Roux-en-Y gastric bypass for Chinese type 2 diabetes mellitus patients with a BMI<28 kg/m2:a multi-institutionalstudy
Hui Liang,Wei Guan,Yanling Yang,Zhongqi Mao,Yijun Mei,Huan Liu,Yi Miao
1DepartmentofGeneral Surgery,The First Affiliated Hospital,Nanjing Medical University,Nanjing,Jiangsu 210029,China;
2Department of General Surgery,Xijing Hospital,The Fourth Military Medical University,Xiˊan,Shaanxi 710032,China;
3Department of General Surgery,The First Affiliated Hospital,Suzhou University,Suzhou,Jiangsu 215006,China;
4Departmentof General Surgery,The Sixth Affiliated Hospital,Wenzhou Medical University,Lishui,Jiangsu 323000,China.
Roux-en-Y gastric bypass for Chinese type 2 diabetes mellitus patients with a BMI<28 kg/m2:a multi-institutionalstudy
Hui Liang1,△,✉,Wei Guan1,△,Yanling Yang2,Zhongqi Mao3,Yijun Mei4,Huan Liu1,Yi Miao1
1DepartmentofGeneral Surgery,The First Affiliated Hospital,Nanjing Medical University,Nanjing,Jiangsu 210029,China;
2Department of General Surgery,Xijing Hospital,The Fourth Military Medical University,Xiˊan,Shaanxi 710032,China;
3Department of General Surgery,The First Affiliated Hospital,Suzhou University,Suzhou,Jiangsu 215006,China;
4Departmentof General Surgery,The Sixth Affiliated Hospital,Wenzhou Medical University,Lishui,Jiangsu 323000,China.
Roux-en-Y gastric bypass surgery(RYGB)has been demonstrated to be successfulfor treating type-IIdiabetes mellitus(T2DM)patients with a body mass index(BMI)<30 kg/m2,butreports of RYGB for T2DMpatients with a BMI<28 kg/m2are lacking.T2DM patients with a BMI<28 kg/m2were prospectively recruited to participate in this study in four hospitals.The endpoint was T2DM remission(defined by fasting blood glucose(FBG)level<110 mg/dL and hemoglobin(Hb)A1c level<6.0%at12 months postoperatively).Predictors of remission were investigated by univariate and multivariate analyses.Eighty-six patients were assessed.Eighty-five patients underwent RYGB,with one conversion to open surgery.We compared the values of various variables before and after surgery.The mean BMI decreased from 24.68±2.12 to 21.72±2.43 kg/m2(P<0.001).Fifty-eight(67.4%)patients were not treated by drugs or insulin after surgery,and 20 patients(23.3%)had complete remission of T2DM at 12 months after surgery with an acceptable number of complications.The mean HbA1c level in the remission group was significantly lower than that in the non-remission group.Patients with a higher weight,lower HbA1c level,higher C-peptide level,and higher FBG level were more likely to have T2DM remission in multivariate analyses.In conclusion,RYGB was effective and safe for treating T2DM patients with a BMI<28 kg/m2. Complete remission can be predicted by cases having a higher weight,lower HbA1c level,higher C-peptide level, and higher FBG level.
Roux-en-Y gastric bypass,type 2 diabetes mellitus,HbA1c,C-peptide,body mass index,metabolic surgery
Introduction
Type 2 diabetes mellitus(T2DM)is worldwide problem.The number of individuals with T2DM is predicted to increase to 439 million by 2030[1,2].T2DM is associated with increased morbidity and mortality[3]. Controlof T2DM by diet,behavior modification and drug treatment is difficult[4-7].The mean body mass index(BMI)of T2DM patients in China is only 24 kg/m2and glucose controlis notideal[5].
In obese patients,bariatric surgery has been shown to be successful for the treatment of obesity and T2DM[8-12].Importantly,gastrointestinal(GI)metabolic surgery is accepted as effective treatment for T2DMpatients with a BMI<35 kg/m2[3,7,13].Furthermore,GI metabolic surgery hasbeen demonstrated to be successful in the treatment of T2DM patients with a BMI<30 kg/m2[14].
Studies[7,9,10,14-16]have suggested that preoperative patientfactors such as age,duration of T2DM,control ofglycated hemoglobin(HbA1c)level,fasting levelof C-peptide,and the BMIare associated with improved glycemic outcomes.However,the resultsofsuch studies were from obese patients.Dixon and colleagues[14]reported thatweightand weightlosshave majorinfluences on the outcomes of gastric bypass surgery in T2DM patients with a BMI<30 kg/m2.
Roux-en-Y gastric bypass surgery(RYGB)is the surgicalprocedure most often used for gastric bypass surgery.RYGB can provide significantand sustained weight loss[11,17-20].RYGB for the treatment of T2DM patients with a BMI<28 kg/m2has notbeen reported.
The primary aim ofthe presentstudy wasto determine the efficacy and safety of RYGB for the treatmentof T2DM patients with a BMI<28 kg/m2.The second aim was to investigate the predictors of remission of T2DM in a Chinese population.
Patients and methods
Ethical approval of the study protocol
The study protocol was approved by the Ethics Committee of each of the four participating hospitals and complied with the Helsinki Declaration.Allparticipants provided written informed consent to be included in the study.
Patients
Between June 2009 and June 2012,patients were recruited to participate in this study from fourhospitals prospectively if they metfour criteria:(i)absence of well-controlled T2DMafter6 monthsofmedicaltreatment; (ii)BMI≤28 kg/m2;(iii)aged 18-75 years;(iv)acceptance of the risks associated with RYGB.The diagnosis of T2DM was based on the criteria setby the American Diabetes Association and was considered to be valid if established by an endocrinologistordiabetes specialist. The exclusion criteria were:(i)patients who had undergone GI surgery previously;(ii)pregnancy;(iii)latent autoimmune diabetes.
Preoperatively,patients were assessed by a specialized team(surgeon,endocrinologist,anesthetist,psychiatrist, and dietician).All patients underwent a routine preoperative work-up and counseling in addition to a detailed diabetic work-up.Follow-up visits were scheduled at1 week as wellas 1,3,6,9,and 12 months after surgery.Postoperative data collected included levels of fasting plasma glucose(FPG),fasting C-peptide and HbA1c,medication use,and the BMI.
RYGB
RYGB wasundertaken by surgeons with>10 yearsˊ experience of GIsurgery in allfour institutions.The RYGB procedure comprised creation of a subcardial gastric pouch(15-30 mL),a biliopancreatic limb length of 100 cm,and a Roux limb length of 100 cm with a 20-mm gastrojejunostomy.The gastrojejunostomy was performed using linearstaplers and a hand-sewn closure ofthe enterotomy.The mesenteric and Petersen defects were closed.
Remission of T2DM
Remission of T2DM was defined as a FPG<110 mg/dL and Hb A1c<6.0%without the use of anti-diabetic medication 12 months after surgery.The patientˊs condition was considered to have improved if the FPG level decreased by>25 mg/d L or the HbA1c levelfellby>1%.Surgery was considered to have been unsuccessfulif glycemic indices showed no significant improvement or became worsened,or if additionalanti-diabetic medication was required.
Statistical analyses
Percentiles,the median,the mean±standard deviation(SD),and range were analyzed foreach continuous variable.Patients were divided into two subgroups for univariate analyses:patients with T2DM remission and patients without T2DM remission.Candidate variables in univariate analyses were:sex,age,weight,BMI, levelof FBG,2-h postprandialblood sugar(2-h PPBS), C-peptide and HbA1c,as well as duration of T2DM. Differences between the two groups with regard to the variables stated above were examined using the unpaired t-testforcontinuous variables and the chi-square test for unordered categorical variables.Multivariate logistic analyses were conducted to determine factors associated with T2DM remission.All P-values were two-tailed with 5%significance levels.All statistical analyses were undertaken using STATA v10.0(Computer Resource Center,Chicago,IL,USA).
Results
Patient characteristics
Overall,86 patients(46 females)with a BMI<28 kg/m2were recruited and RYGB was undertaken in all.Of these 86 patients,80 patients completed the 12-month follow-up and six patients were lost to follow-up.These six patients were excluded from thedata analysis.The median duration of T2DM was 7 (range,0.5-17)years.The mean age of the patients was 48.52(range,22-72)years.The mean BMIwas 24.68(range,18.69-27.99)kg/m2.
Complications of surgery
Ofthese 80 T2DMpatients,no mortalities orserious complications(obstruction,requirementof reoperation) were noted.Conversion to open surgery was required for one patientbecause of injury to mesenteric blood vessels.Hemorrhage ofthe upperdigestive tractoccurred in two patients and both were treated successfully by conservative means.One patientdied of gastric cancer 15 months after RYGB.No other complications were observed.Anemia was documented in 7(8.75%) patients,and alopecia in 6(7.5%)cases.
Efficacy of surgery
Eighty patients completed 12-month follow-up. Hence,various parameters measured before surgery and at the 12-month follow-up were compared.For instance,the mean insulin level decreased from 15.03±13.91 UI/mL before surgery to 12.97±6.65 UI/ mL at12 months aftersurgery,and this difference was notsignificant(P=0.234).The mean C-peptide level increased from 1.38±0.72 ng/mL to 1.56±0.64 ng/ mL,and this difference was marginally significantly different(P=0.086).The mean FBG decreased signific a n tly fro m 1 7 7.8 4±8 1.3 6 m g/d L to 118.44±22.32 mg/dL(P<0.001),and the 2-h PPBS decreased significantly from 334.62±111.78 mg/dL to 163.80±48.96 mg/dL(P<0.001).
The mean BMIdecreased from 24.68±2.12 kg/m2to 21.72±2.43 kg/m2(P<0.001),and the mean HbA1c decreased from 8.59±2.08%to 6.52±1.06% (P<0.001).Of 80 patients,58 patients(72.5%)were not treated by drugs or insulin after surgery,and 20 patients(25%)had complete remission of T2DM at 12 months after surgery with an acceptable number of complications.Only three patients(3.75%)had an HbA1c level<6%preoperatively,and an HbA1c level<6%was observed in 22 patients(27.5%)at 12 months after surgery.Additional 55 patients (68.75%)were not treated by drugs or insulin after surgery,improved their controlof T2DM,and underwentsurgery successfully.
Factors associated with remission of T2DM
Preoperative factors in patients with and without T2DM remission were assessed(Table 1).The sex distribution between the two groups was not significantly different(P=0.126),nor was mean age(P= 0.627).Interestingly,the mean weightin the remission group was higher although the difference was only marginally significant(P=0.065).The mean HbA1c level in the remission group was significantly lower than that in the non-remission group(7.81 vs. 8.89;P=0.045).There was no significantdifference between the two groups with regard to the BMI,FBG level,2-h PPBS,C-peptide level,or T2DM duration (all P>0.05).
Multivariate analyses were applied to investigate the factors associated with T2DM remission(Table 2). Similar to univariate analyses,patients with higher weights were more likely to have T2DM remission (75.1-90 Kg vs.≤60 Kg;odds ratio(OR),2.70; 95%confidence interval(CI),1.27-6.72).Compared with patients with a HbA1c level≤7%before surgery, patients with a HbA1c level≤9%(OR,0.03;95%CI, 0.00-0.26)and>9%(OR,0.11;95%CI,0.01-0.88) were less likely to have T2DMremission.Patients with a higher C-peptide level were more likely to have T2DM remission than patients with a lower C-peptide levelbefore surgery(>2.0 ng/ml vs.≤1 ng/ml;OR, 1.70;95%CI,1.04-2.76).Patients with a higher FBG levelwere more likely to have T2DM remission than patients with a lower FBG level before surgery (>126 mmol/l vs.<126 mmol/l;OR,3.71;95%CI,2.1 0-6.56).Other factors associated with T2DM remission were notfound in multivariate analyses.
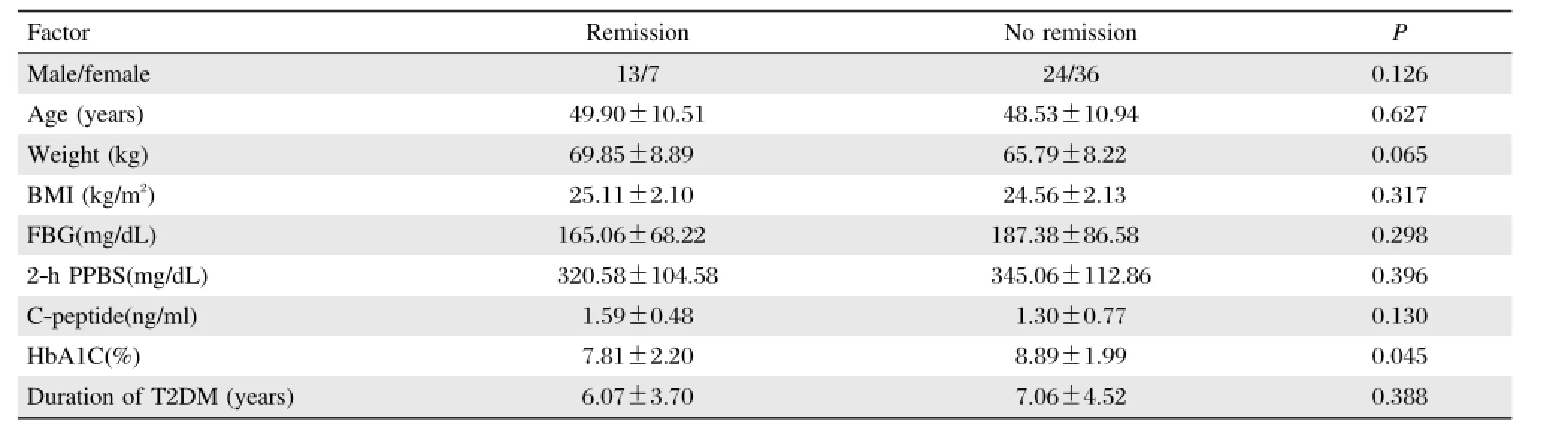
Table 1 Univariate analysis of preoperative factors in patients with and without T2DM remission
Discussion
Buchwald et al.[17]suggested that of all 22,094 patients who underwentbariatric surgery,T2DM was resolved completely in 76.8%of patients and resolved or improved in 86.0%of cases.However,the patients included in that review were diagnosed with obesity with a BMI>35 kg/m2.RYGB is known to achieve sustainable resolution of T2DM in obese subjects. RYGB has been accepted to be effective treatment for T2DM patients with a BMI<35 kg/m2in a few studies[3,7,13,14],but the results were based on short-term follow-up and a BMI>25 kg/m2.The mean BMI of patients with T2DM in China is approximately 24 kg/m2.Therefore,determining the efficacy and safety of GI metabolic surgery for the treatment of T2DM patients with a BMI<28 kg/m2is important.
We found that58 patients were nottreated by drugs or insulin after surgery.Of the 86 patients,20 patients had complete remission of T2DM at 12 months after surgery with an acceptable number of complications. All patients showed improvement or remission with regard to glycemic control.Patientswith higherweights, lower HbA1c level,higher C-peptide level,and higher FBG levelwere more likely to have T2DM remission.
Dixon etal.[14]reported thatexcellentglycemic control was achieved in 31(30%)T2DM patients with a BMI<30 kg/m2at 12 months.A Korean study of 403 patients with T2DM and mean BMI of 24.7 kg/ m2found thatremission occurred in 15%ofpatients[21]. Huang etal.reported that14(63.6%)patients with a BMI of 25-35 kg/m2showed T2DM remission when treated by RYGB[22].We found that25.0%of patients had complete remission of T2DM at 12 months after surgery.Therefore,RYGB for the treatment of T2DM patients with a BMI<28 kg/m2was effective.
The safety of RYGB in the treatment of T2DM patients with a BMI<28 kg/m2is also important. Changes in the BMIat12 months in comparison with the mean preoperative BMI value were significant. Nevertheless,BMI values remained within the normalrange.Some studies focusing on RYGB undertaken on patientswith low BMIvalues corroborate the finding of a less dramatic postoperative change in the BMI[14,22]. The reason why patient weights did not continue to decrease is notclear.Scopinaro etal.postulated thata homeostatic mechanism permits weightloss relative to the amountofcalories,for which the procedure facilitates the absorption ofcalories.Furthermore,a‘‘blunting’’of weight loss is observed[23].
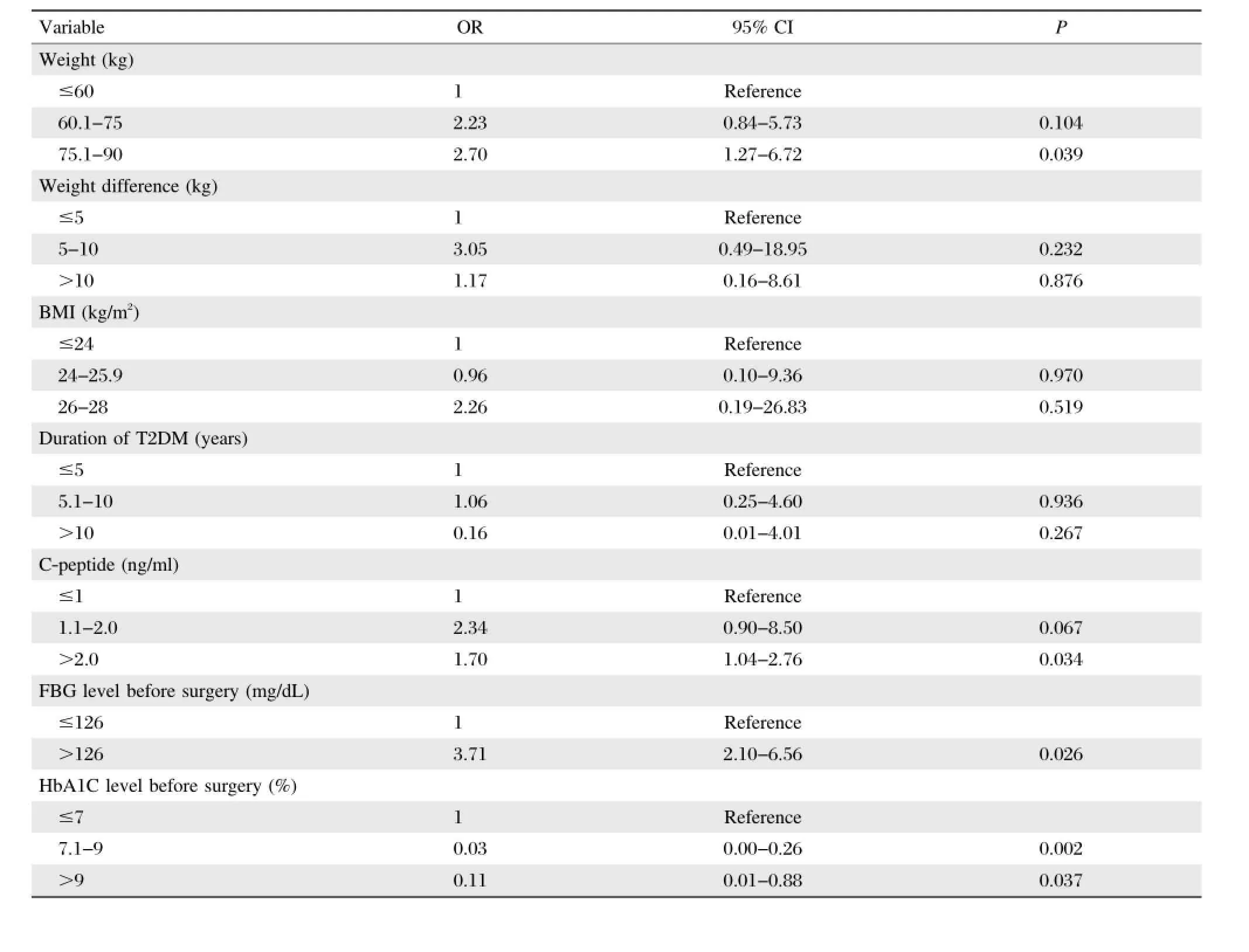
Table 2 Multivariate analyses of preoperative factors in patients with and without T2DM remission
We found thatanemia occurred in 7(8.75%)patients and alopecia in 6(7.5%)individuals.After dietmodification and nutrient supplementation,anemia and alopecia were cured.No malnutrition occurred in our 80 patients.Furthermore,the prevalence of complications aftersurgery was low and,in general,acceptable. Our prospective multi-institutional study suggested that RYGB in the treatmentof T2DM patients with a BMI<28 kg/m2was safe.
Univariate and multivariate analyses were applied to investigate the predictors of T2DM remission.Patients with higher weights,lower HbA1c levels,higher C-peptide levels,and higher FBG levels were more likely to have T2DM remission.Studies have suggested that a higher BMIis associated with a higherprevalence of T2DM remission[14,17].In the present study,the BMI was not significantly associated with the prevalence of T2DM remission,and while preoperative weight was significantly associated with the prevalence of T2DMremission,the weightloss was not.This finding confirms thatnormalization of glycemic indices is not related to weight loss.Dixon and colleagues showed thatweightloss has a major influence on outcomes[14]. In the present study,levels of C-peptide and Hb A1c were found to be associated with the prevalence of remission.C-peptide isa reflection ofbeta-cellfunction. The mean C-peptide value increased marginally after surgery,but a higher C-peptide level was associated with a higherprevalence ofremission.In patients with a BMI<28 kg/m2,the C-peptide levelwasan important predictor.Furthermore,a lower levelof Hb A1c was associated with a higher prevalence of remission.We suggestthatdrug controlof T2DM before surgery may be important.
Our results are encouraging,butthe prevalence of remission in patients with a BMI<28 kg/m2is lower than that in obese patients.However,an additional 55 patients(64.0%)were nottreated by drugs orinsulin after surgery.In view of our findings,preoperative weight and levels of HbA1c,C-peptide and FBG are importantfactorsforpatientselection when considering surgical treatment for T2DM patients with a BMI<28 kg/m2.
The present study had three main limitations.First, the follow-up duration was shortand long-term results are needed to confirm our findings.Second,although thisprospective study wasmulti-institutional,the sample size in the fourcenters was notidentical.Third,differences of habits and customs in the four regions in which the patients were recruited were notassessed.
In conclusion,our prospective study showed that RYGB for T2DM patients with a BMI<28 kg/m2is efficacious,safe and associated with low early morbidity.A totalof25.0%ofpatients with a BMI<28 kg/m2had complete remission of T2DM at 12 months after RYGB with an acceptable number of complications. Complete remission was predicted by higher weight, lower HbA1c level,higher C-peptide level,and higher FBG level.Our findings are interesting,but future studies with a larger sample size(especially in an Asian population)are needed to confirm them.
[1]Shaw JE,Sicree RA,Zimmet PZ.Global estimates of the prevalence of diabetes for 2010 and 2030.Diabetes Res Clin Pract 2010;87(1):4-14.
[2]Carlsson LM,Peltonen M,Ahlin S,etal.Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects.N Engl J Med 2012;367(8):695-704.
[3]Zimmet P,Alberti KG,Shaw J.Global and societal implications of the diabetes epidemic.Nature 2001; 414(6865):782-787.
[4]The relationship ofglycemic exposure(HbA1c)to the risk of developmentand progression of retinopathy in the diabetes control and complications trial.Diabetes 1995; 44(8):968-983.
[5]Xu Y,Wang L,He J,etal.Prevalence and controlof diabetes in Chinese adults.JAMA 2013;310(9):948-959.
[6]Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes(UKPDS 34).UK Prospective Diabetes Study (UKPDS)Group.Lancet 1998;352(9131):854-865.
[7]Lee WJ,Hur KY,Lakadawala M,et al.Gastrointestinal metabolic surgery for the treatment of diabetic patients: a multi-institutional international study.J Gastrointest Surg 2012;16(1):45-51;discussion 51-42.
[8]Pories WJ,Swanson MS,MacDonald KG,et al.Who would have thought it?An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 1995;222(3):339-350;discussion 350-332.
[9]Dixon JB,OˊBrien PE.Health outcomes ofseverely obese type 2 diabetic subjects 1 year after laparoscopic adjustable gastric banding.Diabetes Care 2002:25(2);358-363.
[10]Schauer PR,Burguera B,Ikramuddin S,et al.Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus.Ann Surg 2003:238(4);467-484;discussion 484-465.
[11]Sjostrom L,Lindroos AK,Peltonen M,et al.Lifestyle, diabetes,and cardiovascularrisk factors 10 years after bariatric surgery.N Engl J Med 2004:351(26);2683-2693.
[12]Vidal J,Ibarzabal A,Romero F,et al.Type 2 diabetes mellitus and the metabolic syndrome following sleeve gastrectomy in severely obese subjects.Obes Surg 2008: 18(9);1077-1082.
[13]Rubino F,Kaplan LM,Schauer PR,et al.The Diabetes Surgery Summit consensus conference:recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus.Ann Surg 2010:251(3); 399-405.
[14]Dixon JB,Hur KY,Lee WJ,etal.Gastric bypass in Type 2 diabetes with BMI<30:weightand weightloss have a major influence on outcomes.Diabet Med 2013:30(4); e127-134.
[15]Hall TC,Pellen MG,Sedman PC,etal.Preoperative factors predicting remission of type 2 diabetes mellitus after Roux-en-Y gastric bypass surgery for obesity.Obes Surg 2010:20(9);1245-1250.
[16]Lee WJ,Chong K,Ser KH,et al.C-peptide predicts the remission of type 2 diabetes after bariatric surgery.Obes Surg 2012:22(2);293-298.
[17]Buchwald H,Avidor Y,Braunwald E,etal.Bariatric surgery:a systematic review and meta-analysis.JAMA 2004:292(14);1724-1737.
[18]Werling M,Fandriks L,Bjorklund P,et al.Long-term results of a randomized clinical trial comparing Rouxen-Y gastric bypass with vertical banded gastroplasty. Br J Surg 2013:100(2);222-230.
[19]Reed MA,Pories WJ,Chapman W,etal.Roux-en-Ygastric bypass corrects hyperinsulinemia implications for the remission of type 2 diabetes.J Clin Endocrinol Metab 2011:96(8);2525-2531.
[20]Sovik TT,Taha O,Aasheim ET,et al.Randomized clinical trialof laparoscopic gastric bypass versus laparoscopic duodenalswitch forsuperobesity.Br J Surg 2010:97(2);160-166.
[21]Kim JW,Cheong JH,Hyung WJ,et al.Outcome after gastrectomy in gastric cancer patients with type 2 diabetes.World J Gastroenterol 2012:18(1);49-54.
[22]Huang CK,Shabbir A,Lo CH,et al.Laparoscopic Rouxen-Y gastric bypass for the treatment of type II diabetes mellitus in Chinese patients with body mass index of 25-35.Obes Surg 2011:21(9);1344-1349.
[23]Scopinaro N,Papadia F,Marinari G,et al.Long-term control of type 2 diabetes mellitus and the other major components of the metabolic syndrome after biliopancreatic diversion in patients with BMI<35 kg/m2.Obes Surg 2007:17(2);185-192.
△Hui Liang and Wei Guan contributed equally to this work.
✉Corresponding author:Prof.Hui Liang,Department of General Surgery,The First Affiliated Hospital with Nanjing Medical University,300 Guangzhou Road,Nanjing,Jiangsu 210029,China.Tel:
86-25-68302120,E-mail:drhuiliang@hotmail.com.
Received 19 July 2014,Revised 26 September 2014,Accepted 29 December 2014,Epub 25 January 2015
The authors reported no conflict of interests.
©2015 by the Journal of Biomedical Research.All rights reserved.
10.7555/JBR.29.20140109
 THE JOURNAL OF BIOMEDICAL RESEARCH2015年2期
THE JOURNAL OF BIOMEDICAL RESEARCH2015年2期
- THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Recent advances in bariatric/metabolic surgery:appraisalof clinical evidence
- Metabolic bariatric surgery and type 2 diabetes mellitus:an endocrinologistˊs perspective
- Bariatric surgery in old age:a comparative study of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy in an Asia centre ofexcellence
- Maternalinheritance of severe hypertriglyceridemia impairs glucose metabolism in offspring
- Osthole inhibits proliferation of human breast cancer cells by inducing cell cycle arrest and apoptosis
- Quercetin attenuates the development of 7,12-dimethylbenz(a) anthracene(DMBA)and croton oil-induced skin cancer in mice
