老年人原发性胆汁反流性胃炎病理特征分析
季红莉,王 清,付万发,张 翼,陈 明,黄 慧
老年人原发性胆汁反流性胃炎病理特征分析
季红莉1*,王 清2,付万发1,张 翼1,陈 明1,黄 慧1
(北京老年医院:1消化科,2病理科,北京 100095)
探讨原发性胆汁反流对老年人胃黏膜组织损伤的病理特点。回顾性地分析2013年1月~2014年8月于我院经胃镜检查诊断的77例老年原发性胆汁反流性胃炎(BRG)患者为观察组,同时取同期诊断为幽门螺杆菌(Hp)感染的非BRG慢性胃炎的78名老年患者为对照组,分析两组患者胃黏膜组织的病理变化特点。原发性BRG患者Hp感染率为19.5%。胆汁反流组与Hp感染的非BRG慢性胃炎病理组织特征比较:轻、中、重慢性炎分别为32.5%11.5%、58.4%34.6%和9.1%53.8%,中性粒细胞浸润分级(无、轻、中、重)分别为83.1%41.0%、11.7%20.5%、5.2%32.1%和0.0%6.4%。淋巴滤泡、肠上皮化生和胃黏膜萎缩检出率分别为4.3%26.9%、5.2%17.9%和6.5%25.6%;胆汁反流组中,Hp阳性和Hp阴性患者轻、中、重度慢性炎分别为:13.3%37.1%、53.3%59.7%和33.3%3.2%,中性粒细胞浸润分级(无、轻、中、重)分别为53.3%41%、20.0%9.7%、20.0%0.0%和6.7%0.0%,淋巴滤泡、肠上皮化生和胃黏膜萎缩检出率分别为53.3%4.8%、0.0%6.5%和0.0%8.1%。原发性胆汁反流可引起老年患者胃黏膜组织慢性炎症反应、肠上皮化生、腺体萎缩,但其发生率低于Hp感染的慢性胃炎。中性粒细胞浸润和淋巴滤泡形成主要与Hp感染相关,Hp感染并未增加原发性胆汁反流患者胃黏膜萎缩、肠化生不良结局的发生。
原发性胆汁反流性胃炎;老年人;病理学;内镜检查
十二指肠胃反流是机体存在的一种生理现象,过多的十二指肠胃反流可致胃黏膜损伤,称为胆汁反流性胃炎(bile reflux gastritis,BRG),它是消化系统常见病,约占胃炎总数的12.3%[1]~16.4%[2]。发生于非手术胃的BRG,称为原发性BRG;而发生于胃幽门手术后过多胆汁反流引起的胃炎,称为继发性BRG,继发性BRG可导致胃黏膜肠化、萎缩和不典型增生等病理改变[3]。而老年原发性BRG是否具有相同的病理特点?与幽门螺杆菌(,Hp)感染的慢性胃炎相比又有何特点?本研究选择经内镜诊断的老年原发性BRG患者进行组织病理学分析,以了解老年原发性BRG的病理特征。
1 对象与方法
1.1 研究对象
所有病例均为2013年1月~2014年8月因上腹部症状于北京老年医院进行胃镜检查的≥60岁的老年人,观察组为原发性BRG患者,共77人,男性23人,女性54人,年龄(64.1±4.9)岁;对照组Hp感染的非BRG的慢性胃炎患者,共78人,男性41人,女性37人,年龄(68.4±6.8)岁,两组患者均无胃肠道手术史。
1.2 方法
1.2.1 胃镜检查 去除继发于手术后胃的病例,符合将“内镜下见到黏液湖胆染和胃窦黏膜糜烂(或中度以上充血)并存者诊断为BRG”作为原发性BRG的内镜诊断标准[4]。(1)胃黏膜尤其是胃窦部黏膜充血、水肿或脆性增加;(2)胃黏液湖为黄色或绿色胆汁染色;(3)胃黏膜有胆汁附着或染色;(4)无胃肠道手术史。
1.2.2 胃黏膜病理检查 胃镜检查时,取距幽门2~3cm胃窦大小弯各一块组织,进行苏木精−伊红(hematoxylin-eosin,HE)染色。按2012年《中国慢性胃炎共识意见》[5],观察慢性炎症(轻、中、重)、中性粒细胞浸润(无、轻、中、重);淋巴滤泡(有、无);肠化(有、无);萎缩(有、无)等形态学特征。
1.2.3 幽门螺杆菌感染诊断标准 (1)病理组织学检查,病理切片为亚甲蓝−硼酸染色阳性为Hp阳性诊断标准;(2)C13呼气试验检测,参考值为0~3.9,>3.9为阳性。以上两种方法任何1种为阳性,即诊断为Hp感染。
1.3 统计学处理
2 结 果
77例老年原发性BRG患者中,15例患者合并Hp感染,感染率为19.5%。
比较观察组和对照组病理组织形态学特征,观察组以轻中度慢性炎症为主,淋巴滤泡形成、腺体萎缩和肠上皮化生发生率低于Hp感染患者(表1)。两组患者相比,观察组中性粒细胞浸润即急性炎症反应发生率低,且以轻度急性炎症反应为主(表2)。BRG患者中,Hp阳性与Hp阴性组织病理学特点比较见表3。BRG患者中,Hp阳性与Hp阴性中性粒细胞浸润情况比较见4。
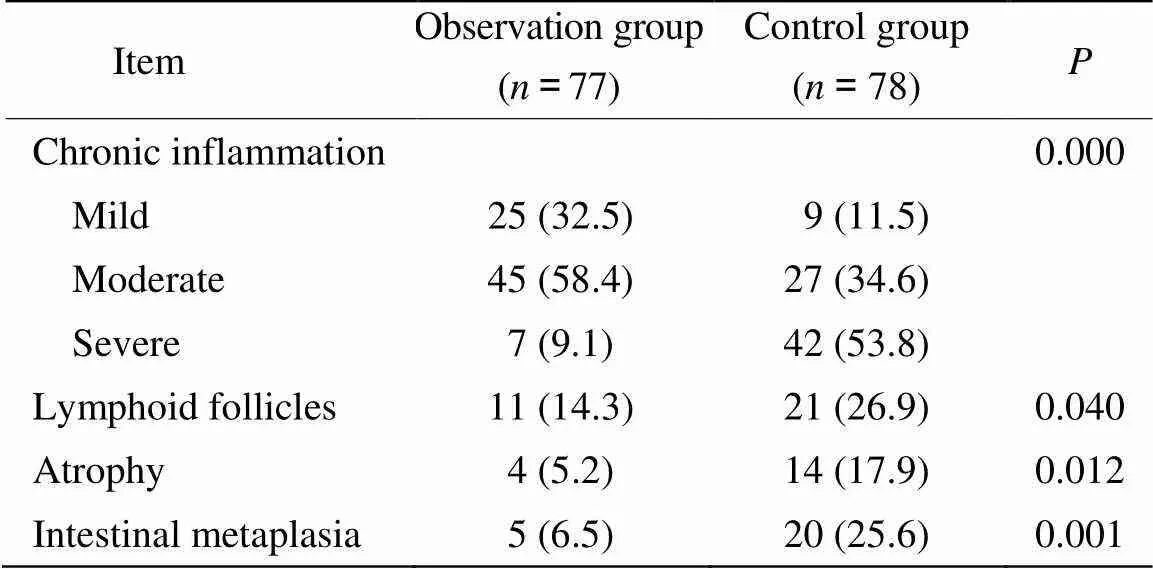
表1 观察组和对照组组织病理学特点比较
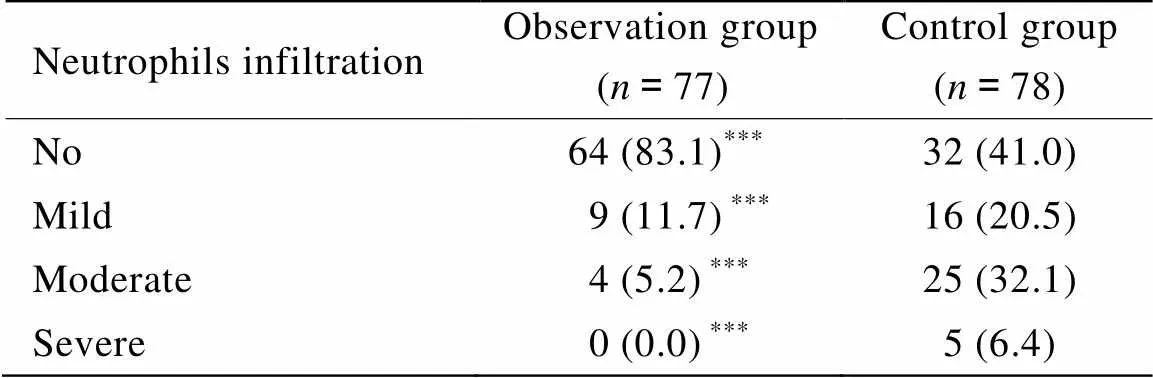
表2 观察组和对照组中性粒细胞浸润情况比较
Compared with control group,***<0.001
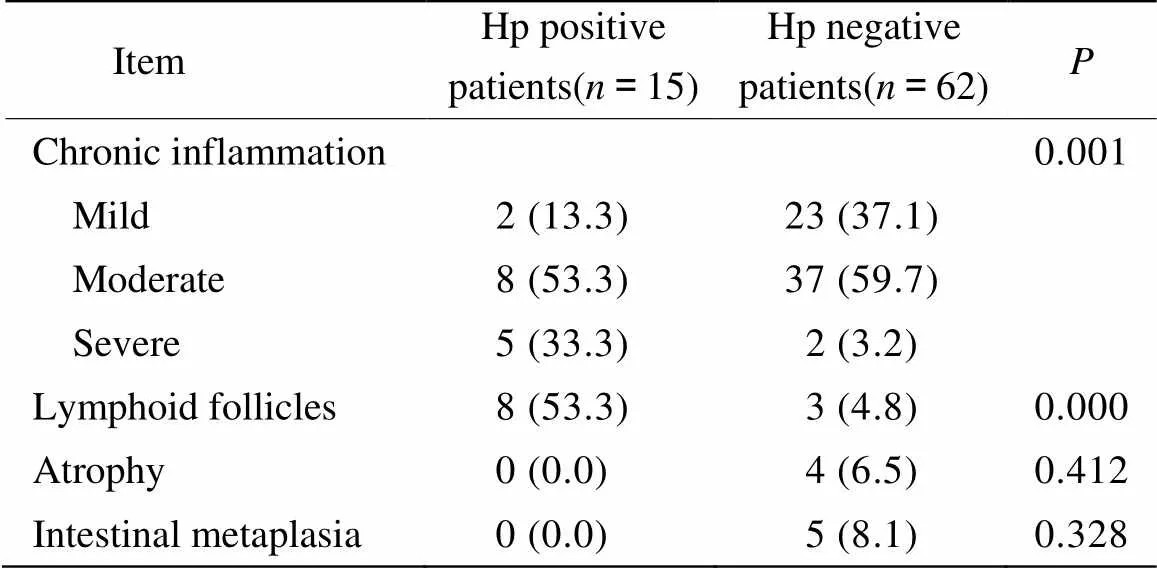
表3 原发性BRG患者Hp阳性与Hp阴性者组织病理学特点比较
BRG: bile reflux gastritis; Hp:
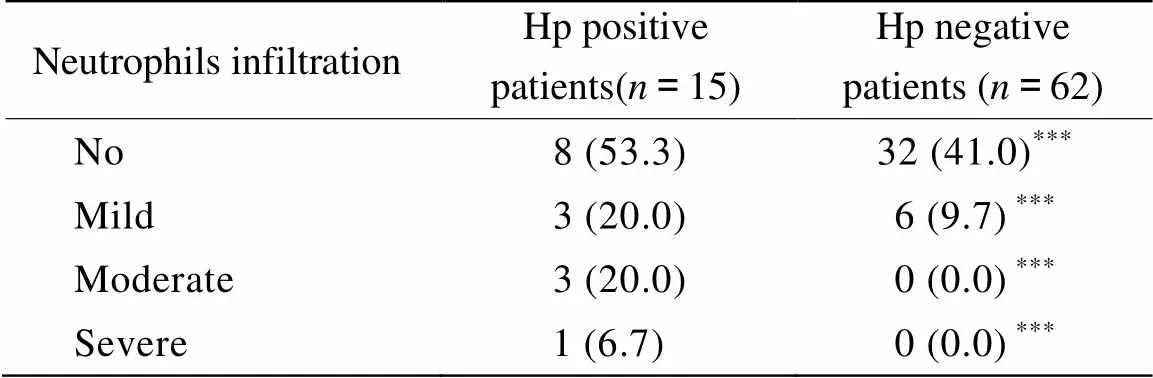
表4 原发性BRG患者Hp阳性与Hp阴性患者中性粒细胞浸润情况
BRG: bile reflux gastritis; Hp:. Compared with Hp positive patients,***<0.001
3 讨 论
发生于非手术胃的BRG,称为原发性BRG。由于其临床表现、胃镜所见及病理组织学缺乏特异性和量化指标,目前较为准确、可行的诊断技术有核素检查和24h胃内胆汁浓度监测,但由于可操作性及费用等问题,尚未在临床广泛使用。内镜检查仍是诊断BRG的主要方法[6],既可观察胃黏膜病变情况,又可通过活检了解组织学变化。因此本文采用内镜检查方法,排除手术胃的继发性BRG,对原发性BRG进行研究。
BRG可与Hp感染共存,Hp感染是否在BRG中起致病作用,目前尚无统一说法。本研究中,BRG病例Hp感染率较低,为19.5%,明显低于全球人群Hp感染率50%[7],考虑与胆汁破坏了胃内Hp生存的酸性环境、胆汁酸抑制了Hp的生长或胆汁直接杀灭Hp有关[8]。除Hp感染外,胆汁反流也是慢性胃炎胃黏膜损伤的重要病因之一[9]。胆汁反流与Hp感染对胃黏膜具有不同的损伤机制,胆汁对胃黏膜的直接损害是BRG发病的主要环节[10],组织病理学特征为小凹增生明显但黏膜炎症不明显的化学性胃病。本研究中,胆汁反流组慢性炎症反应以轻中度反应为主,与陈维顺等[11]研究一致。而淋巴滤泡形成、中性粒细胞浸润,胆汁反流组明显低于Hp感染组,提示淋巴滤泡和炎症的活动性主要与Hp感染相关,胆汁反流与胃黏膜慢性活动性炎症细胞浸润无关[12]。
慢性胃炎均可发生胃黏膜萎缩、肠上皮化生以及不典型增生甚至癌变等不良结局,其发生与致炎因子的性质、作用时间有关。有研究认为,Hp感染和胆汁反流对胃黏膜损伤具有协同作用[13],Hp感染的BRG胃黏膜炎症程度更为严重。本研究中,Hp感染的BRG患者炎症反应虽较Hp阴性的BRG患者更重,但两者之间腺体萎缩和肠上皮化生的发生率比较,差异并无统计学意义,BRG可导致胃黏膜萎缩和肠上皮化生的发生,但Hp感染并未加重BRG的不良反应。
总之,胆汁反流和Hp感染是导致胃黏膜损伤的独立因素,胆汁反流对胃黏膜的损伤轻于Hp感染对胃黏膜的损伤,胆汁反流和Hp感染均可导致胃黏膜萎缩、肠上皮化生[14,15],但未发现Hp感染可加重BRG患者胃黏膜萎缩和肠上皮化生等不良结局的发生。
[1] Ye P, Li ZS, Xu GM,. Efficacy of home made hydrotalcite in treating bile reflux gastritis and 24-hour intragastric bile monitoring[J]. Chin J Dig, 2004, 24(5): 263−265. [叶 萍, 李兆申, 许国铭, 等. 国产铝碳酸镁治疗胆汁反流性胃炎和24小时胆汁监测[J]. 中华消化杂志, 2004, 24(5): 263−265.]
[2] Gastrointestinal Motility Group, Digestive Disease Society, Chinese Medical Association. A multicenter study on dyspepsia symptoms, gastric motor function, and related factors in patients with chronic gastritis[J]. Chin J Dig, 2006, 26(9): 602−605. [中华医学会消化病学分会胃肠动力组. 慢性胃炎患者消化不良症状、胃动力功能与有关因素的多中心调研[J]. 中华消化杂志, 2006, 26(9): 602−605.]
[3] Hu XJ, Dong LH, Ge JR,. Clinical pathology of primary bile reflux gastritis[J]. Chin J Dig Endosc, 2006, 23(3): 215−217. [胡学建, 董来华, 葛建荣, 等. 原发性胆汁反流性胃炎的临床病理分析[J]. 中华消化内镜杂志, 2006, 23(3): 215−217.]
[4] Lin JK, Hu PJ, Li CJ,. A study of diagnosis of primary biliary reflux gastritis[J]. Chin J Intern Med, 2003, 42(2): 81−83. [林金坤, 胡品津, 李初俊, 等. 原发性胆汁反流性胃炎诊断的探讨[J]. 中华内科杂志, 2003, 42(2): 81−83.]
[5] Digestive Disease Society of Chinese Medical Association. China Chronic Gastritis Consensus Opinion (2012, Shanghai)[J]. Chin J Dig, 2013, 33(1): 5−16. [中华医学会消化病学分会. 中国慢性胃炎共识意见(2012年, 上海)[J]. 中华消化杂志, 2013, 33(1): 5−16.]
[6] Wang J, Gu W, Ge XY,. Correlation analysis of total bile acid concentration with pathology and endoscopic classification in bile reflux gastritis[J]. Chin J Dig, 2012, 32(7): 473−475. [王 吉, 顾 玮, 葛心怡, 等. 胆汁反流性胃炎胃液总胆汁酸浓度与病理及内镜分级的相关性分析[J]. 中华消化杂志, 2012, 32(7): 473−475.]
[7] World Gastroenterology Organization Practice Guideline:in developing countries[J]. Chin J Gastroenterol, 2011, 16(7): 423−428. [世界胃肠病学组织全球指南−发展中国家幽门螺杆菌感染[J]. 胃肠病学, 2011, 16(7): 423−428.]
[8] Chen SL, Mo JZ, Cao ZJ,. Influences of bile reflux on profile of gastric mucosal lesions in chronic gastritis[J]. Acad J Shanghai Sec Med Univ, 2005, 25(2): 167−170. [陈胜良, 莫剑忠, 曹芝君, 等. 胆汁返流对慢性胃炎胃黏膜病变的影响[J]. 上海第二医科大学学报, 2005, 25(2): 167−170.]
[9] Yao P, Guo XG. Relationship between duodenogastric reflux and pathology of gastric mucosa[J]. China J Endosc, 2011, 17(4): 354−357. [姚 萍, 郭学刚. 内镜下胆汁反流与胃黏膜损害关系探讨[J]. 中国内镜杂志, 2011, 17(4): 354−357.]
[10] Wei Y, Ding SG. Advances in study on bile reflux gastritis[J]. Chin J Gastroenterol, 2014, 19(5): 305−308. [魏 颖, 丁士刚. 胆汁反流性胃炎研究进展[J]. 胃肠病学, 2014, 19(5): 305−308.]
[11] Chen WS, Luo HY, Zhu YR,. Pathological features of primary bile reflux gastritis in adolescents: an analysis of 40 cases[J]. World Chin J Dig, 2009, 17(23): 2417−2420. [陈维顺, 罗虹雨, 朱宜人, 等. 青年人原发性胆汁反流性胃炎病理特征分析40例[J]. 世界华人消化杂志, 2009, 17(23): 2417−2420.]
[12] Chen TS, Li AF, Chang FY. Gastric reddish streaks in the intact stomach: endoscopic feature of reactive gastropathy[J]. Pathol Int, 2010, 60(4): 298−304.
[13] Guo WQ, Yao P. The pathogenesis and related factors of primary bile reflux gastritis[J]. Chin Gen Pract, 2009, 12(6): 511−513. [郭伟强, 姚 萍. 原发性胆汁反流性胃炎的发病机制及相关因素[J]. 中国全科医学, 2009, 12(6): 511−513.]
[14] Ding H, Chen SL, Li J,. Correlation of total bile acid in gastric juice andinfection with gastric intestinal metaplasia[J]. Chin J Gastroenterol, 2013, 18(1): 11−15. [丁 慧, 陈胜良, 李 吉, 等. 胃液总胆汁酸和幽门螺杆菌感染与胃黏膜肠化生的相关性研究[J]. 胃肠病学, 2013, 18(1): 11−15]
[15] Wu BZ. Relationship between bile reflux gastritis and Hp infection[J]. China Foreign Med Treat, 31(30): 18−19. [吴炳卓. 胆汁反流性胃炎与HP感染的关系探讨[J]. 中外医疗, 2012, 31(30): 18−19.]
(编辑: 李菁竹)
Pathological features of primary bile reflux gastritis in the elderly
JI Hong-Li1*, WANG Qing2, FU Wan-Fa1, ZHANG Yi1, CHEN Ming1, HUANG Hui1
(1Department of Gastroenterology,2Department of Pathology, Beijing Geriatric Hospital, Beijing 100095, China)
To investigate the pathological features of primary bile reflux gastritis (BRG) in the elderly.Clinical data of 77 elderly patients with primary BRG diagnosed by endoscopy (observation group) and another 78 elderly patients suffering from chronic gastritis by(Hp) infection but not with bile reflux (control group) admitted in our hospital from January 2013 to August 2014 were collected and retrospectively analyzed. The pathological changes in the gastric mucosa tissue were observed and compared between the 2 groups.The Hp infection rate was 19.5% in the primary BRG patients. The rates of mild, moderate and severe gastritis were 32.5%11.5%, 58.4%34.6% and 9.1%53.8% in the observation group and the control groups respectively. Neutrophils infiltrating classification (no, mild, moderate and severe) were 83.1%41.0%, 11.7%20.5%, 5.2%32.1% and 0.0%6.4% respectively for the 2 groups. The detection rates of lymphoid follicles, intestinal metaplasia and gastric mucosal atrophy were 4.3%26.9%, 5.2%17.9% and 6.5%25.6%, respectively between them. What’s more, between the Hp-positive and Hp-negative patients from the observation group, the ratios of mild, moderate and severe inflammation were 13.3%37.1%, 53.3%59.7% and 33.3%3.2% respectively, the ratios of no, mild, moderate and severe infiltration of neutrophils were 53.3%41.0%, 20.0%9.7%, 20.0%0.0% and 6.7%0.0%, respectively, and the rates of lymphoid follicles, intestinal metaplasia and gastric grand atrophy were 53.3%4.8%, 0.0%6.5% and 0.0%8.1%, respectively.Primary bile reflux results in chronic inflammation in gastric mucosa, intestinal metaplasia, and gland atrophy in the elderly patients. But the incidence of BRG is lower than that of chronic gastritis due to Hp infection. Neutrophils infiltration and lymph follicles formation are mainly associated with Hp infection. However, for the patients with primary BRG, Hp infection does not increase the risks of mucosal atrophy and intestinal metaplasia.
primary bile reflux gastritis; aged; pathology; endoscopy
R573.3; R592
A
10.11915/j.issn.1671−5403.2015.01.014
2014−10−19;
2014−11−26
季红莉, E-mail: dragon918@163.com

