Risk factors for post-operative delirium in elderly Chinese patients
Xiaoli Yuan, Zhixia Jiang, Lingxia Song, Li Yang, Ying He, Gongyin Luo
Risk factors for post-operative delirium in elderly Chinese patients
Xiaoli Yuan, Zhixia Jiang, Lingxia Song, Li Yang, Ying He, Gongyin Luo
Objective:The purpose of this study was to systematically analyze the risk factors for postoperative delirium (PD) in elderly patients in an effort to provide a basis for developing relevant clinical interventions in China.
Methods:All published studies focusing on the risk factors for PD among elderly patients in Wanfant Data, China National Knowledge Infrastructure (CNKI), and VIP were collected according to the inclusion and exclusion criteria of this study. A meta-analysis was performed on casecontrol studies using RevMan5.2 software, and the incidence of PD risk factors was calculated among case series.
Results:Sixteen studies, including 8 case-control studies and 8 case series, were included in the current study. There were 353 cases and 2008 controls in the case-control studies. The pooled odds ratios (95% CI) of PD risk factors were as follows: hypoxemia, 2.58 (1.59~4.18); pulmonary infection, 4.51 (2.23~9.13); hypertension, 2.16 (1.20~3.89); coronary heart disease, 1.50 (0.82~2.73); post-operative pain, 3.18 (1.63~6.20); general anesthesia, 3.64 (0.94~14.11); operative time, 1.70 (0.79~3.66); and senility, 0.52 (–0.25~1.29). The meta-analysis showed that hypoxemia, pulmonary infection, hypertension, coronary heart disease, post-operative pain, general anesthesia, operative time, and senility were signif cant risk factors for PD. There were 404 cases in the case series, and the incidence of hypoxemia, hypertension, general anesthesia, diabetes mellitus, senility, coronary heart disease, pulmonary infection, and cerebrovascular disease was 62.62%, 55.90%, 33.7%, 24.8%, 16.58%, 15.3%, 13.9%, and 12.1%, respectively, which was much higher than other risk factors.
Conclusion:Senility, hypertension, coronary heart disease, diabetes mellitus, pulmonary infection, hypoxemia, post-operative pain, and general anesthesia are signif cant risk factors for PD among elderly Chinese patients.
Elderly patient, Post-operative delirium, Risk factor, Systematic review, Metaanalysis
Introduction
Delirium, one of the acute organic brain syndromes, is an important complication that commonly occurs in post-operative senile patients; the incidence of delirium is 8%~78%. Post-operative delirium (PD) cannot only increase the morbidity and mortality of pressure sores, pulmonary infections, falls and phlebothromboses, but can also lead to depression or self-mutilation. Thus, the duration of hospitalization can be prolonged. There is no scientif c consensus regardingthe pathogenesis, epidemiologic status, diagnosis, therapy, and risk factors for PD [1, 2]. In the current study, meta-analysisbased qualitative and quantitative assessments of case-control studies and a statistical summary of case series and reports were made to investigate the risk factors for PD in elderly patients.
Data and methods
R etrieval strategy
All published articles which focused on the risk factors for PD among elderly patients before December 2013 in the Wanfang Data, CNKI, and VIP databases were collected. Based on several pre-checks, specif c co-locations of subject headings and free words were determined and searched, and references were traced when necessary. CNKI retrieval serves as an example (Fig. 1).
Inclusion and exclusion criteria
For case-control studies, the inclusion criteria were as follows: (1) published studies focused on the risk factors for PD among Chinese patients >60 years of age; (2) studies with a consistent def nition of disease diagnosis and study essentials, and the diagnostic criteria for delirium according to the 4th edition of theDiagnostic and Statistical Manual of Mental Disorders(DSM-IV-TR); (3) research time and site specif ed; and (4) study design and sample size clearly stated. The exclusion criteria were as follows: (1) study replicated a previously published study; (2) poor quality; and (3) f rst-hand data were incomplete.
For case series, the inclusion criteria were: (1) diagnostic criteria for delirium were in accord with DSM-IV-TR; (2) with highly suspected and clearly described etiological factors. The exclusion criteria were: cases without clearly described etiological factors or suff cient diagnostic evidences.

Fig. 1. CNKI retrieval strategy.
Statistical analysis and methods
RevMan 5.2 software was used for analysis. The included studies were heterogeneity-tested, and the pooled odds ratio (POR) with 95% CI (in parentheses) was calculated. If homogeneity existed between various study results, a f xed-effect model was used. If homogeneity did not exist, a random-effect model was used. AP<0.05 suggested that a risk factor might be related to senile PD. The proportional occurrence of each risk factor was compared between high risk factors among case reports and case series (Charts 1–7, Tables 1 and 2).
Results
Included articles
Fifty-nine study-related articles were retrieved. Among the retrieved articles, 16 (8 case-control studies and 8 case series) were selected as follows: 1) 15 replicated studies or studies with incomplete data sets were deleted; 2) 3 studies were excluded based on a review of the titles and abstracts; 3) studies which met the inclusion criteria after scanning the full content were selected (Chart 8). There were 26 risk factors analyzed among these articles (Tables 3 and 4).
Discussion
Risk factors
A number of studies with a focus on delirium have followed the f rst relevant research conducted by Engel and Romano in the 1840s, but the results differ due to various study methods, patient selection, and diagnostic criteria [1]. Based on an analysis of delirium-related articles (8 case-control studies and 8 case series), the current study shows that pre-operative complications (hypertension, CHD, DM, and pulmonary infection), post-operative hypoxemia, post-operative pain, and general anesthesia are signif cant risk factors for delirium in elderly patients (≥70 years of age).

Chart 1. Meta-analysis forest plot of hypoxemia and PD in elderly patients.
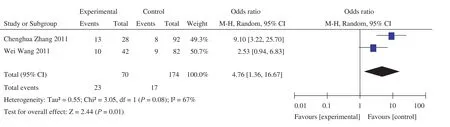
Chart 2. Meta-analysis forest plot of pre-operative pulmonary infection and PD in elderly patients.
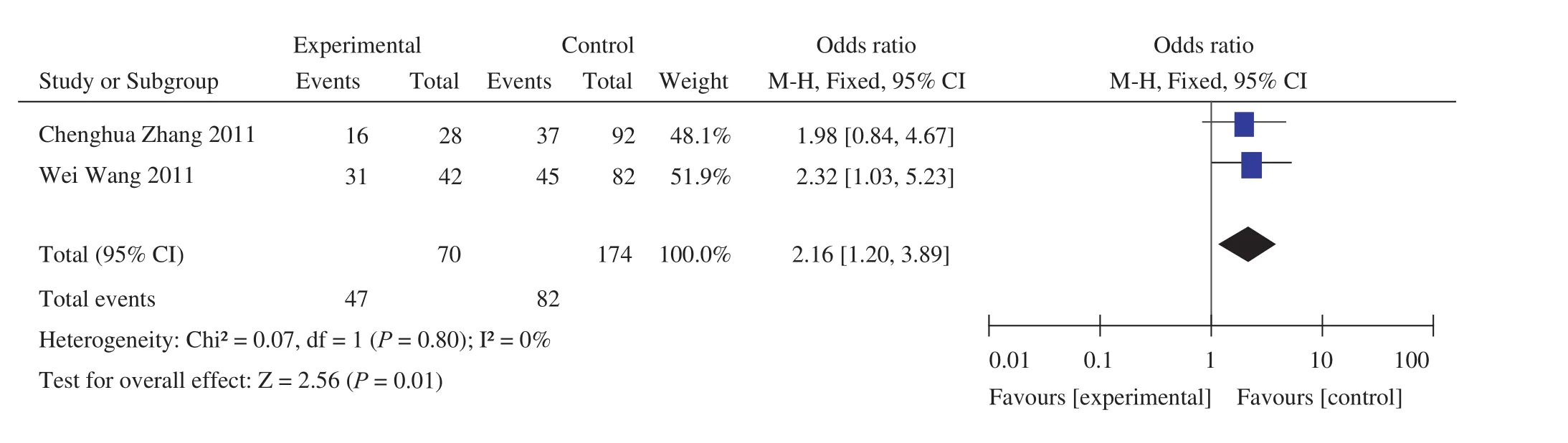
Chart 3. Meta-analysis forest plot of pre-operative hypertension and PD in elderly patients.
Physiologic functions degenerate in older people. Indeed, brain function degeneration and a decline in the synthesis of acetylcholine, one of the central neurotransmitters, may be a key etiologic factor for delirium. Comparative studies have shown that the incidence of PD in patients >65 years of age is 4–10 times higher than young people and 3 times higher inpatients >75 years of age than patients >65 years of age [19]. Case-control studies [5, 6, 9] have shown that senility (≥70 years of age) is a risk factor for PD, with but one exception [7], while the combined analysis of the studies did not demonstrate senility (≥70 years of age) to be a risk factor for PD; however, based on a case series senility (≥70 years of age) wasshown to have a high incidence among all risk factors (16.58% [67/404]). Thus, it can be concluded that senility (≥70 years of age) should not be dismissed as a causative factor for PD.

Chart 4. Meta-analysis forest plot of pre-operative coronary heart disease and PD in elderly patients.

Chart 5. Meta-analysis forest plot of general anesthesia and PD in elderly patients.

Chart 6. Meta-analysis forest plot of senility (≧70 years of age) and PD in elderly patients.
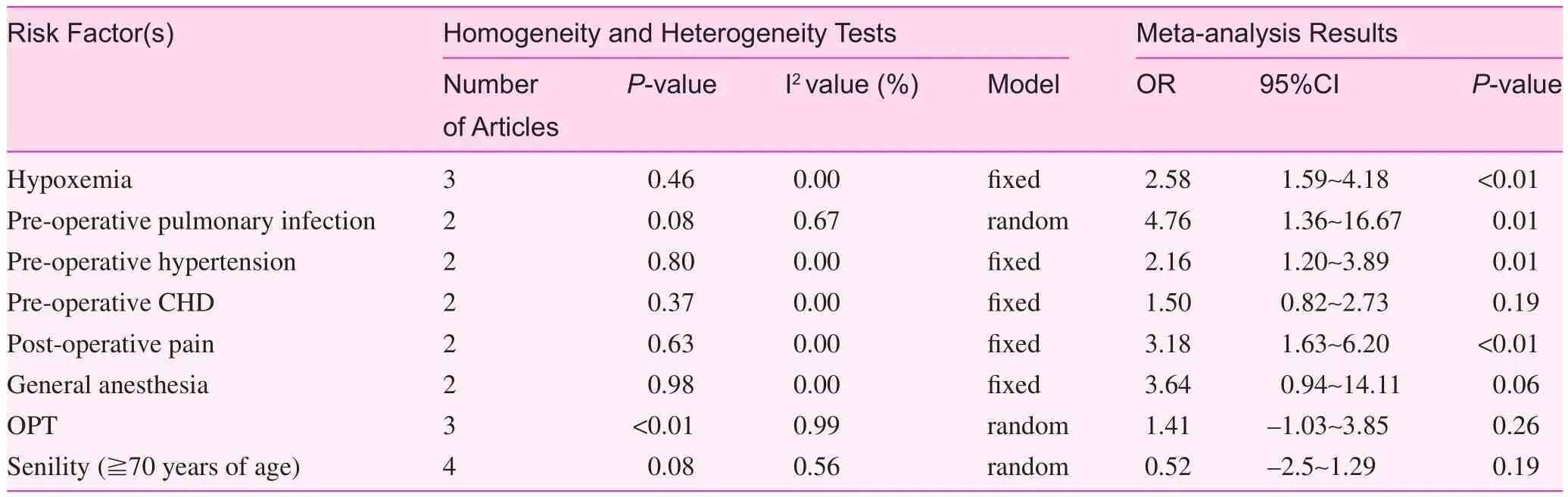
Table 1. Meta-analysis results of PD risk factors in elderly patients

Table 2. Statistical data of case series (n=404)
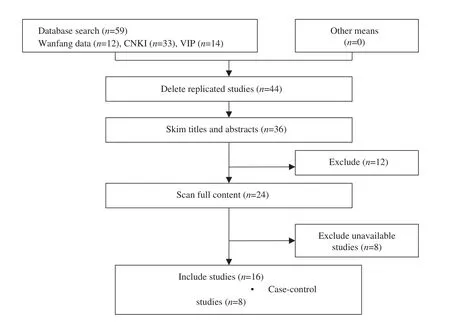
Chart 8. Screening process.
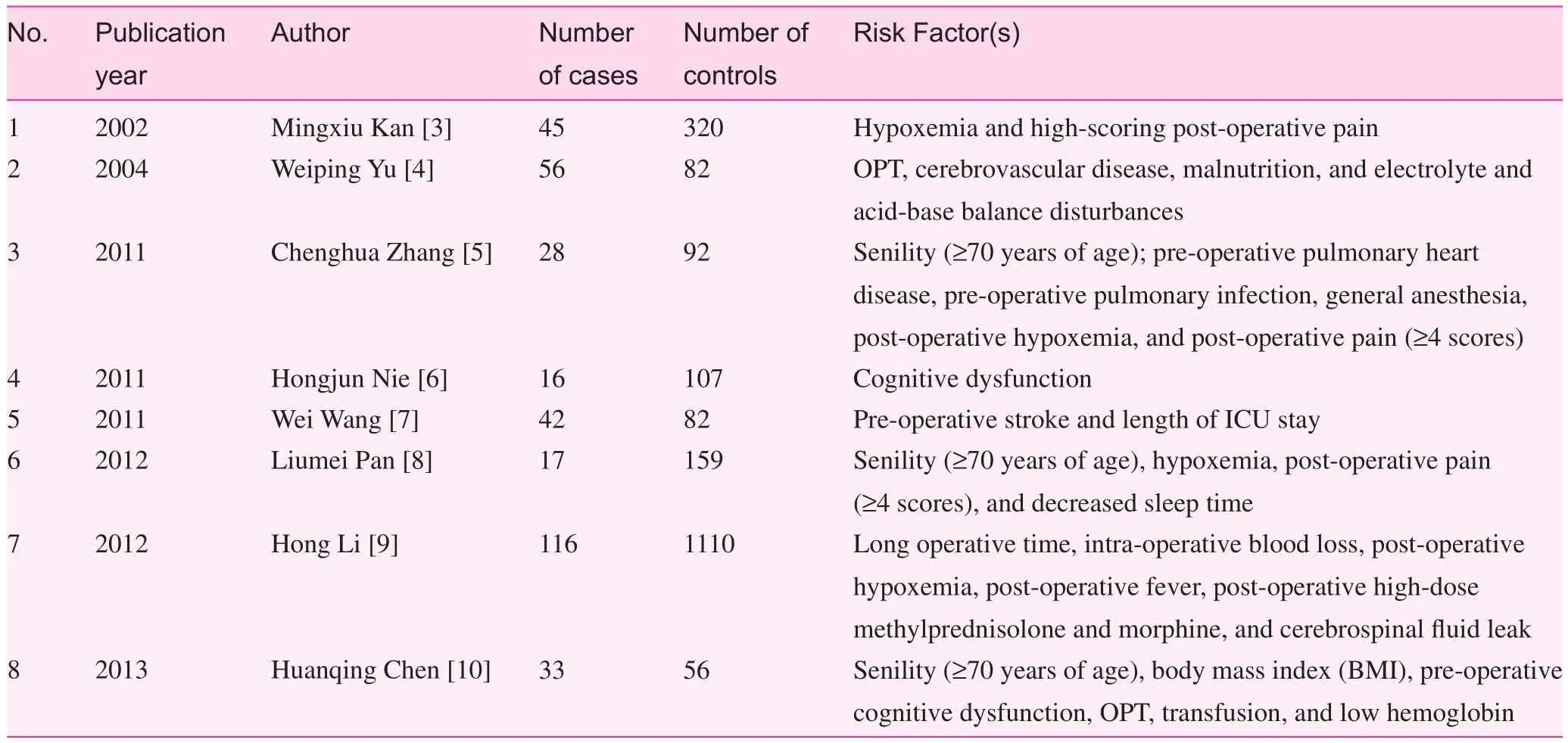
Table 3. Characteristics of case-control studies
Chronic hypertension has a negative inf uence on patient memory, abstract reasoning ability, attention, and cerebral auto-regulation, which collectively make the cerebrum moresensitive to changes in blood pressure; when the blood pressure drops, cerebral ischemia and anoxia will develop and delirium will occur. This process takes place in patients with pulmonary infections because the decrease in effective ventilation will have a negative effect on the cerebral oxygen supply. Oh and other researchers [20] have shown that the level of blood glucose has a positive correlation with the incidence of delirium; controlling blood glucose can reduce the incidence of delirium. Based on case-control studies, pre-operative pulmonary heart disease and pulmonary infections have been shown to be independent risk factors for PD [5]. Pre-operative hypertension and DM are also independent risk factors of PD [7], while any pre-operative disease is a signif cant risk factor for PD [6]. Based on an analysis of all relevant studies, we conclude that pre-operative hypertension, DM, CHD, and pulmonary infection are key risk factors for PD. The pertinent case series have conf rmed that the incidence of pre-operative hypertension, DM, CHD, and pulmonary infection (55.90% [226/404], 24.80% [100/404], 15.30% [62/404], and 13.90% [56/404]) are higher among all the risk factors for PD in elderly patients.
An anesthetic-related study showed that [21] benzodiazepines and propofol have high aff nities for GABA receptors in the central nervous system; the mimetic effect of GABA may cause changes in neurotransmitters and lead to delirium. Another study [22] showed that general anesthesia can decrease the cerebral metabolic rate, which in turn may cause delirium. There are several studies, however, that show general anesthesia cannot lead to delirium [23]. General anesthesia has been reported to be an independent risk factor for senile PD [5], but anesthesia methods are not related to PD [7]. A combined analysis of these studies showed that general anesthesia is a risk factor for PD in elderly patients, which was conf rmed in a case series (33.70% [136/404]).
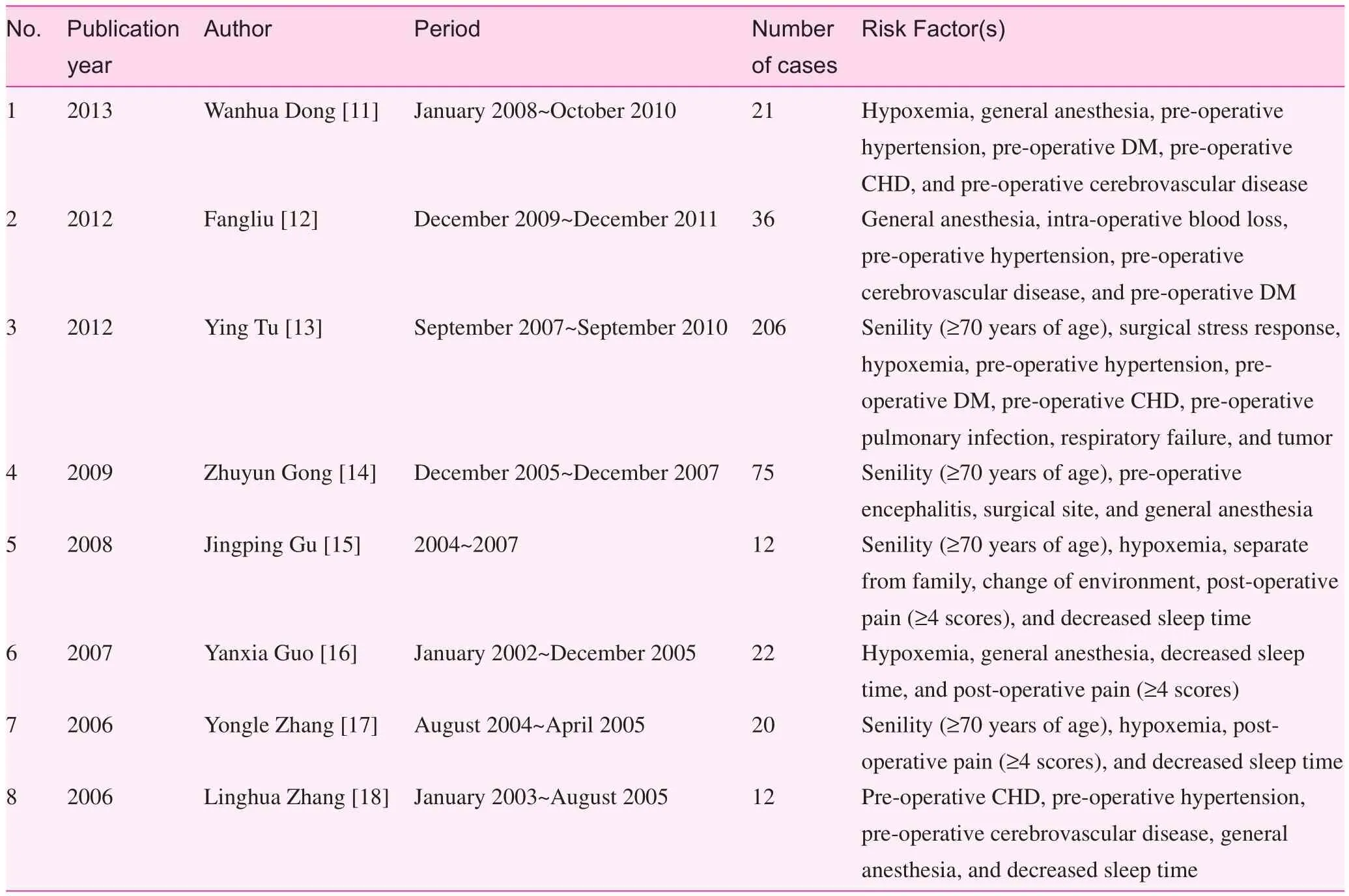
Table 4. Characteristics of case series
Pain is a form of an acute stress disorder. When people are stressed, blood epinephrine and norepinephrine levels will increase, the rate of cerebral blood f ow will increase, and oxygen consumption will increase. As a result, the metabolism of brain cells will be affected negatively, thus decreasing the information exchange capabilities of cells. Post-operative pain ref ects the body’s response to noxious stimulation. Postoperative pain can initiate changes in neuroendocrine function, especially an excess secretion of serum cortisol, can inhibit hippocampal cortex function and cause cognitive dysfunction [24] as well as delirium. In addition, post-operative pain can seriously impact patient sleep quality, and result in an irregular sleep cycle, including sleep deprivation, thus prompting the development of delirium. Post-operative pain has been shown to be a risk factor for delirium by one study [8], but not another study [5]. The current study showed that post-operative pain is an important among risk factor for senile PD.
Diminished respiratory function and cardiocerebral vascular diseases will cause dysfunction of cerebral blood f ow post-operatively and lead to hypoxemia. There is a signif cant correlation between hypoxemia and PD; specif cally, hypoxemia is a precipitating factor for early post-operative cerebral dysfunction [25]. Rosenberg and other researchers [26] have shown that post-operative hypoxia is a key factor causing dysphrenia, and inadequate oxygen can prevent PD. Another study [27] showed that among 92 surgery patients, there were 39 (42%) who developed delirium post-operatively. Post-operative delirium commonly manifests on the second post-operative day, ref ecting the level of hypoxia on the f rst day post-operatively [27]. Case-control studies [3, 5, 8] which have focused on the correlation between hypoxemia and PD have shown that hypoxemia is a risk factor for senile PD. In a case series involving 404 participants, there were 253 PD patients (62.62% [253/404]) with hypoxemia, which is consistent with the above f ndings.
Interventions of PD
PD prevention is important; to do so requires elimination of the risk factors [28]. Due to the characteristics of delirium, acute onset (within hours or days) and undulatory state (the occurrence, exacerbation, remission, and disappearance of symptoms often occurs within 24 h), delirium is easily underestimated and missed in clinical practice [7]. Considering all of the risk factors and characteristics of PD, the following interventions should be developed: (1) Elderly patients should be assessed comprehensively and accurately pre-operatively for multiple organ function, and the complications should be treated to improve general health status, thus reducing the incidence and severity of PD. (2) Blood gases and electrolytes should be monitored pre- and post-operatively to maintain water, electrolyte, and acid-base balance, and preserve circulatory stability. (3) Implement preventive analgesia to reduce neurotransmitter release and prevent the occurrence of PD. Large doses of steroids and morphine should be used with caution. (4) Preventive oxygen therapy should be classif ed as routine treatment to control pulmonary infection and hypoxemia. (5) Security measures and intensive perambulate should be taken to ensure the safety of patients with delirium-related dysphoria and hallucinations. Sedatives and analgesics should be given accurately according to medical orders. Observe the changes in patient vital signs and consciousness, and closely evaluate the severity of disease properly. (6) Add a daily delirium assessment to the post-operative nursing routine, and improve early identif cation and prevention capabilities of medical workers to reduce the incidence of delirium.
Limitation and enlightenment of this study
Through a systematic review, the current study showed that senility, pre-operative hypertension, DM, pulmonary infection, post-operative hypoxemia, pain, and general anesthesia are signif cant risk factors for PD; however, because the sample size in this study was not large enough, the power of testing may be on the low side, thus affecting the veracity of the meta-analysis. Indeed, a quality case-control study with a larger sample size is needed to verify the conclusions reached in the current study.
Conf ict of interest
The authors declare no conf ict of interest.
1. Li u JH, Yue Y. Postoperative delirium in elderly patients. Int J Anesthesiol Resus 2009;30:48–51.
2. Liu C, Han XW, Ding XP, Lu HB, Zhou PL. Advances in postoperative delirium in elderly patients. The J Pract Med 2013;29:1891–3.
3. Kan MX, Jiang P, Wang J. Risk factors of postoperative delirium in elderly patients. J Jiangsu University (Medicine Edition) 2002;12:333–4.
4. Yu WP, Jing ZP, Zhao J, Zhao ZQ, Bao JM, Feng X, et al. Postoperative delirium in the elderly after endovascular exclusion for abdominal aortic aneurysms. Chinese J Geriatr 2004;23:393–5.
5. Zhang CH, Ma WQ, Yang YL, Dong FT, Wang HM. The incidence and risk factors of postoperative delirium in elderly patients undergoing hip fracture operation. J Clin Anesthesiol 2011;27:455–7.
6. Niu HJ, Zhao B, Zhang YQ, Jiang YH, Yang YX. Risk factors of 123 delirium patients after hip fracture surgery. Guizhou Med J 2011;35:743–6.
7. Wang W, Wang DX. The incidence and risk factors of postoperative delirium in elderly patients in critical condition after non-cardiac surgery. Med J Chinese People’s Liberation Army 2011;36:653–6.
8. Pan LM, Wang Y, Xu XX, et al. Risk factors of senile total hip replacement arthroplasty and its nursing care. Nurs Pract Res 2012;9:16–7.
9. Li H, Li CD, Yi XD, Liu H, Liu XY. Analysis of risk factors for delirium in the elderly patients after spinal operation. J Peking University (Health Sciences) 2012;44:847–50.
10. Chen HQ. Risk factors of senile delirium patients after hip fracture surgery. Chinese J Rural Med Pharm 2013;20:11–2.
11. Dong WH, Wu MQ, Jiang YY. Relevant factors of delirium in the elderly patients after spinal operation. Guide of China Med 2013;11:705–6.
12. Liu F. Risk factors of senile delirium after hepatoma surgery and its nursing strategy. J Nurs Train 2012;27:2285–7.
13. Tu Y, Qian L. Etiological factors of 206 senile postoperative delirium and its nursing intervention. J Qilu Nurs 2012;18:80–1.
14. Gong ZY, Wang B. Clinical analysis and nursing strategy of acute postoperative senile delirium in ICU. Chinese Nurs Res 2009;23:10–2.
15. Gu JP. Relevant factors of delirium patients after CABG and its nursing strategy. Nei Mongol J Tradit Chinese Med 2008;9:47–8.
16. Guo YX, Chang XL, Liu AQ, Xu CY, Ma LQ. Etiological factors of 22 senile delirium after hip replacement arthroplasty and its nursing experience. J Qilu Nurs 2007;13:92–3.
17. Zhang YL, Dou DM, Zhang SQ, Wang X, Cao HE, Zhang YL. Risk factors of senile postoperative delirium. Chinese General Pract 2006;9:717–8.
18. Zhang LH, Le GF. Etiological factors of senile delirium after emergent abdominal operations and its nursing. Chinese Nurs Res 2006;20:2033–4.
19. Ruan J, Gao Y, Hang YN. Central nervous system complications after general anesthesia. Chinese J Med Guide 2007;9:387–8.
20. Oh YS, Kim DW, Chun HJ, Yi HJ. Incidence and risk factors of acute postoperative delirium in geriatric neurosurgical patients. J Korean Neurosurg Soc 2008;43:143–8.
21. Pandh aripande P, Shintani A , Peterson J, Pun BT, Wilkinson GR, Dittus RS, et al. Loraz epam is an in dependent risk factor for transitioning to delirum in intensive care unit patients. Anest hesiology 2006;10:21–6.
22. Saniova B, Drobny M, Sulaj M. Delirium and postoperative cognitive dysfunction after general anesthesia. Med Sci Monit 2009;15:81–7.
23. Morrison RS, Magaziner J, Gilbert M, Koval KJ, McLaughlin MA, Orosz G, et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. The J Gerontol 2003;58:76–81.
24. Rapeli P, Kivisaari R, Autti T, Kähkönen S, Puuskari V, Jokela O, et al. Cognitive function during early abstinence from opioid dependence: a comparison to age, gender, and verbal intelligence matched controls. BMC Psychiatry 2006;6:9.
25. Zhang LJ. Clinical analysis and strategy of senile postoperative delirium. Nurs J Chinese People’s Liberation Army 2006;23:59–60.
26. Roeeaberg J, Aakerlund LP. Postoperative delirium: treatment with supplementary oxygen. Br J Anaemh 1994;75:286–90.
27. Li YC. Hypoxemia and organ dysfunction in later postoperative period. Int J Anesthesiol Resus 1997;18:45–6.
28. Gu M, Wang Z. Diagnosis and treatment of emergent delirium. Chinese J Crit Care Med 2010;30:393–7.
Nursing Department, Zunyi Medical College Aff liated Hospital, Guizhou 563003, China
Zhixia Jiang
Nursing Department, Zunyi Medical College Aff liated Hospital, Guizhou 563003, China
E-mail: jzxhl@126.com
Funded by the International S&T Cooperation Program of Guizhou Province in 2010 (G7033) Project of Humanitarian Company Division of Zunyi Medical College in 2010 (F-427)
28 September 2014;
Accepted 15 November 2014
 Family Medicine and Community Health2014年4期
Family Medicine and Community Health2014年4期
- Family Medicine and Community Health的其它文章
- The Community Hub: a proposal to change the role of Residential Aged Care Facilities (RACFs)
- A case-control study on family environment characteristics of accident-prone children
- Analysis of the characteristics of coronary artery lesions in patients with obstructive sleep apnea-hypopnea syndrome and inf uencing factors
- Effect of core stability training on balance in elderly women
- Effects of psycho-scene-drama on empathic ability of patients with chronic schizophrenia
- Pre hospital medical services and paramedic engagement in Australian health care – Improving the pathways of care through collaborative action
