生改变。这也排除心肌VT。偶联房性期前刺激显示同样提前V波。较早的偶联房性刺激产生令人感兴趣的发现,图3所示预激心律时的偶联心房期外刺激,通过旁路推迟了心室激动,重整心动过速而不改变VH或VA间期。这证实心动过速时前向旁道的递减特性。也证实相对于V,H是逆行H。如果希氏束激动促进间隔心房的激动,那么,这一重整至少会轻微改变心房激动的形式。鉴于很晚的心房期外激动(来自认定的前向旁道部位)提前间隔A,使得毗邻希氏束的心房由逆行旁道激动成为可能,而LBBB心动过速时H到A受阻。此外,ORT和预激心动过速时心房激动相同,均未见经AVN逆传的心房激动。LBBB心动过速周长变化时,VH和VA保持恒定。这样,可诊断为由Mahaim纤维和紧邻其的非递减性旁道介导的旁道-旁道心动过速。
随后,患者发生经两条AV旁道2∶1 AV传导的房性心动过速(图4A)。图4A显示三尖瓣环9点处特征性Mahaim电位,M-QRS间期短。M与QRS间期短并非Mahaim传导的特征。这表明经右后非递减传导旁道的顺传也参与QRS波群的形成,是一种预激的Mahaim传导。成功消融Mahaim纤维引起QRS形态变化。ORT期间标测到右后旁道并于三尖瓣环后区成功消融(图4B)。两条径路消融后为持续性RBBB,500ms起搏无VA传导,表明AV结逆传不良。
图2体表Ⅰ、Ⅱ、Ⅲ,右心房(从右房外侧壁HALO1,2到HALO17,18),希氏束[远端(HBED)和中段(EBEM)],冠状窦远端[(CSD)和近端(CSP)]及右心室尖(RVA)腔内电图。A.顺向型心动过速伴右束支传导阻滞差异;B.周长较短和心室-希氏束间期80ms长的左束支传导阻滞心动过速,逆行偏心性心房激动与前一心动过速相同。
图3体表Ⅰ、Ⅲ和V1,右心房,希氏束,冠状窦和右心室心尖腔内电图。心动过速时早期偶联房性刺激(星标)的效应。CI:房性刺激偶联间期,TCL:心动过速周长,V-V′:期外刺激与其后体表QRS波群之间的间期。
图4左前斜位透视定位及随后的导管记录电图:沿三尖瓣环的双十极导管(HALO 1,2 to 17,18),十极冠状窦导管(CS),标测和消融导管(星标,RFd和RFp),希氏束四极导管(远端:HBED,中段:HBEm和近端:HBEp),右心室心尖四极导管。A.房性心动过速2∶1传导,Mahaim纤维成功消融部位消融导管记录到M电位。因经两条径路顺传,可见M-局部V间期短,RVA和心室环部(RFd)同时激动。B.顺传型心动过速记录,三尖瓣环后外侧消融导致局部VA分离和心动过速中止(向下实线箭头)。
[1]Thajudeen A,Namboodiri N,Choudhary D,et al."Classical" response in a pre-excited tachycardia∶What are the pathways involved[J]?Circ Arrhythm Electrophysiol,2013,6∶e11-e16.
(童鸿)