The Community Hub: a proposal to change the role of Residential Aged Care Facilities (RACFs)
Ian Maddocks
The Community Hub: a proposal to change the role of Residential Aged Care Facilities (RACFs)
Ian Maddocks
Introduction
In Australia, as in most parts of the world, the increasing number of aged persons and the proportion of the population represented by aged persons is a cause of concern that will require changes in many areas of community life, including aged care [1]. This paper draws on Australia’s experience to propose a new model for residential aged care with potential international application.
The health care needs of the aged are also changing everywhere. More aged persons have chronic diseases needing regular supervision and management, and there are more aged persons with dementia. We must anticipate elderly populations seeking more health care at a time when families and authorities are less able to afford health care [2].
These Barriers Limit Effective Aged Care
1. Attitudinal Barriers
a)Attitudes in Bureaucracies
Residential aged care in Australia is heavily regulated, regimented, and change is generally imposed through compliance-based legislation demanding considerable paper work, which limits staff satisfaction and time with patients.
b)Community Attitudes
The common stereotype of older people is associated with decline, dependency, and dementia. Residential Aged Care Facilities (RACFs) suffer a poor reputation, and the prospect of placement in a RACF f lls many older people with dread [3].
c)Staff AttitudesThe culture of the RACF focuses on disease and the maintenance of comfort, which encourages resident inactivity and both physical and social decline. A pervasive concern about ‘duty of care’ induces an anxiety to avoid responsibility and mistakes. Staff-to-patient ratios are low, work must be rushed, and residents have to adapt to set times for hygiene, meals, and sleep, which are a cause for dissatisfaction amongst residents and family members. More emphasis on activity and encouragement for patients to fend for themselves reduces the number needing major assistance and compresses the stage of decline that precedes death, thus allowing more time to attend to individual needs [4].
2. Structural Barriers
RACFs are a complex mix; specif -cally, RACFs are large and small, public and private, and for-prof t and not-for-prof t. The multiple agenciesinvolved embody a wide variety of histories, values, managements, and associations. Common to most is a relative isolation from the communities in which they are located.
Ways of incorporating RACFs into the community around them will be particularly important if more aged persons are to be managed in homes. The RACFs need to be in a position to offer support for local home care, with respite opportunities, particularly for dementia care [4]. If the RACFs offer clinical supervision of home care, symptom crises can also be managed in the home, avoiding transfers to acute hospital care.
3. Staff ng Barriers
a)MedicalMany primary care practitioners (commonly called general practitioners [GPs] in Australia) are reluctant to undertake visits to homes or RACFs, regarding fees for such consultations as inadequate. Increasingly, locum services provide medical advice in those areas, with the attendant risk of inappropriate overprescribing, and unnecessary hospital admission for acute illness episodes [5–7].
Lack of medical interest in aged care partly ref ects a lack of training. A comprehensive preparation in psycho-geriatrics, chronic disease, and palliative care is needed, but has not been part of existing medical curricula.
b)Nursing
Funding for RACFs means that the sometimes solitary registered nurse f nds that much time is taken up with completion of administrative duties and paper work. Enrolled nurses commonly supervise medications and provide support for the less-qualif ed carers who are the major work force.
c)Caretakers
RACF caretaker staff ng increasingly relies on relatively young persons recruited from overseas and trained in a short intensive program after arrival. There are communication diff culties and cultural misunderstandings. Many hope for further education and alternative employment opportunities.
The caretakers have not done this kind of work before, many having relied on servants at home [8].
Most elderly persons wish for care in their own home. This places signif cant demands on those who provide care in the home. The elderly persons need regular support from visiting physicians, nurse practitioners, other health workers, and volunteers, plus access to respite care.
d)Other Staff
The many discomforts of very elderly persons benef t from the available support of allied health expertise, including psychology, podiatry, dietetics, speech pathology, physiotherapy, pharmacy, occupational therapy, speech therapy, and social work. These services need to be accessible both to RACF residents and those receiving care at home.
4. Clinical Management Barriers
RACF staff often feel that support is inadequate and they are overburdened by responsibility. Transfer of RACF residents to acute hospital care is a common response to any signif cant acute clinical need if only a locum service, unfamiliar with the case in question, is available. This creates an issue for emergency departments whose staff see the arrival of an aged person with a sometime minor deterioration in health status as a distraction from their main work [9, 10].
Hospitalization encourages unnecessary investigation, futile treatment, and not infrequently, deterioration and death of an elderly person in an unfamiliar and inappropriate environment [11].
AN ALTERNATIVE MODEL
The Community Aged Care Hubis proposed as a development of the RACF that will offer coordination and management of all matters affecting the health and well-being of elderly persons at the community level. The Community Hub would continue to provide comprehensive aged care for its RACF residents, but also participate in social support, preventive care, dementia care, and palliative care for aged persons in the homes of the local community (Figure 1).
Components of Community Aged Care Hub
1. Improved Medical Supervision and Support A primary care practice on-site, with medical staff trained in aged care, psycho-geriatrics, and palliative care provides in-house clinical leadership while continuing to offer care in the local community.
On admission, each resident receives, in consultation with family members, a comprehensive assessment embracing a full medical and social history, risk assessment, medication review, and the preparation of an advance directive document [12, 13]. This routine will reduce unnecessary hospital transfers. Hospital-type treatment in RACFs is a viable alternative for many hospital transfers if regular medical review of residents and better on-site management of the complex, multiple medical needs of aged persons is available [14, 15].
2. A New Positive Culture of Healthy Ageing
Aged individuals will be encouraged by the Hub to take a more informed and positive ownership of their own health. Staff at all levels will aff rm ownership of the same positive approach to their own health. Emphasis on graded exercises, improved nutrition, and more interaction in social settings will reduce the need for staff intervention in matters of mobility, hygiene, and feeding. A gymnasium, staffed by a personal trainer, can make an enormous contribution and be relevant to all but the most dependent residents [4].
Flexibility in management should allow trials of innovative practices in clinical care, staff deployment, and opportunity to offer admissions from local homes for respite or emergency situations rather than transfer to emergency or acute hospital care.
Medical leadership, based in-house, will bring a new conf dence to staff, a heightened morale as they engage with the new paradigm of healthy ageing and conf dence in the available back-up and skilled review. Allied health services available on a fulltime or sessional basis will enhance the cultural shift required.
The medical presence will be augmented by nurse practitioners with expertise in psycho-geriatrics and palliative care. The nurse practitioners will support care in the RACF and those community health care staff visiting local homes (GPs, district nurses, caregivers, and family members). The nurse practitioners will undertake in-service education and support of caregivers and volunteer helpers, help devise imaginative and proactive care routines, and facilitate an increased opportunity for death being managed in the home.
3. A Better-Trained Workforce Medical graduates taking up work in a Community Hub need conf dence in geriatrics, psycho-geriatrics, and palliative care. A wide-ranging program that embraces all three areas at the diploma level should be open to graduates in all health disciplines, not just medicine, and would attract graduates in nursing, psychology, social work, physiotherapy, and pharmacy. Such a diploma, whether offered through a college or university, will be available by distance study.
GPs or staff from other health disciplines who complete the diploma need recognition as elderly care practitioners, equipped to undertake leadership and teaching roles in aged care situations.
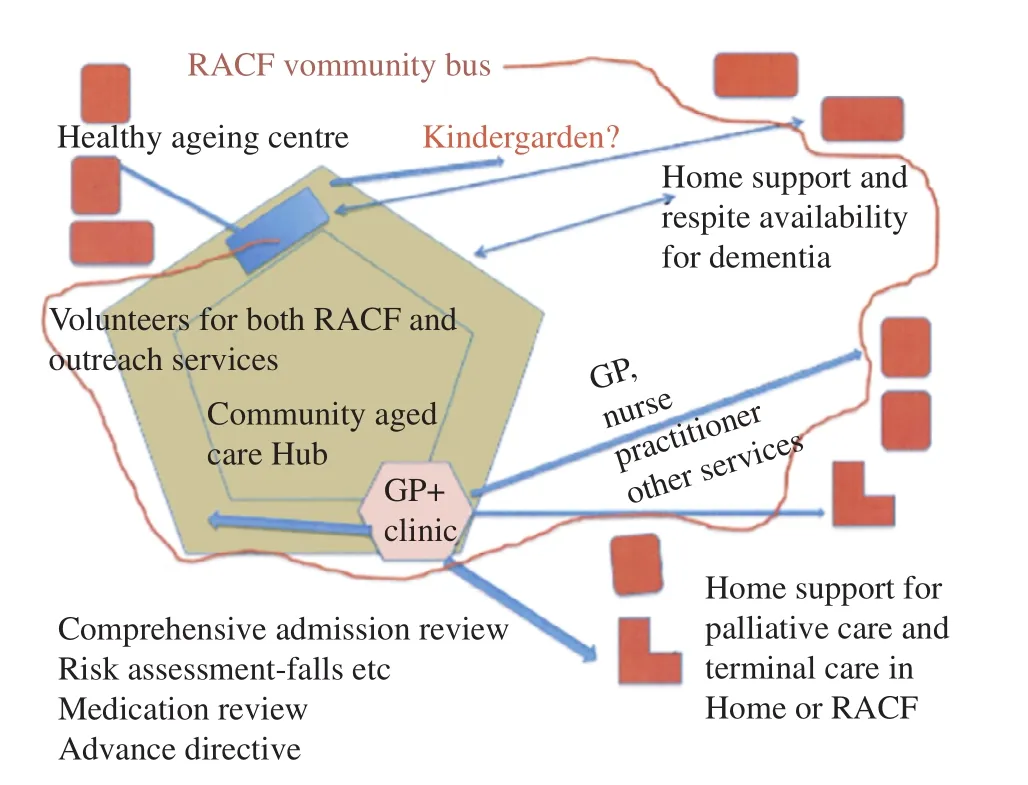
Figure 1. Map/diagram of the proposed components of the Community Aged Care Hub.
4. A Centre for Education and Training
Forming close links to tertiary and technical training institutions, the Hub will offer on-site undergraduate and post-graduate placements for students of aged care in all disciplines, learning through participation in care delivery, case-studies, tutorials, and discussions. When undergraduates meet the realities of aged care through encounters with feisty elderly RACF residents and others in home placements, they f nd a new interest in aged care as a career opportunity [16].
5. Integration into the Local Community The Aged Care Community Hub will become a part of the local community by providing services into local homes and bringing community members into the facilities.
Home visits will make the local aged familiar with the RACF and its staff, and comfortable to accept admission there when necessary. IT services, linking homes and the Hub, can expand the range of clinical contact, particularly when both parties already know one another.
Relevant RACT services may include the following:
Club facilities for aged personsliving in the local community will encourage mobility, strength, and intellect through regular use of the gymnasium, exercise classes, games (bridge and billiards) and discussion groups (e.g., book club and lecture series).
A community bus serviceto undertake regular pick-up and set-down runs for access to the Hub by home-based patients and Club participants.
General social supportwith a midday hot meal for elderly persons from the local community, plus an opportunity to have laundry done, or a regular assisted shower can be considered. These services will supplement home-visiting services, such as district nurses, visiting meal services, or home care clinical packages.
A Volunteer Organizationwill provide encouragement and support of in-house and Club activities. Volunteers have a special role in befriending elderly persons who have limited family contact. The volunteers can allay, with a quiet presence, the agitation and confusion to which many elderly are prone, and help in the vexed issue of over-medication with psycho-active drugs for resident restraint [17].
A vibrant facility, busy with community activity, would encourage the involvement of the recently retired as helpers for older aged in-house or in homes, and assist their own healthy ageing. Training and encouragement programs for this essential corps of Hub supporters will involve members of the multidisciplinary team and require the employment of a volunteer coordinator.
A kindergardenon-site would be a bonus, bringing into the lives of the residents some of the sense of extended family which used to be the setting for aged care, but which has largely disappeared in modern urban societies. Young mothers, whose own parents may face the prospect of old age with trepidation, will become more attuned to the realities and the opportunities of old age. Their small children may f nd, in both the affection demonstrated by the elderly residents and the stories they can tell, an awareness of age that they might otherwise miss.
Co-Location of Hub Elements is not as Important as Cooperation/Collaboration
The many suggested components for a Community Hub will not easily be added to existing RACFs, though new facilities might consider combining the facilities on one campus. A consortium of RACFs, building a Community Hub by sharing facilities across a region (one having a gym, one a pool, and one a special interest in palliative care) can allow progress to begin. Already, one or more of the changes suggested are being introduced in particular RACFs in Australia. A steady development towards a fuller comprehensive vision will usually have to happen step-by-step, and will require broader encouragement to direct its development.
Establishing Community Hubs
In each country there will be a wide range of existing stakeholders with potential to take up this vision, including government departments, not-for-prof t and for-prof t organizations managing RACFs, professional organizations, universities, community authorities, and volunteer bodies.
式中:F为综合评分;F1、F2和F3为主成分1、2和3的得分;Y1、Y2、Y3为主成分的特征值;C为累积特征值。
Primary care physicianswill need to see an advantage for their future careers in taking up the concept of the Hub and preparing through further education to be part of an exciting development in aged care.
Community health organizationsmight undertake a coordinating role in the further local development of the proposal.
Government Agencies
All levels of government should recognize the advantage of a model that brings comprehensive aged health care and social welfare support close together in location and management. There are major opportunities for better care and cost savings, for example through the closure of expensive acute hospital beds as RACFs undertake more hospital-type care.
A f nancial subsidy to GPs who undertake supervision of palliative care in the home has been shown to lead to a far higher proportion of home deaths with further reduction in acute hospital costs.
The central role of the Hub in the health of their communities and should encourage local government authorities to supplement services for its elderly citizens.
Educational Institutions
Caregiver skills will be enhanced if placement experience at a Hub is incorporated in whatever training is offered to carers.
There is an opportunity for private providers to be involved in developing more comprehensive curricula for other professional or lay caregivers geared to different levels of involvement.
RACFs
Organizations or authorities that manage RACFs need to see the advantages for their residents and staff in the proposed cultural change and closer links with community care. For a RACF to transform into a Community Aged Care Hub offers every probability of becoming engaged with something far more exciting and prof table in every sense than current models of residential aged care.
Design Considerations
Existing RACFs will be constrained by the RACFs already in place; specif cally, there will be limited space for expansion, and often only a partial transformation to a Hub will be possible. Incremental steps will be fostered through the consortium concept.
Where structural change can be effected, consideration can be given to matters as follows:
• future uncertainties of climate change, with the risk of higher temperatures and heat stress for elderly persons;
• medical and psychological reasons to incorporate fresh air and light in design; and
• appropriate design and furnishing of wards for dementia care, incorporating a color geography that assists residents to identify one area from another, and brightly-colored materials to life mood for staff and residents [18].
Funding Change
A substantial future increase in demand on health spending for aged care seems inevitable, but the introduction of the Community Hubs can lead to greater coordination of care and reduction in both duplication and bureaucratic oversight of existing services, thus reducing costs.
The pathway for establishing and funding Community Hubs will vary from country-to-country, and the relative place of government funding and private investment cannot be generalized, but the principles underlying the Hub concept have universal application.
ConclusionA new culture, a new spirit, a new community
A Community Hub offers a RACF and its community setting a vital spirit engendered among those who work in and support the Hub, and a new culture of caring, not only within the institution, but throughout the local community. As the Community Hub is widely recognized to improve the lives of elderly persons both within the RACF and at home in the community, individuals serving in that setting will be encouraged to consider their work as a privilege.
At the same time, some old-fashioned community responsibility for health costs might be anticipated, the kind that in the past supported a hospital that was ‘owned’ by the community. As the aged care facility in a community grows in local recognition and status, the aged care facility will attract greater local efforts to raise capital funds for new structures and equipment, or scholarships for further training, and interest in volunteering to be part of an enterprise of which the community is justif ably proud.
Conf ict of interest
The author declares no conf ict of interest.
1. Productivity Commission. Caring for Older Australians – Productivity Commission Inquiry Report, 08/2011.
2. Wysocki A, Butler M, Kane RL, Kane RA, Shippee T, Sainfort F. Long-term care for older adults: a review of home and community-based services versus institutional care. Comparative Effectiveness Reviews, No. 81. Minnesota Evidence-based Practice Center, November 2012.
3. These issues were raised at a consultation with the S.A. Older Women’s Advisory Committee on Saturday, March 29, 2014.
4. Boylan J. Putting theory into practice: an operational framework for healthy ageing. Residential Services Manager, Milpara and Highercombe RACFs, Hope Valley, SA., Mimeo, 2014.
5. Gadzhanova S, Reed R. Medical services provided by general practitioners in residential aged-care facilities in Australia. Med J Aust 2007;187:92–4.
6. Taylor MJ, Edvardsson D, Horey D, Featherstonhaugh D, Nay R, Swerissen H. General practitioner service provision in residential aged care facilities: 1998–2011. Australas J Ageing 2013;32:56–9.
7. O’Halloran J, Britt H, Valenti L. General practitioner consultations at residential aged-care facilities. Med J Aust 2007;187:88–91.
8. Goh Sok G. Palliative care physician, Adelaide. Personal Communication.
9. Jones S, Wallis P. Effectiveness of a geriatrician in the emergency department in facilitating safe admission prevention of older patients. Clin Med 2013;13:561–4.
10. Street M, Marriott JR, Livingston PM. Emergency department access targets and the older patient: a retrospective cohort study of emergency department presentations by people living in residential aged care facilities. Australas Emerg Nurs J 2012;15:211–8.
11. Elliott RA, Tran T, Taylor SE, Harvey PA, Belfrage MK, Jennings RJ, et al. Gaps in continuity of medication management during the transition from hospital to residential care: an observational study (MedGap Study). Australas J Ageing 2012;31:247–54.
12. Westbrook GA, Black D, Horden A. Comprehensive medical assessments for monitoring and improving the health of residents in aged care facilities: existing comprehensive medical assessments and a trial of a new service model. Australas J Ageing 2011;30:5–10.
13. Silvester W, Parslow RA, Lewis VJ, Fullam RS, Sjanta R, Jackson L, et al. Development and evaluation of an aged care specif c Advance Care Plan. BMJ Support Palliat Care 2013;3:188–95.
14. Arendts G, Reibel T, Codde J, Frankel J. Can transfers from residential aged care facilities to the emergency department be avoided through improved primary care services? Data from qualitative interviews. Australas J Ageing 2010;29:61–5.
15. Lau L, Chong CP, Lim WK. Hospital treatment in residential care facilities is a viable alternative to hospital admission for selected patients. Geriatr Gerontol Int 2013;13:378–83.
16. G-TRAC example of University of Adelaide initiative: gtrac@ adelaide.edu.au.
17. Rees G. CEO Alzheimers Australia. Personal Communication.
18. Mead R. The sense of an ending. New Yorker. May 2013; 92–103.
Ian Maddocks
AM, MD, FRACP, FAFPHM, FAChPM, DTM&H, Senior Australian of the Year, 2013, Emeritus Professor (Palliative Care), Flinders University of South Australia, Australia
E-mail: ian.maddocks@f inders. edu.au
9 November 2014;
Accepted 5 December 2014
——以PRETCO口试为例
 Family Medicine and Community Health2014年4期
Family Medicine and Community Health2014年4期
- Family Medicine and Community Health的其它文章
- A case-control study on family environment characteristics of accident-prone children
- Risk factors for post-operative delirium in elderly Chinese patients
- Analysis of the characteristics of coronary artery lesions in patients with obstructive sleep apnea-hypopnea syndrome and inf uencing factors
- Effect of core stability training on balance in elderly women
- Effects of psycho-scene-drama on empathic ability of patients with chronic schizophrenia
- Pre hospital medical services and paramedic engagement in Australian health care – Improving the pathways of care through collaborative action
