脑血管病患者介入诊疗与心电图异常的临床研究
卢振产,沈 双,张 冰,俞子恒,程震峰
·临床诊疗提示·
脑血管病患者介入诊疗与心电图异常的临床研究
卢振产,沈 双,张 冰,俞子恒,程震峰
目的 探讨介入诊疗对脑血管病患者心电图异常改变的影响。方法 选取2011年1月—2014年2月湖州市中心医院神经内科住院行介入诊疗的脑血管病患者635例,根据脑血管病类型分为缺血性脑血管病组481例,出血性脑血管病组154例,于介入诊疗操作前、后进行心电图检查,并结合年龄、脑血管病类型等进行分析。结果 635例患者中发现明确心电图异常403例,异常率为63.5%。<45岁患者发现心电图异常13例(14.6%),45~60岁患者发现心电图异常80例(38.1%),>60岁患者发现心电图异常310例(92.3%),不同年龄段患者心电图异常率比较,差异有统计学意义(χ2=5.52,P<0.01)。缺血性脑血管病组患者发现心电图异常362例(75.3%),出血性脑血管病组患者发现心电图异常41例(26.6%),差异有统计学意义(χ2=119.00,P<0.01)。介入诊疗操作前、后,缺血性脑血管病组患者心电图异常率均高于出血性脑血管病组(P<0.05)。缺血性脑血管病组患者介入诊疗操作后心电图异常率与介入诊疗操作前比较,差异无统计学意义(P>0.05);出血性脑血管病组患者介入诊疗操作后心电图异常率高于介入诊疗操作前(P<0.05)。结论 介入诊疗与脑血管病患者的心电图异常有关,完善心电图检查,能够及时了解脑血管病患者接受介入诊疗操作过程中的心脏风险。
脑血管障碍;心电描记术;诊断;治疗
卢振产,沈双,张冰,等.脑血管病患者介入诊疗与心电图异常的临床研究[J].中国全科医学,2015,18(24):2957-2960.[www.chinagp.net]
Lu ZC,Shen S,Zhang B,et al.Clinical study of abnormal changes in electrocardiograph after interventional diagnosis and treatment of patients with cerebrovascular disease[J].Chinese General Practice,2015,18(24):2957-2960.
随着脑血管(包括颈动脉系统)介入诊疗手段的不断改进、成熟,脑血管介入诊疗技术在各级医院的神经内、外科广泛开展,脑血管介入诊疗目前已成为神经内、外科临床常见血管疾病〔如:颅内动脉瘤、脑血管动静脉畸形和颅内外血管狭窄(包括脑底异常血管网病)〕的重要诊断及治疗方法,临床应用日渐普遍[1-3]。目前,针对脑血管病介入诊疗引起心电图异常的报道较少,现对本院3年来635例行脑血管病介入诊疗的脑血管病患者的心电图异常情况分析,以降低神经科脑血管介入诊疗操作引起的心脏相关危险。
1 资料与方法

1.2 介入诊疗 术前准备:向患者及家属介绍手术的方法、经过、相关并发症的风险、注意事项及解决方案,做好相关术前准备(如备皮、导尿等),术前予以0.1 g苯巴比妥肌肉注射缓解患者的紧张恐惧心理。术中操作:患者取平卧位,常规脑血管造影检查,局部麻醉满意后,采用Seldinger技术穿刺右侧股动脉,置入合适导管鞘,进行数字减影血管造影术(DSA)检查,将微导管配合微导丝输送至各个颅内、外动脉,经造影获得清晰全脑血管影像后即结束。需进行血管内介入治疗的患者,予以全身麻醉后,再次经造影确认病变部位及评估后,颈动脉狭窄或动脉夹层患者经微导丝置入相应的支架,蛛网膜下腔出血合并动脉瘤患者经微导丝置入电解脱弹簧圈(膨胀弹簧圈或纤毛弹簧圈),必要时植入相应的支架。术后处理:严密观察生命体征及病情变化,术后患者绝对卧床休息,对患者进行持续心电监护,严密监测患者的心率、血压变化,检测有无头痛、恶心、呕吐、痫样发作、脑水肿加重征象或颈动脉窦受压后出现头昏、血压降低、心率下降等颅内灌注不足症状和体征。
1.3 心电图检查 患者入院后(介入诊疗操作前)及介入诊疗操作后立即采用标准12导联心电图机进行心电图检查,介入诊疗操作后常规床边心电监护至少24 h。因同一例患者心电图可有多种改变,每分析1张心电图及改变类型均按1次人数计算。心电图异常表现包括:房性期前收缩、阵发性心房颤动、窦性心动过速、窦性心动过缓、房室传导阻滞、束支传导阻滞、室性期前收缩、QT间期延长、ST-T段改变、其他(如:窦性心律不齐、左心室肥厚),左心室高电压等未列入异常考察范围。

2 结果
2.1 心电图异常率 635例患者中发现心电图异常403例,异常率为63.5%。<45岁患者发现心电图异常13例(14.6%),45~60岁患者发现心电图异常80例(38.1%),>60岁患者发现心电图异常310例(92.3%),不同年龄段患者心电图异常率比较,差异有统计学意义(χ2=5.52,P<0.01)。缺血性脑血管病组与出血性脑血管病组患者房性期前收缩、窦性心动过速、房室传导阻滞、室性期前收缩发生率比较,差异均无统计学意义(P≥0.05);两组阵发性心房颤动、窦性心动过缓、束支传导阻滞、QT间期延长、ST-T段改变发生率及心电图异常率比较,差异均有统计学意义(P<0.05,见表1)。
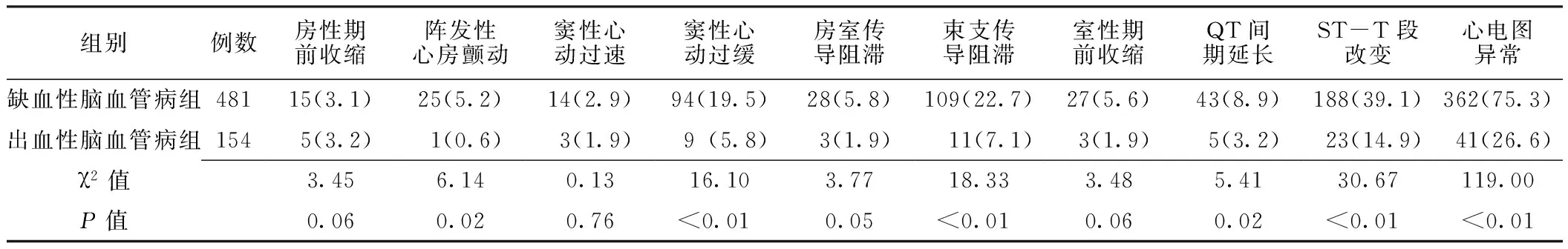
表1 缺血性脑血管病组和出血性脑血管病组患者心电图异常率比较〔n(%)〕
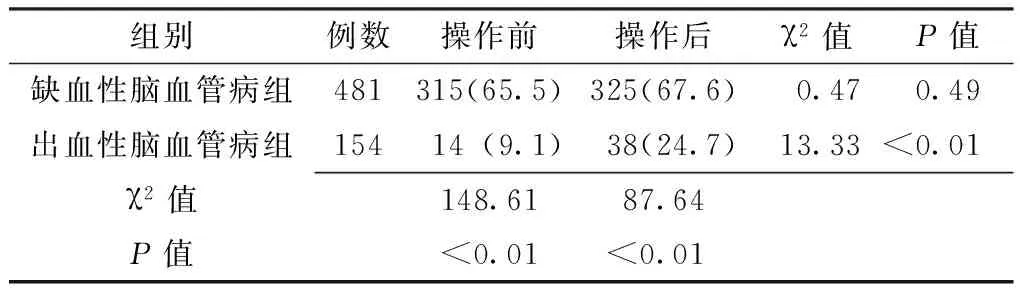
2.2 两组患者介入诊疗操作前后心电图异常率 介入诊疗操作前、后,缺血性脑血管病组患者心电图异常率均高于出血性脑血管病组,差异有统计学意义(P<0.05)。缺血性脑血管病组患者介入诊疗操作后心电图异常率与介入诊疗操作前比较,差异无统计学意义(P>0.05);出血性脑血管病组患者介入诊疗操作后心电图异常率高于介入诊疗操作前,差异有统计学意义(P<0.05,见表2)。
表2 缺血性脑血管病组和出血性脑血管病组患者介入诊疗操作前后心电图异常率比较〔n(%)〕
Table 2 Comparison of the abnormality rate of ECG between ischemic cerebrovascular disease group and hemorrhagic cerebrovascular disease group before and after interventional diagnosis and treatment
组别例数操作前操作后χ2值P值缺血性脑血管病组481315(65.5)325(67.6)0.470.49出血性脑血管病组15414(9.1)38(24.7)13.33<0.01χ2值148.6187.64P值<0.01<0.01
3 讨论
普遍认为,脑血管(包括颈动脉)介入诊疗操作过程中未直接接触心脏,仅个别患者在拔除血管鞘时或拔鞘后加压包扎时,刺激迷走神经反射表现为血压下降、心率下降等。部分接受颈动脉支架植入术患者可能由于颈动脉压力感受器受刺激会一过性造成短暂性心率过缓或窦性停搏[1-2],但是既往研究显示,脑血管介入诊疗过程中仍易引起血管及心脏血流动力学的改变而导致心脏损害及相关的心电图异常改变[6]。接受脑血管介入诊疗的患者常有较重的脑血管病变如大面积脑梗死、脑出血或蛛网膜下腔出血,这一类人群既往均有较多报道,急性脑血管病后易发生脑心综合征等一系列心电异常改变及心脏损伤[7-9]。
本研究结果显示,635例脑血管病患者中发现心电图异常403例,异常率为63.5%。且随着年龄的增加心电图异常率增加,探究原因可能是,脑血管病多发生在中老年人群,即使既往无明显心脏病,但是患者在脑血管病变(缺血或出血)基础上常合并有高血压、糖尿病、肾功能不全、慢性支气管炎(慢性阻塞性肺病)等涉及全身动脉粥样硬化、心脏功能受损的危险因素,包括颈动脉、脑动脉、冠状动脉、甚至包括心肌肥厚重塑、窦房结心室传导纤维在内均可能已经受累[9]。本研究结果显示,缺血性脑血管病组及出血性脑血管病组患者心电图ST-T段改变发生率最高,与既往陈贞谊等[10]针对健康体检老年人心电图异常特征分析研究中的结果一致。
本研究发现,缺血性脑血管病组患者介入诊疗操作前心电图异常315例,异常率65.5%,介入诊疗操作后心电图异常325例,异常率67.6%,介入诊疗操作后心电图异常率并未显著增加,缺血性脑血管病组患者年龄偏大,介入诊疗操作前心电图异常检出率高,在接受介入诊疗操作后心电图异常在原有异常的基础上加重,虽然心电图异常率未显著增加,但是其心电图异常的危险系数及危险程度明显增加,因此提醒临床神经科介入诊疗医师需密切注意患者心脏的安全。另外本研究结果显示,出血性脑血管病患者介入诊疗操作后心电图异常率增加,此类患者可能总体病情较缺血性脑血管病严重,脑实质出血及蛛网膜下腔出血均会造成颅内压升高及颅内水肿,介入诊疗较缺血性脑血管病时间长,且部分患者需在全身麻醉下操作,自主神经功能紊乱,儿茶酚胺分泌增多,导致心脏功能紊乱出现[7],颅内血流动力学的异常改变,加上此类患者年龄相对较轻,心理情绪波动大,诸多因素叠加后最终造成出血性脑血管病患者在介入诊疗操作后心电图异常率明显增加,但是此类心电图异常改变常随着病情的稳定很快恢复正常,其绝大部分临床预后良好,无明显后遗症,仅需要在介入诊疗操作过程及介入诊疗操作后短期密切观察及对症处理。周建萍[11]曾报道5例患者的心电图因脑血管病引发尼加拉瀑布样T波改变,虽然上述极端情况较罕见,但在临床脑血管病的介入诊疗中需引起足够的重视。
彭应龙等[12]报道患者接受颈动脉支架成形术后,心动过缓发生率达到38.7%,由于本研究纳入接受颈动脉狭窄支架植入的样本量较少,故在缺血性脑血管病患者介入诊疗操作后窦性心动过缓发生率只有19.5%,但在实际临床,患者接受颈动脉支架成形术后发生的窦性心动过缓可能达到50%。因此,接受颈动脉支架成形术后的患者尤其术前合并有窦性心动过缓的老年患者更需在术后72 h内密切监测患者的生命体征,及时复查心电图。
本研究属于回顾性研究,纳入样本前就已经排除了相当一部分合并有高危心脏病及心律失常的患者,故结果可能有一定的误差,纳入样本时出血性脑血管病患者的年龄较缺血性脑血管病患者小,同时本研究纳入的患者基本上以脑血管介入诊断为主,接受颈动脉及颅内动脉支架或动脉瘤填塞等患者偏少也是一项缺陷,因此还有待于进一步进行前瞻性大样本的临床观察研究。
综上所述,介入诊疗与脑血管病患者的心电图异常有关,神经科医师在脑血管介入诊疗操作前后均需对患者心电图异常变化予以足够的关注,常规心电图检查在介入诊疗操作前后均有一定参考价值。本研究认为脑血管介入诊疗操作对患者心脏有一定影响,尤其应在介入诊疗操作过程及操作后短时间内注意心脏情况,多次做心电图检查,及时纠正心脏的异常改变,能够降低神经科临床脑血管介入诊疗操作引起的心脏相关危险及并发症。
[1]Cremonesi A,Castriota F,Secco GG,et al.Carotid artery stenting:an update[J].Eur Heart J,2015,36(1):13-21.
[2]Jauch EC,Saver JL,Adams HP Jr,et al.Guidelines for the early management of patients with acute ischemic stroke:a guideline for healthcare professionals from the American Heart Association/American Stroke Association[J].Stroke,2013,44(3):870-947.
[3]陈敏,贺婕.心理干预对脑血管介入治疗术后患者身心康复的影响[J]. 神经损伤与功能重建,2013,8 (3):227.
[4]全国第四届脑血管病学术会议标准(1995)[J].中华神经杂志,1996,29(6):376-381.
[5]Surawicz B,Childers R,Deal BJ,et al.AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram:part Ⅲ:intraventricular conduction disturbances:a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee,Council on Clinical Cardiology;the American College of Cardiology Foundation;and the Heart Rhythm Society:endorsed by the International Society for Computerized Electrocardiology[J].Circulation,2009,119(10):e235-240.
[6]Mylonas SN,Moulakakis KG,Antonopoulos CN,et al.Carotid artery stenting-induced hemodynamic instability[J].J Endovasc Ther,2013,20(1):48-60.
[7]Shi JH,Hu RL,Yang YQ,et al.Correlation between QT dispersion and serum enzyme changes in patients with acute cerebrovascular disease[J].Journal of Chongqing Medical University,2013,33(11):1341-1343.(in Chinese) 石金河,户瑞丽,杨亚勤,等.心电图QT离散度与急性脑血管病患者血清酶学变化相关性研究[J].重庆医科大学学报,2013,33(11):1341-1343.
[8]Xie YH.Characteristic analysis of ECG changes of cerebrocardiac syndrome caused by acute cerebral vascular disease[J].Chinese Journal of Modern Drug Application,2014,8(11):18-19.(in Chinese) 谢玉华.急性脑血管病致脑心综合征心电图改变的特点分析[J].中国现代药物应用,2014,8(11):18-19.
[9]Dutta P,Courties G,Wei Y,et al.Myocardial infarction accelerates atherosclerosis[J].Nature,2012,487(7407):325-329.
[10]Chen ZY,Yan P.Characteristic analysis on electrocardiography abnormalities of the elderly in physical check[J].Geriatrics & Health Care,2013,19(6):385-387.(in Chinese) 陈贞谊,颜平.健康体检老年人心电图异常特征分析[J].老年医学与保健,2013,19(6) 385-387.
[11]Zhou JP.Five cases of electrocardiogram of cerebrovascular diseaae which trigger Niagara falls T wave changes[J].Chinese Journal of Cardiac Arrhythmias,2010,14(2):152-153.(in Chinese) 周建萍.脑血管疾病引发尼加拉瀑布样T波改变心电图五例[J].中华心律失常学杂志,2010,14(2):152-153.
[12]Peng YL,Song L,Tong XQ,et al.Analysis of factors causing hemodynamic instability in performing carotid artery angioplasty with stenting[J].Journal of Interventional Radiology,2013,22(7):535-539.(in Chinese) 彭应龙,宋莉,佟小强,等.颈动脉支架成形术血流动力学改变的影响因素分析[J].介入放射学杂志,2013,22(7):535-539.
(本文编辑:陈素芳)
Clinical Study of Abnormal Changes in Electrocardiograph After Interventional Diagnosis and Treatment of Patients With Cerebrovascular Disease
LUZhen-chan,SHENShuang,ZHANGBing,etal.
DepartmentofNeurology,HuzhouCentralHospital,Huzhou313000,China
Objective To investigate the abnormal changes of electrocardiogram(ECG) after interventional diagnosis and treatment of patients with cerebrovascular disease.Methods We enrolled 635 patients with cerebrovascular disease who were admitted into the Department of Neurology of Huzhou Central Hospital and received interventional diagnosis and treatment there from January 2011 to February 2014.According to the type of cerebrovascular disease,481 patients were assigned into ischemic cerebrovascular disease group and 154 patients were assigned into hemorrhagic cerebrovascular disease group.Before and after interventional diagnosis and treatment,ECG examination was conducted,and the ECG results were analyzed in combination with age and the type of cerebrovascular disease.Results Of the 635 patients,abnormal changes of ECG occurred in 403,with an abnormality rate of 63.5%.Among patients younger than 45,13 (14.6%) patients had abnormal changes in ECG;among patients aged 45 to 60,80 (38.1%) had abnormal changes in ECG;among patients older than 60,310 (92.3%) had abnormal changes in ECG.Patients of different age ranges were significantly different (χ2=5.52,P<0.01) in the abnormality rate of ECG.In ischemic cerebrovascular disease group,abnormal ECG changes occurred in 362 (75.3%) patients,and in hemorrhagic cerebrovascular disease group,abnormal ECG changes occurred in 41 patients(26.6%),with significant difference between the two groups (χ2=119.00,P<0.01).Before and after interventional diagnosis and treatment,ischemic cerebrovascular disease group was higher (P<0.05) than hemorrhagic cerebrovascular disease group in the abnormality rate of ECG.The abnormality rate of ECG of ischemic cerebrovascular disease group after interventional diagnosis and treatment was not significantly different (P>0.05) from that before interventional diagnosis and treatment;the abnormality rate of ECG of hemorrhagic cerebrovascular disease group was higher (P<0.05) than that before interventional diagnosis and treatment.Conclusion Interventional diagnosis and treatment is related with ECG abnormality.The perfection of ECG examination could timely find the cardiac risk during interventional diagnosis and treatment of patients with cerebrovascular disease.
Cerebrovascular disorders;Electrocardiography;Diagnosis;Therapy
湖州市科技计划项目(2013GYB01)
313000浙江省湖州市中心医院神经内科(卢振产,沈双,张冰),心内科(俞子恒,程震峰)
卢振产,313000浙江省湖州市中心医院神经内科;E-mail:ganlanshu1227@163.com
R 743
B
10.3969/j.issn.1007-9572.2015.24.017
2014-12-10;
2015-06-27)

