Efficacy of biofeedback therapy via a miniwireless device on sleep bruxism contrasted with occlusalsplint:a pilot study
WeiPing Gu,Jie Yang,FeiMin Zhang,XinMin Yin,XiaoLong Wei,Chen Wang
1Jiangsu Key Laboratory ofOral Diseases,Nanjing Medical University;Departmentof GeneralDentistry,Affiliated Hospitalof Stomatology,Nanjing Medical University,Nanjing,Jiangsu 210029,China;
2Jiangsu Key Laboratory of Oral Diseases,Nanjing Medical University;Department of Stomatology,Jiangsu province Geriatric Institution,Jiangsu Province Official Hospital,Nanjing,Jiangsu 210029,China;
3Jiangsu Key Laboratory of Oral Diseases,Nanjing Medical University;Department of Prosthodontics,Affiliated Hospital of Stomatology,Nanjing Medical University,Nanjing,Jiangsu 210029,China;
4Department of Stomatology,Benq Medical Center,Nanjing Medical University,Nanjing,Jiangsu 210019,China;
5College of Automation Engineering,Nanjing University of Aeronautics and Astronautics,Nanjing,Jiangsu,210016,China.
Efficacy of biofeedback therapy via a miniwireless device on sleep bruxism contrasted with occlusalsplint:a pilot study
WeiPing Gu1,Jie Yang2,FeiMin Zhang3,✉,XinMin Yin4,XiaoLong Wei5,Chen Wang3
1Jiangsu Key Laboratory ofOral Diseases,Nanjing Medical University;Departmentof GeneralDentistry,Affiliated Hospitalof Stomatology,Nanjing Medical University,Nanjing,Jiangsu 210029,China;
2Jiangsu Key Laboratory of Oral Diseases,Nanjing Medical University;Department of Stomatology,Jiangsu province Geriatric Institution,Jiangsu Province Official Hospital,Nanjing,Jiangsu 210029,China;
3Jiangsu Key Laboratory of Oral Diseases,Nanjing Medical University;Department of Prosthodontics,Affiliated Hospital of Stomatology,Nanjing Medical University,Nanjing,Jiangsu 210029,China;
4Department of Stomatology,Benq Medical Center,Nanjing Medical University,Nanjing,Jiangsu 210019,China;
5College of Automation Engineering,Nanjing University of Aeronautics and Astronautics,Nanjing,Jiangsu,210016,China.
The putative causes ofbruxism are multifactorialand there are no definite measures forbruxism management.The aim ofthis study was to evaluate the efficacy ofbiofeedback therapy on sleep bruxism,compared with occlusalsplint. Twenty-fourvolunteers with sleep bruxism were divided into two groups:the GTB group thatwere treated with biofeedback therapy(n=12)and the GTO group thatwere treated with occlusalsplint(n=12).A minipressure sensor integrated with a monitoring circuitby use ofa maxillary biofeedback splintwas fabricated.To fosterthe relaxation of the masticatory muscles and the nervous system,the wireless device received signals from bruxism events and vibrationsalerted the bruxerwhen the threshold wasexceeded.Totalepisodes and average duration ofbruxism eventsduring 8 hours of sleep were analyzed with the monitoring program(TRMY1.0).After 6 and 12 weeks,the episodes(P= 0.001)and duration(P<0.05)in the GTB group declined dramatically.In contrast,there were no significantdifferences in the GTO group after the treatment(P>0.05).Furthermore,the episodes had significant differences between the GTB group and the GTO group afterthe same period oftreatment(P=0.000).The resultssuggestthatbiofeedback therapy may be an effective and convenientmeasure for mild bruxers,when compared with occlusalsplinttherapy.The miniwireless biofeedback method may be of value for the diagnosis and managementof bruxism in the future.
sleep bruxism,biofeedback,occlusalsplint,miniaturization,vibration,wireless technology
Introduction
Bruxism is an oral parafunction characterized by clenching and grinding of teeth during wakefulness or sleep.Awake bruxism(AB),often known as tooth clenching,is mainly associated with anxiety,life stress including work pressure and family responsibilities[1-4], and a number of psychopathological symptoms[5]. In geriatric patients,awake bruxism is frequently observed in frontotemporal dementia,and normalpressure hydrocephalus which characteristically shows frontallobe dysfunction and can be regarded as a frontal neurologicalsign of various disorders[6].Sleep bruxism (SB),which mostly occurs during night,is an oromandibular behavior defined as a stereotyped movement characterized by tooth grinding and/or clenching[7,8]. According to the International Classification of Sleep Disorders Version 2(ICSD-2),SB isclassified asa sleep related movementdisorderusually associated with sleep arousals[9].Both AB and SB may be also associated with various movements and degenerative disorders,such as oromandibulardystonia and Huntingtonˊs disease[10].
The prevalence of SB in the adultpopulation isestimated to be approximately 8-10%[11].The majornegative impacts of bruxism on health include tooth attrition and destruction[12];risk factors associated with increased mechanicaland/or technicalcomplications in prosthodontic rehabilitation[13];contribution to(not simple cause-effectrelationship)chronic masticatory myofascial pain[14,15];exacerbation of temporomandibular disorders or induction of temporaltension headache;grinding sounds thatmay interfere with the sleep offamily orlife partners[16,17].
Generally speaking,the putative etiology of SB has multiple factors including genetic factors,some drugs and medications,psychosocialfactors,and centralnervous system orcombined factors[18,19].Information aboutgenetic predisposition to SBstemsmostly from studiesbased on questionnaires or analyses ofmonozygotic twin populations,some drugs(alcohol,caffeine,and tobacco)and medications(e.g.,selective serotonin re-uptake inhibitors, benzodiazepines,and dopaminergic drugs),which have relationship with the etiopathogenesis of SB[20].At present,sleep arousal,autonomic sympathetic-cardiac activation,neurotransmitters and other centralfactors play major roles in the genesis of SB.Psychosocial components,such as anxiety and stress may be risk factors for SB[21].Treatment modalities for bruxism involve reversible occlusalcorrection,behavioralchanges and pharmacologicalapproaches[22].The mostcommon method ofreversible occlusaladjusting formany bruxers is the use of occlusalappliance.However,the inherent effect of an occlusalsplint has been found to be the protection of tooth wear rather than the alleviation of bruxism behavior itself[23].One of the behavioral approaches is the biofeedback method for bruxism;the efficacy has been reported by many researchers.The majority of these devices rely on electromyography (EMG)ofthe masticatory muscles[24,25].
However,there are some disadvantages of EMG biofeedback devices,i.e.,the EMG signals can be affected by electrode position,posture and skin resistance.Itisalso difficultforbruxersto tolerate the device wellwhile asleep with the electrodesattached on masseter and/or temporalis muscles[26].So far,there is no approach that is effective for bruxism management. The purpose ofthis study is to evaluate the efficacy of biofeedback therapy on SB via a miniwirelessbiofeedback device contrasted with occlusalsplint.We sought to determine whether the awareness of clenching or grinding ofteeth can alleviate the episodes of bruxism behavioritselfafterseveralweeksoftraining and learning in bruxers.
Materials and methods
Mini wireless biofeedback device
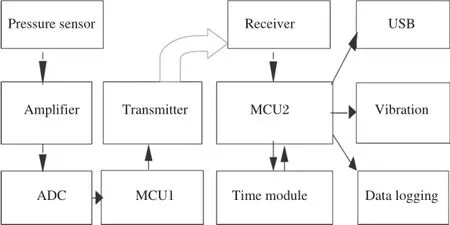
Fig.1The mini wireless biofeedback system.The signals were transformed from the analog-to-digitalconverter(ADC)to microcontroller unit (MCU1 and MCU2,MSP430F4152,Texas Instrument,USA),which has ultra lowerpowerconsumption with active mode of200μA,1 Mhz and 2.2 v.
The configuration of the proposed system used for monitoring and vibration is shown in Fig.1.The pressure sensor(HU-101,SaiYing Electronics Technology Development Inc.Bengbu,China)was embedded 0.5-1 mm below the surface ofa maxillary biofeedback splint(Jing Yi Denture Co.Ltd.,Nanjing,China)atthe pointcontacted by the mandibular canine in the intercuspalposition.A stabilization splint,which covers the maxillary or mandibular fulldentalarch,is rather large[11,27].In consideration ofthe bruxerˊs comfort,the design of a biofeedback splint(Fig.2A)is different from a traditionalanterior or stabilization splint.An anterior splintis smalland covers some ofthe anterior teeth.Because the button cell(CR2025,Panasonic, Indonesia,20 mm×2.5 mm)and minimonitoring circuit(18 mm×16 mm×5 mm,Fig.2B)are designed to be packed into the splint,itis essentialto extend the margin ofthe splintto the lingualsurfaceofbilateralmaxillary premolars.
The wireless transmitter sent the signals of bruxism events per second and the signals were received by a watch style device.When the value exceeded the threshold,as clenching or grinding of teeth occurred during sleep,the watch vibrated to inform the bruxer of the abnormal movement of teeth and induce voluntary relaxation of the masticatory muscles and nervous system(Fig.2C and 2D).
Software for analysis of bruxism events
The software(TRMY 1.0,Nanjing Jing Tong Ren Biological Technology Co.,Ltd,Nanjing,China)was developed in Labwindows 8.5(National instruments, USA).The analysis of bruxism events through the USB ofthe vibration device included the value ofbite force,the occurring time(year/month/day/hour/minute/ second)and the duration in specific intervals,asshowing in Fig.3.
Validation of the mini wireless biofeedback device
The patent of the mini biofeedback device was approved by State Intellectual Property Office of China in 2012[28].For evaluating the validity of the device,the authors simultaneously compared the device with polysomnography(PSG,Alice 5 Diagnostic Sleep System,Philips Respironics.Inc,USA)in bruxers. The PSG was provided by the Departmentof Oraland MaxillofacialSurgery,Affiliated HospitalofStomatology, Nanjing MedicalUniversity.The sensitivity was 88.1% and the specificity was 84.5%in detection of bruxism events(Fig.4A and 4B)(109 detections for PSG and 96 detections of bruxism events for monitoring device. Bruxism was diagnosed as previously described[21,29]).
Experiment protocol subjects
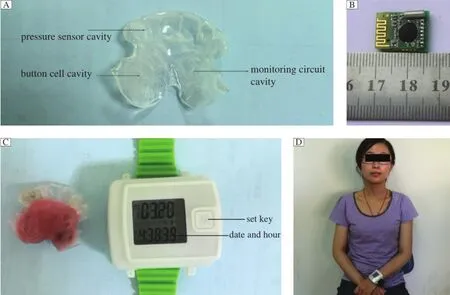
Fig.2Mini wireless biofeedback device.A:The margin of the biofeedback splintextends to the lingualsurface of the bilateralmaxillary second premolars.The cavity design for placement of the pressure sensor,monitoring circuit and button cell.B:Mini-monitoring circuit (18 mm×16 mm×5 mm).C:A maxillary biofeedback splint with pressure sensor,monitoring circuit and button cell embedded(left),a watch style vibration device(right).D:A bruxer with the maxillary biofeedback splint for monitoring and the wireless vibration device.Use of photo was permitted by the study subject.
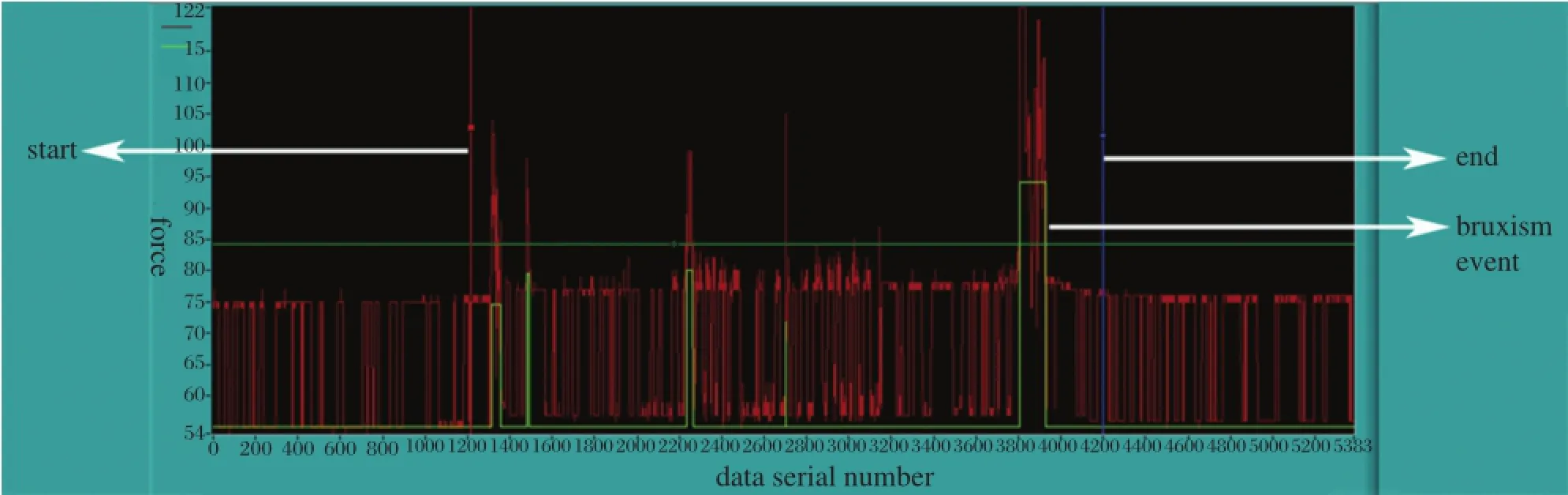
Fig.3A result sample of monitoring device.The irregularred lines demonstrate bite forces during sleep,the area between a red and blue line(the white arrow)is the interval for analysis,the green rectangles represent episodes of bruxism events.
Twenty-four outpatients with a diagnosis of SB were recruited between December 2011 and May 2013 from the Department of General Dentistry,Affiliated Hospitalof Stomatology,Nanjing Medical University. The subjectswere assignedto the GTB group(9 females, 3 males,mean age 26.6±5.0 years)and the GTO group (10 females,2 males,mean age 24.7±5.5 years)using a random numbertable.
The inclusion criteria were:bruxers between the ages of 20-40 years,>six month history of bruxism (according to American Academy of Sleep Medicine (AASM)clinicaldiagnostic criteria for SB[21])which was confirmed by clinical examination and bed-partner orfamiliesand no history ofpsychologicaland neurotic diseases.Patients undergoing treatmentfor temporomandibular disorders and patients with organic nerve disease were excluded from the experiment.Excluded treatments included botulinum toxin injection and/or use of other drugs to reduce masseter and temporalis muscle hyperactivity because of some effects that are similar with biofeedback therapy for managementof bruxism and may interfere with the resultsofthis study. Enrollmentofparticipants and the experimentalprocedures in this study were conducted in accordance with the Declaration of Helsinki(revised in Edinburgh 2000).Allsubjects signed an informed consentform to participate in a protocol that had been approved by the Ethics Committee of Affiliated Hospital of Stomatology,Nanjing Medical University.
Experimental procedure
Dental impressions for each of the participants in GTB and GTO were taken formanufacturing the maxillary biofeedback splintdesigned as Fig.2A.A baseline of episodes,duration,and a biting force value for each bruxer was determined withoutvibration during the firstthree nightsby setting the threshold to the maximum.The threshold was set to a normal value,which was determined by using the mean value of the biting force,calculated in specific intervals(e.g.,one minute, one hour and 8 hours)via TRMY 1.0,and the duration of≥3s[30].When the threshold was exceeded,the bruxers in the GTB group would become conscious of clenching or grinding of teeth during sleep and relax themselvesvia alleviating the tension ofthe masticatory musclesand nervoussystem.In contrast,the GTOgroup were treated with a maxillary biofeedback splintwithout vibration by setting the threshold to the maximum value during the treatmentperiod.Six and 12 weeks after therapy in each group,the episodes and duration of bruxism events were monitored and recorded again by use of the miniwireless monitoring device during 8 hours ofsleep fordata collection.
Statistical analysis
The total episodes and durations of bruxism events during 8 hours of sleep were analyzed after 6 and 12 weeks of therapy.Within each group,the difference between pre-and post-treatment,and the efficacy of biofeedback therapy versus occlusalsplinttreatment between GTB and GTO were assessed by univariate ANOVA.The multiple comparisons ofthe post-hoc test were performed with Tukey HSD test to determine which groups had significantdifferences between and within GTB and GTO in SPSS version 19.0(IBM SPSS Statistics,Chicago,IL,USA).A probability value of P<0.05 was considered statistically significant.
Results
Totalepisodes and duration of bruxism events in GTB and GTO at the beginning
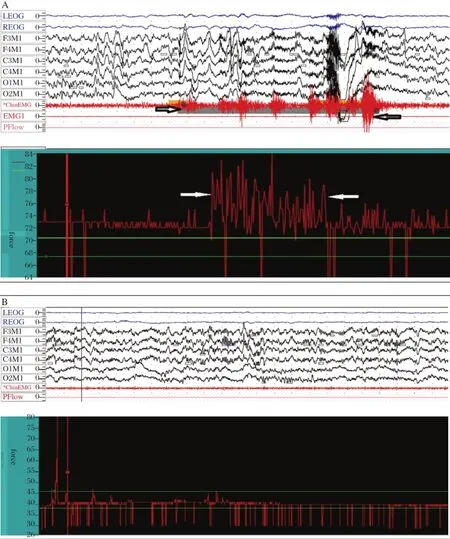
Fig.4 The images of polysomography(PSG)and the monitoring device.A:The comparison of a polysomography and the monitoring device;the PSG demonstrates a bruxism event,which consisted of a series of EMG activities,with the amplitude reaching 20%maximum voluntary contraction(MVC),and the duration is more than 2 seconds.In contrast,the monitoring device demonstrates a series of serrations with the amplitude of force exceeding 20%of the maximum bite force(relative to the baseline)during intercuspal position and the duration was no less than 3 seconds.B: Demonstration of the EMG amplitude of masseter muscle during sleep with no remarkable changes,while the monitoring device also presented the baseline value of bite force without significant changes during sleep simultaneously.
The average total episodes of bruxism events during 8 hours ofsleep were 10.2±2.8(range,7 to 16)times in GTB atthe beginning.In GTO,the average totalepisodes of bruxism events were 11.9±5.7(range,4 to 21)times.The duration of bruxism events in GTB ranged from 5 to 40 seconds(mean,17.3±9.6 s).In GTO, the duration ranged from 6 seconds to 24 s;the average duration was 14.8±5.5 seconds.There were no significantdifferences between GTB and GTO,both in total episodes(P=0.883)and duration of bruxism events (P=0.907).For the occurrence times,bruxism events were observed throughout the sleep.
Efficacy of GTB and GTO after 6 and 12 weeks of therapy
The totalepisodes and duration in GTB and GTO, before,after 6 and 12 weeks of therapies are illustrated in Fig.5A and Fig.5B.The differences in episode and duration before and after in GTB had statistical significance(episodes P=0.001,duration P=0.026 and 0.012 respectively).However,there were no significant differences in GTO comparing bruxism events atthe baseline with 6 and 12 weeks after occlusalsplint therapy(all P>0.05).
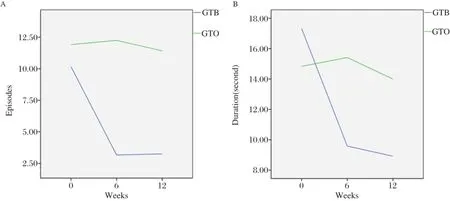
Fig.5Efficacy of GTB and GTO after 6 and 12 weeks of therapy.A:The total episodes in GTB declined dramatically from the beginning to the end of 6 and 12 weeks after biofeedback therapy(P=0.001),while there are no significant differences in GTO(6 weeks,P=0.998.12 weeks, P=0.970).B:The duration in GTB has significant difference between 6 and 12 weeks after biofeedback therapy compared to baseline(6 weeks, P=0.026,12wks,P=0.012),while similar results cannot be found in GTO(P=0.999).
Asshown in Table 1,post6 and 12 weeksoftherapy, the total episodes of bruxism events during 8 hours of sleep in GTBwere(3.2±1.2)timesand(3.3±1.4)times. The episodes in GTO were(12.3±6.0)times and (11.4±3.7)times,and there were significantdifferences between GTB and GTO(all P=0.000)after therapy.The average duration ofbruxismevents in GTBwas(9.6±3.2) seconds and(8.9±2.7)seconds,and the duration in GTO was(15.4±6.0)seconds and(14.0±6.1)s.There were no significant differences(P=0.172 and P=0.305) comparing GTB with GTO.Furthermore,there were no significant differences of episodes and duration between 6 and 12 weeks in GTB and GTO(all P>0.05)after biofeedback and occlusal splint therapy.Sleep quality in GTB and GTO
Pittsburgh Sleep Quality Index(PSQI)[31]is a useful instrumentin measuring sleep quality.The sleep quality of each subjectwas evaluated by PSQI based on the bruxerˊs self-report.Two in GTB and one in GTO reported some interferences with sleep,and the value of PSQIwas higherthan five(5-10)according to the survey of PSQIin this study.
Discussion
The etiology and neurologicalmechanism thatgenerate SB are not well understood.During the past decades, researchers have focused on centralfactors rather than peripheralfactors(e.g.,occlusalfactors)[17,32,33].However, occlusalsplintformanagementof bruxism is currently the standard for mostdentists.Though a number of reports have been published with descriptions of the efficacy of these reversible occlusalinterventions[34], many patients show little improvement in SB after having endured long-term occlusion adjusting therapy. Van der Zaag etal.[35]observed large differences among individuals with stabilization splints.Some of them indeed showed a decrease in bruxism activity(19%-29%),while othersshowed no change oreven an increase(33%-48%).This suggests thatthe effectof occlusal modification has contributed much more to the protection of naturalteeth and less to stopping the behavioral movement of bruxism itself[27].
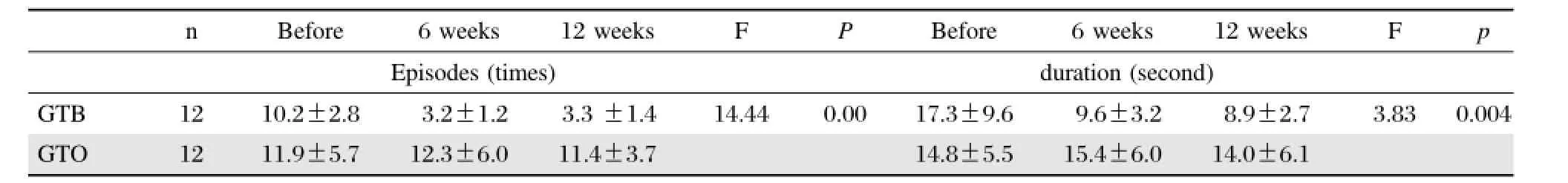
Table 1 Total episodes and duration of bruxism events during 8 hrs sleep before,6 and 12 weeks after
Due to reasons mentioned above,the use ofmedications(e.g.,botulinum toxin,L-dopa,SSRI,and propranolol)in the management of bruxism has been increasingly studied in recentyears.Some drugs have a paralytic effecton masticatory muscles by inhibition ofacetylcholine release atthe neuromuscularjunction, e.g.,botulinum toxin[36,37].So far,its application in the managementof bruxism is mainly described in case reports and in randomized clinicaltrials(RCT)which have also been recently reported[38].In short,it was shown thatSB did improve with frequently prescribed, non-specific muscle relaxant medicines[39];the effectiveness of botulinum toxin has been reported for many neurologicaldisorders[40].Although the maintenance of therapeutic efficacy and the influence of these medicines on bruxism have not been fully understood,its long-term tolerability and the risk of addiction need further attention.
An alternative measure for managementof bruxism is behavioral approaches,which has been tried for many years.The biofeedback method uses the concept that bruxers can unlearn their undesired behaviors when a stimulus makes them aware of their adverse muscle activities.This technique has been applied for bruxism during wakefulness as wellas for SB.While awake,patients can be trained to control their jaw muscle activities through auditory or visualfeedback from a surface EMG.
Auditory,electrical,vibratory and even taste stimuli can be used for SB feedback[24,25,41,42].The majority of case reports regard the biofeedback method to be an effective measure for the management of bruxism. Among these reports,the better design was a biofeedback device invented by Jadidietal.[24],which is based on EMG ofthe temporalis withoutsubstantialsleep disturbance.Generally,bruxism diagnosis and biofeedback devices are based on monitoring masticatory muscle activity using surface electromyography.However,the surface EMG signalis affected by many factors such as electrode position,posture and skin resistance.In addition,attachmentofmultiple electrodesto the bruxerˊs face by a dentist or the bruxer without causing bruxer discomfortorsleep disruption is noteasy orconvenient. Severalresearchers have tried to measure SB activity directly by using an intra-oral appliance.Nishigawa etal.[30]measured bite force using a strain-gauge transducerincorporated into a bite-guard.Thisdevice wasan analogue pressure sensorwith electricalwires connected outofthe mouth during sleep.Anotherpatentproposed a device which tracks the position of the jaw using an opticalsensing unit,butitrequired an upperand lower splint,as the lightemitter and the detector were separated on each splint[43].
Therefore,despite the number of techniques that have been developed to detect and treat bruxism in the clinic,a practicalmethod is stillnot available for bruxers to effectively and conveniently use.Compared to otheroraldevicesformonitoring and treating bruxism, the characteristics ofthe biofeedback device the authors have proposed in thisstudy are as follows:(i)The miniature maxillary biofeedback splintis integrated into one packet.As shown in Fig.2the splintcovers from the rightcanine to the leftcanine with the margin extending to the lingualsurface of the bilateral premolars.The design took into consideration both the patientˊscomfort and adequate cavitiesforembedding the monitoring circuit.A large splintoften feelsuncomfortable,compared with a minione.Moreover,some studies showed thata thick splintcan decrease rhythmic masticatory muscle activity(RMMA)in bruxers.However,the effectseems to be transitory[23].To reduce the thickness of splintˊs effects on bruxism behavior and the oromandibular motor system,the authors designed the cavities forthe pressure sensor,circuit and button cellusing a wax model.The thickness of the contactpointbetween the upper and lower canine is about0.5 mm less than an ordinary resin splint in the intercuspalposition,with no obvious contactin the mandibularposturalposition; (ii)The biofeedback systemˊs operation is based on pressure-orient,which has distinctdifference from an EMG-based device.The benefitof EMG is thatit is more objective in evaluating bruxism events.However, there are some disadvantages to EMG as mentioned above.The wirelessfeature addressesthe mostimportant considerations,patientcomfortand ease ofuse;(iii)The biofeedback device incorporates monitoring with biofeedback function and the threshold is convenientto modify subject to different circumstances.In many studies,the biofeedback devices relied on audio[44],which has the major disadvantage of sleep disturbance.In the development of this device,accurate vibration time was determined by a watch style device which is worn on the bruxerˊs wrist.In some cases,the patients may be conscious of bruxism behavior by feeling the vibration of the wrist without substantial waking.
There is no definite method for the managementof bruxism with evidence-based tests to date.According to the data from subjects recruited in this study,the GTB results suggest that the total episodes of bruxism events had decreased dramatically,and had statistical significance from the baseline to 6 and 12 weeks afterbiofeedback therapy during 8 hours of sleep(P= 0.001).Furthermore,the average duration had also declined in the participants from the preliminary night to the end of 6 and 12 weeks study period(P=0.026 and 0.012).In contrast to GTO,there were no significantdifferences in episodes and duration(all P>0.05). Meanwhile,there were significantdifferences in episodes between GTB and GTO after treatment(all P=0.000).As the splinthas the same design ofstructure and thickness for GTB and GTO,itis reasonable to assume the different efficacy in GTB resulted from the biofeedback method.However,despite having no universalstandard for grading the severity of bruxism events at present,it is very important to narrow the resultsˊinterpretation.In this study,the totalepisodes ofbruxism events ranged from 4 to 21 times in the baseline,indicating thatthe participants actually had‘mild bruxism’.In other words,based on the results of this study,itis difficultto assume thatthe biofeedback therapy can be effective for allbruxers.The results have similar findings with some other reports,such as Jadidi et al.and Watanabe et al.[24,40],mentioned above. The occlusalsplinttherapy in GTO demonstrated the indefinite results in the managementof bruxism.The findingsafter6 and 12 weeksoftherapy are similarwith Van der Zaag et al.[35],some of the bruxers have improvement of bruxism events(three bruxers out of twelve have improved their bruxism behaviors).The mean awake time in GTB is about3-4 times pernight withoutobvious disturbance of sleep,according to the Pittsburgh Sleep Quality Index(PSQI)[31]survey with the bruxersˊself-reports(two in GTB and one in GTO have higher scores than five).This study suggests that the efficacy of biofeedback therapy on SB is relative to the bruxersˊself-awarenessoftheirbehaviorin bruxism eventsand the relaxation self-training,especially on the alleviation ofepisodes ofbruxism events.Whether the putative mechanism of biofeedback lies in GTB is in connection with the relaxation of masticatory muscles or has effects on the central nervous system needs furtherresearch.
In conclusion,the miniwireless biofeedback device hasproposed an effective,novel,and convenientmethod forbruxism therapy when contrasted with occlusalsplint in this study.The totalepisodes and average duration were decreased remarkably after6 and 12 wks therapy. Awarenessofclenching orgrinding ofteeth can alleviate the episodes of bruxism behavior itself after several weeksˊtraining and learning in mild bruxers.
Acknowledgments
We would like to thank Professor XiaoFeng Song and Professor ZhiYu Qian for their kind help with the miniwirelessdevice development.The Bureau ofHealth of Jiangsu Province supported this study(H200939).A Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD,2014-37)supported this study.
[1]Winocur E,Uziel N,Lisha T,etal.Self-reported bruxism -associations with perceived stress,motivation forcontrol, dentalanxiety and gagging.J OralRehabil2011;38(1):3-11.
[2]Rao SK,BhatM,David J.Work,stress,and diurnalbruxism: a pilot study among Information technology professionals in Bangalore city,India.Int J Dent2011;2011:650489.
[3]van Selms MK,Lobbezoo F,Wicks DJ,et al.Craniomandibular pain,oral parafunctions,and psychological stress in a longitudinal case study.J Oral Rehabil 2004; 31(8):738-745.
[4]Endo H,Kanemura K,Tanabe N,etal.Clenching occurring during the day is influenced by psychologicalfactors. J Prosthodont Res 2011;55(3):159-164.
[5]Manfredini D,Lobbezoo F.Role of psychosocial factors in the etiology ofbruxism.J Orofac Pain 2009;23(2):153-166.
[6]Kwak YT,Han IW,Lee PH,et al.Associated conditions and clinical significance of awake bruxism.Geriatr Gerontol Int 2009;9(4):382-390.
[7]De Laat A,Macaluso GM.Sleep bruxism as a motor disorder.Mov Disord 2002;17(suppl):S67-S69.
[8]Bader G,Lavigne G.Sleep bruxism;an overview of an oromandibular sleep movement disorder.Review Article. Sleep Med Rev 2000;4(1):27-43.
[9]Thorpy MJ.Classification of sleep disorders.Neurotherapeutics 2012;9(4):687-701.
[10]Chokroverty S.Overview of sleep&sleep disorders. Indian J Med Res 2010;131:126-140.
[11]Lobbezoo F,van der Zaag J,van Selms MK,et al. Principles for th e management o f brux ism.J Oral Rehabil2008;35(7):509-523.
[12]Tsigg os N,Torto pidis D,Hatzik yriakos A,et al. Association between self-reported bruxism activity and occurrence of dentalattrition,abfraction,and occlusalpits on natural teeth.J Prosthet Dent 2008;100(1):41-46.
[13]Johansson A,Omar R,Carlsson GE.Bruxism and prosthetic treatment:a critical review.J Prosthodont Res 2011;55(3):127-136.
[14]Velly AM,Gornitsky M,Philippe P.Contributing factors to chronic myofascial pain:a case-control study.Pain 2003;104(3):491-499.
[15]Svensson P,Jadidi F,Arima T,et al.Relationships between craniofacial pain and bruxism.J Oral Rehabil 2008;35(7):524-547.
[16]Fernandes G,Franco AL,Siqueira JT,etal.Sleep bruxism increases the risk for painfultemporomandibular disorder, depression and non-specific physical symptoms.J Oral Rehabil 2012;39(7):538-544.
[17]Koyano K,Tsukiyama Y,Ichiki R,et al.Assessment of bruxism in the clinic.J Oral Rehabil2008;35(7):495-508. [18]Lavigne GJ,Khoury S,Abe S,et al.Bruxism physiology and pathology:an overview for clinicians.J Oral Rehabil 2008;35(7):476-494.
[19]Behr M,Hahnel S,Faltermeier A,etal.The two main theories on dental bruxism.Ann Anat 2012;194(2):216-219.
[20]de la Hoz-Aizpurua JL,D az-Alonso E,LaTouche-Arbizu R,et al.Sleep bruxism.Conceptual review and update. Med Oral Patol Oral Cir Bucal 2011;16(2):e231-e238.
[21]Carra MC,Huynh N,Lavigne G.Sleep bruxism:a comprehensive overview for the dental clinician interested in sleep medicine.DentClin North Am 2012;56(2):387-413.
[22]Shetty S,Pitti V,Satish Babu CL,et al.Bruxism:A Literature Review.J Indian Prosthodont Soc 2010;10(3): 141-148.
[23]Klasser GD,Greene CS.Role of oral appliances in the management of sleep bruxism and temporomandibular disorders.Alpha Omegan 2007;100(3):111-119.
[24]Jadidi F,Castrillon E,Svensson P.Effect of conditioning electricalstimulion temporalis electromyographic activity during sleep.J Oral Rehabil 2008;35(3):171-183.
[25]Watanabe A,Kanemura K,Tanabe N,et al.Effect of electromyogram biofeedback on daytime clenching behavior in subjects with masticatory muscle pain.J Prosthodont Res 2011;55(2):75-81.
[26]Kim JH,McAuliffe P,OˊConnellB,etal.Developmentof wireless bruxism monitoring device based on pressuresensitive polymer composite.Sensors and Actuators A: Physical 2010;163(2):486-492.
[27]Klasser GD,Greene CS,Lavigne GJ.Oral Appliances and the Management of Sleep Bruxism in Adults:A Century of Clinical Applications and Search for Mechanisms.Int J Prosthodont 2010;23(5):453-462.
[28]XiaoLong Wei,WeiPing Gu,ZhiYu Qian,et al.A biofeedback device for bruxism.China.201120149478.2, January 4,2012.
[29]Doering S,Boeckmann JA,Hugger S,et al.Ambulatory polysomnography for the assessment of sleep bruxism. J Oral Rehabil 2008;35(8):572-576.
[30]Nishigawa K,Bando E,Nakano M.Quantitative study of bite force during sleep associated bruxism.J Oral Rehabil 2001;28(5):485-491.
[31]Buysse DJ,Reynolds CF 3rd,Monk TH,et al.The Pittsburgh Sleep Quality Index:a new instrumentfor psych iatric p ractic e an d researc h.Psyc h ia try Res 1989;28(2):193-213.
[32]Lavigne GJ,Kato T,Kolta A,et al.Neurobiological mechanisms involved in sleep bruxism.Crit Rev Oral Biol Med 2003;14(1):30-46.
[33]Lobbezoo F,Naeije M.Bruxism is mainly regulated centrally,not peripherally.J Oral Rehabil 2001;28(12): 1085-1091.
[34]MadaniAS,Abdollahian E,Khiavi HA,etal.The efficacy of gabapentin versus stabilization splint in managementof sleep bruxism.J Prosthodont2013;22(2):126-131.
[35]Van der Zaag J,Lobbezoo F,Wicks DJ,et al.Controlled assessmentof the efficacy of occlusal stabilization splints on sleep bruxism.J Orofac Pain 2005;19(2):151-158.
[36]Pidcock FS,Wise JM,Christensen JR.Treatmentof Severe Post-Traumatic Bruxism With Botulinum Toxin-A:Case Report.J Oral Maxillofac Surg 2002;60(1):115-117.
[37]Santamato A,Panza F,Di Venere D,et al.Effectiveness of botulinum toxin type A treatment of neck pain related to nocturnal bruxism:a case report.J Chiropr Med 2010;9(3):132-137.
[38]Lee SJ,Mc Call WD Jr,Kim YK,et al.Effect of Botulinum Toxin Injection on Nocturnal Bruxism.Am J Phys Med Rehabil 2010;89(1):16-23.
[39]Long H,Liao Z,Wang Y,et al.Efficacy of botulinum toxins on bruxism:an evidence-based review.Int Dent J 2012;62(1):1-5.
[40]Jankovic J.Disease-oriented approach to botulinum toxin use.Toxicon 2009;54(5):614-623.
[41]Watanabe T,Baba K,Yamagata k,et al.A vibratory stimulation-based inhibition system for noctural bruxism: a clinical report.J Prosthet Dent 2001;85(3):233-235.
[42]Nissani M.Can Taste Aversion Prevent Bruxism.Appl Psychophysiol Biofeedback 2000;25(1):43-54.
[43]John D.Summer,Erik Bodegom,Allen Lee.Intra-oral jaw tracking device.U.S.Patent 5989023,November 23,1999.
[44]Foster PS.Use of the Calmset 3 biofeedback/relaxation system in the assessmentand treatmentofchronic nocturnal bruxism.Appl Psychophysiol Biofeedback 2004;29(2): 141-147.
✉Corresponding author:Prof.Feimin Zhang,Jiangsu Key Laboratory of Oral Diseases,Nanjing Medical University;Department of Prosthodontics,Affiliated Hospital of Stomatology,Nanjing Medical University,136 Hanzhong Road,Nanjing,Jiangsu 210029,China,
Tel:+86-25-85031831,E-mail:fmzhang@njmu.edu.cn.
Received 26 September 2013,Revised 25 March 2014,Accepted 28 May 2014,Epub 18 November 2014
The authors reported no conflicts of interest.
©2015 by the Journal of Biomedical Research.All rights reserved.
10.7555/JBR.28.20130145
 THE JOURNAL OF BIOMEDICAL RESEARCH2015年2期
THE JOURNAL OF BIOMEDICAL RESEARCH2015年2期
- THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Recent advances in bariatric/metabolic surgery:appraisalof clinical evidence
- Metabolic bariatric surgery and type 2 diabetes mellitus:an endocrinologistˊs perspective
- Roux-en-Y gastric bypass for Chinese type 2 diabetes mellitus patients with a BMI<28 kg/m2:a multi-institutionalstudy
- Bariatric surgery in old age:a comparative study of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy in an Asia centre ofexcellence
- Maternalinheritance of severe hypertriglyceridemia impairs glucose metabolism in offspring
- Osthole inhibits proliferation of human breast cancer cells by inducing cell cycle arrest and apoptosis
