Analysis of the characteristics of coronary artery lesions in patients with obstructive sleep apnea-hypopnea syndrome and inf uencing factors
Bin Sun, Jing Liu, Ding Huang, Cheng Liu
Analysis of the characteristics of coronary artery lesions in patients with obstructive sleep apnea-hypopnea syndrome and inf uencing factors
Bin Sun, Jing Liu, Ding Huang, Cheng Liu
Objective:The current study involved an analysis of the characteristics of coronary artery lesions of patients with obstructive sleep apnea-hypopnea syndrome (OSAHS) and the corresponding inf uencing factors.
Methods:One hundred twenty patients were selected by sleep apnea monitoring and coronary angiography. According to the apnea-hypopnea index (AHI), the patients were divided into the following 3 groups: patients with an AHI<10 times/h as the control group (n=25); patients with an AHI=10~15 times/h as the mild OSAHS group (n=32); and patients with an AHI>15 times/h as the moderate-to-severe OSAHS group (n=63). The clinical and laboratory test data of patients in each group were collected. A single-factor ANOVA and multi-factor logistic regression analysis were performed on the study data to analyze the coronary artery lesions in patients with OSAHS and the corresponding inf uencing factors.
Results:(1) With respect to smoking, alcohol consumption, BMI, blood glucose, blood lipids, and blood pressure among the three groups, there were no signif cant differences between the three groups; however, age did differ among the three groups (P<0.05). (2) The incidence of anterior descending artery, right coronary artery, single-vessel, and coronary artery lesions as determined by coronary angiography was signif cantly different (P<0.05). The incidence of these vascular lesions in the moderate-to-severe group was higher than the mild group, and the incidence of coronary artery lesions in the moderate-to-severe group was higher (P<0.0167). (3) Based on multifactor logistic regression analysis, alcohol consumption (OR=7.058; 95% CI, 1.953–25.508), age (OR=1.845; 95% CI, 1.121–3.038), and the AHI (OR=2.404; 95% CI, 1.088–5.314) were the major risk factors for coronary artery lesions. Alcohol consumption (OR=12.114; 95% CI, 3.058–47.979) and the AHI (OR=3.052; 95% CI, 1.210–7.694) were the risk factors for single-vessel disease. Age (OR=2.812; 95% CI, 1.236–6.400) was the major risk factor for multi-vessel disease.
Conclusion:The probability of coronary artery lesions increased with OSAHS severity. The main manifestation of the increased possibility was single-vessel coronary artery lesions. In singlevessel disease, the anterior descending branch and the right coronary artery were the most vulnerable, which may be related to the anatomic distribution. Alcohol consumption, age, and AHI are the major risk factors for coronary artery lesions. Alcohol consumption and AHI are major risk factors for single-vessel disease. Age is the main risk factor for multi-vessel disease.
Obstructive sleep apnea-hypopnea syndrome, Coronary artery lesions
Introduction
Obstructive sleep apnea-hypopnea syndrome (OSAHS) is the most common form of sleep respiratory disorder. Previous studies have shown that the effects of OSAHS on the body are complex and widespread, and could lead to damage to multiple systems and organs, particularly complications of cardiovascular diseases. Schafer et al. [1] reported that approximately 50% of OSAHS patients have coronary artery lesions, which was conf rmed by coronary angiography. To better understand the specif city of the coronary artery lesions of patients with OSAHS, the current study retrospectively analyzed 120 patients with coronary heart lesions who received sleep monitoring and coronary arteriography in our hospital to better determine the clinical characteristics of the disease and provide new ideas and an effective clinical basis for carrying out early prevention and treatment of coronary artery lesions complicated by OSAHS.
Subjects and methods
Subjects
One hundred twenty patients with OSAHS treated in the Heart Center of the First Aff liated Hospital of Xinjiang Medical University Hospital between June 2013 and June 2014 were selected, among whom 84 were males (70%) and 36 were females (30%), with a mean age of 48.64±9.45 years. The OSAHS diagnostic criteria were based on the “Guidelines for Diagnosis and Treatment of Obstructive Sleep Apnea-Hypopnea Syndrome” (2011 revised edition) [2]; specif cally, patients with symptoms, such as typical nocturnal sleep snoring with apnea and di urnal sleepiness (ESS score≥9 points), stenosis and obstruction in any site of the airway, as indicated on physical examination, and a apnea-hypopnea index (AHI)≥5 times/h were diagnosed with OSAHS. For patients with non-obvious diurnal sleepiness (ESS score <9 points) and an AHI≥10 or ≥5 times/h, the presence of one or more of the following symptoms was diagnostic: cognitive dysfunction; coronary artery disease; cerebrovascular disease; diabetes; and insomnia. Based on the AHI, patients could be divided into the following three groups: patients with an AHI<10 times/h as the control group (n=25); patients with an AHI=10~15 times/h as the mild OSAHS group (n=32); and patients with an AHI>15 times/h as the moderate-to-severe OSAHS group (n=63).
The exclusion criteria were as follows: (1) patients with nasal and chronic lung diseases; (2) congenital heart disease, severe arrhythmias, and valvular heart disease; (3) infectious and rheumatic autoimmune diseases; and (4) severe liver and renal function impairment, chronic wasting diseases, and malignant tumors.
Methods
General information collection:The clinical data of patients included in the study were collected, such as age, and cigarette smoking and alcohol consumption history. Smoking was def ned as at least 1 cigarette per day, and a smoking history for >1 consecutive year, and still smoking now or quitting smoking <6 months before enrollment in the study. Consuming alcohol was def ned as drinking at least once a week for >1 consecutive year, and still drinking now or quitting drinking<6 months before enrollment in the study. The blood pressure was measured after patients were admitted to the hospital, the diagnosis of hypertension was based on Chines e Hypertension Prevention Guideline (2010 revised edition) [3].
Examination of biochemical indices:All patients fasted for 8 h, then had a fasting venous blood sample drawn the next morning. A Roche C8000 automatic biochemical analyzer was utilized to test the triglycerides (TG), total cholesterol (TC), fasting blood glucose (FBG), and blood glucose 2 h after an oral glucose tolerance test (2 hPG). The 2009 Diabetes Diagnosis and Treatment Guidelines of the American Diabetes Association [4] were used to establish a diagnosis of diabetes.
Sleep respiration monitoring:All subjects underwent sleep monitoring 7 h at night, and the Australian PSG instrument Com2pumedics2 E-type analyzer was utilized for analysis to simultaneously monitor blood oxygen saturation, abdominal breathing movements, snoring, and oral and nasal airf ow. After monitoring, trained technicians analyzed the data, including the apnea-hypopnea index (AHI) and the lowest blood oxygen saturation (LSaO2), and the height and weight were measured to calculate the body mass index (BMI) the evening before monitoring, as follows: BMI=weight (kg)/ height (m)2.
Coronar y angiography:A GE Innova200 all-digital cardiovascular imaging machine was used for coronary angiography and the Beijing Strong ST-DDS v3.1.24.10509+P2 medical imaging workstation system was used for image analysis to evaluate the main arteries of the coronary artery (left main coronary artery [LM], l eft anterior descending artery [LAD], left circumf ex artery [LCX], and right coronary artery [RCA]. Based on the number of main coronary arteries involved, diagnosis of single- and multi-vessel disease was made (multi-vessel disease was def ned as lesions involving two or more arteries). Coronary angiography was completed according to the Judkins method and the degree of blood vessel stenosis was determined by multi-position projection. According to the American College of Cardiology/American Heart Association (ACC/AHA) guidelines for coronary angiography, any lesions with ≥50% stenosis of the vascular inner diameter of any branch of the LM, LAD, LCX, and/or RCA meets the diagnostic criteria for coronary heart disease. The above operations were inspected by two experienced interventional cardiologists.
Statistical methods
Results
Basic information
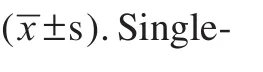
The comparison among the three groups in terms of gender, cigarette smoking, alcohol consumption, FBG, TG, TC, 24 hSBP, and 24 hDBP was not st atistically signif cant (P>0.05). The comparison among the three groups in terms of age generated a statistically signif cant difference (P<0.05), and the patients in the moderate-to-severe group were older than the patients in the mild group (P<0.05) (Table 1).
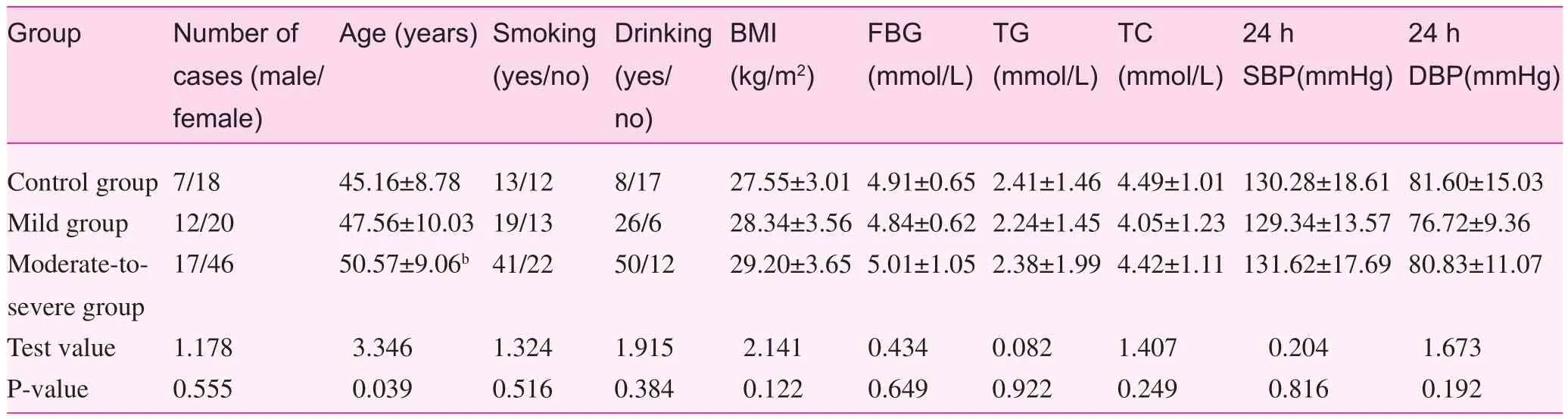
Table 1. Comparison of basic information between the three groups (x±s)
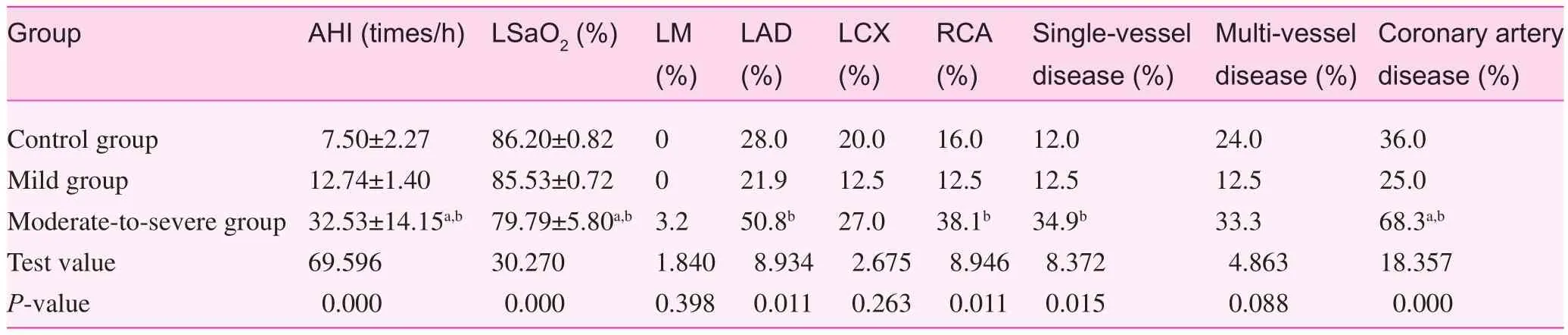
Table 2. Comparison of different indices between the groups (x±s)
Inter-group comparison for each indicator of sleep monitoring and coronary angiography
The comparison among the 3 groups with respect to patient sleep monitoring indicators, coronary angiography results, and the incidence of LAD, RCA, single-vessel, and multivessel lesions revealed signif cant differences (P<0.05). The AHI in the moderate-to-severe group was higher than the mild and control groups (P<0.05), and the LSaO2in the moderate-to-severe group was lower than the mild and control groups (P<0.05). The incidence of LAD, RCA, and single-vessel lesions in the moderate-to-severe group was higher than the mild group (P<0.05). The LVEDD and IVST in the moderate-to-severe group were higher than the moderate group (P<0.05), and the rate of LVEDD and IVST in the severe group was higher than the moderate group (P<0.05). The incidence of coronary artery disease in the moderateto-severe group was higher than the mild and control groups (P<0.05) (Table 2).
Factors inf uencing coronary artery disease, singlevessel lesions, and multi-vessel lesions
Gender, cigarette smoking, alcohol consumption, age, 24 hSBP, 24 hDBP, AHI, and LSaO2were used as independent variables, and coronary artery disease, single-vessel lesions, and multi-vessel lesions were used as dependent variables to conduct logistic regression analysis (for specif c variable assignment, see Table 3). Alcohol consumption, age, and AHI were shown to be the major risk factors for coronary artery disease. Alcohol consumption and AHI were the main risk factors for single-vessel lesions, and age was the main risk factor for multi-vessel lesions (Table 4).
Discussion
The adult morbidity rate of OSAHS is 2%–4% [5]. It has been shown that the morbidity rate of OSAHS patients with hypertension or coronary artery disease is 30%–50% [6]. The incidence of coronary artery disease ranks f rst among various types of heart disease. Therefore, the incidence of coronary artery disease in patients with OSAHS has features, such as coronary lesions and the severity of the lesion, that are worthy of further exploration. It has been recommended [7] thatpatients with moderate or severe respiratory disturbances need treatment (AHI>15 times/h), but the following question remains: Will the coronary lesions become more severe in patients with OSAHS? Therefore, in the current study the patients with moderate-to-severe OSAHS were considered as the same observation group in whom to analyze the results of coronary angiography.
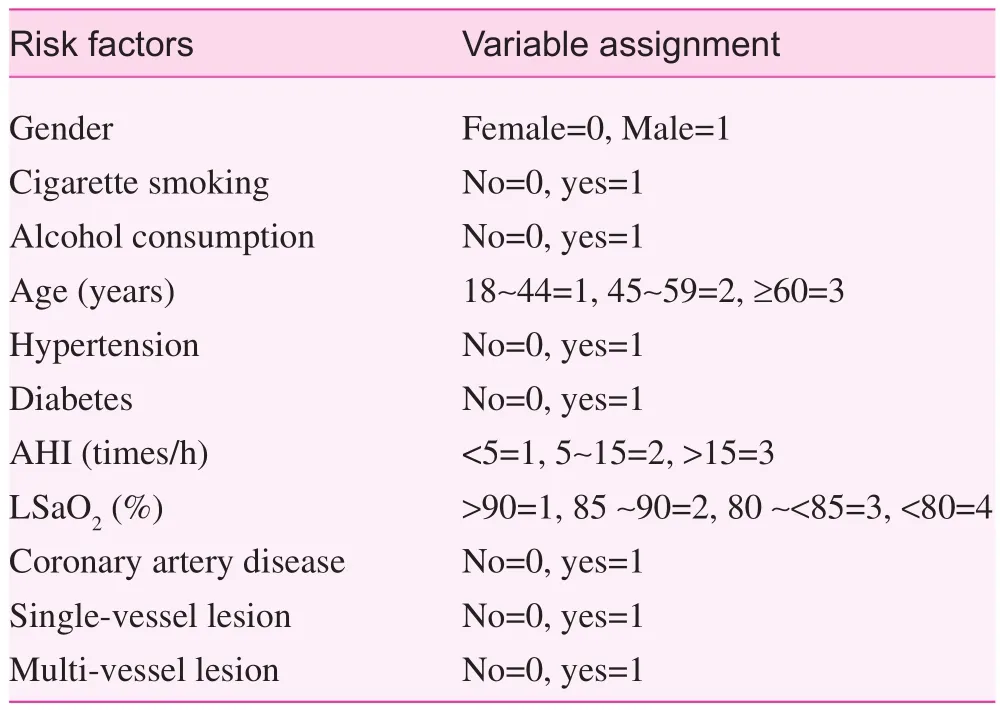
Table 3. Variable assignment
A baseline data comparison showed that among the three groups, age was a signif cant factor (P<0.05); specif cally, with an increase in the severity of OSAHS, age gradually increased. The results conformed to major risk factors in the Guidelines for the Diagnosis and Treatment of Obstructive Sleep Apnea – Hypopnea Syndrome (2011 revised edition) [2]. The analysis of variance among the three groups indicated that there was a difference with respect to the anterior descending artery, right coronary artery, single branch, and coronary artery disease; the incidence of descending coronary artery lesions, right coronary artery lesions, and single-vessel lesions with in patients with severe OSAHS was higher than control patients and patients with mild OSAHS, and the differences were statistically signif cant (P<0.05). It was shown that with exacerbations of OSAHS, the probability of coronary artery disease increases; the main manifestation was an increase in single-vessel coronary artery lesions (mainly the anterior descending or right coronary artery lesions).
Logistic regression analysis was performed on the occurrence of coronary heart disease, which showed that alcohol consumption, age, and AHI are independent risk factors for coronary artery disease. Except that age was a non-controllable risk factor, drinking and AHI were independent riskfactors for coronary artery disease. A meta-analysis, which summarized 177,723 subjects with coronary artery disease [8], showed that moderate drinking might reduce the morbidity and mortality of East Asian men with coronary artery disease. With an increase in alcohol consumption, the risk of all-cause mortality signif cantly increased, and the consumption of daily alcohol should not exceed 40 g. It was suggested that alcohol consumption is a risk factor for coronary artery disease, which is thought to be related to the excessive alcohol consumption of the subjects included in the current study. The results of the study showed that with an increase in AHI, the risk of coronary artery disease increased, which is consistent with domestic and international studies [9, 10], and the following mechanisms are considered: 1) Endothelial dysfunction is the initiating step in coronary atherosclerosis. NO is a protective factor for endothelial cell function, and endothelin (ET) is an endothelium-derived vasoconstrictive factor secreted by endothelial cells. Hypoxia and radical effects can raise the level of ET, and ET secretion increases and the NO:ET ratio decreases, thereby contributing to the occurrence and development of atherosclerosis. Some studies have suggested that changes could occur to NO and ET concentrations in patients with OSAHS. Ip et al. [11] reported that the level of NO in the blood of patients with OSAHS decreased. Phillips and Somers [12] found that the ET concentration of patients with OSAHS ET increased. A series of chain reactions might increase the possibility of coronary artery disease in patients with OSAHS. 2) Nocturnal hypoxia might affect the activity of the lipoprotein receptor, resulting in an increase in low-density lipoprotein, and the low-density lipoprotein became oxidized with the inf uence of superoxide and subsequently entered into macrophages to form foam cells, further aggravating atherosclerosis. 3) The OSAHS-induced hypercapnia will further increase blood viscosity, further give rise to blood f ow resistance, increase the burden on the heart, and further aggravate coronary ischemia and anoxia, thus leading to a coronary heart disease event. 4) The nocturnal repeated onset of apnea and a drop in blood oxygen saturation and oxygen partial pressure stimulate the interstitial cells adjacent to the renal tubules to secrete erythropoietin, and an increase in erythropoietin leads to a rise in blood viscosity and a decline in blood f ow. Such hemodynamic changes induce a drop in blood f ow and a decline in the coronary blood supply. 5) Bokinsky et al. [13] found that patients with OSAHS experienced an increase in spontaneous platelet aggregation during sleep, which dropped after treatment of continuous per nasal positive airway pressure ventilation, indicating that patients with OSAHS might secondarily develop changes in platelet function, leading to the formation of platelet aggregation and making concomitant arterial thrombotic diseases occur easily. These processes contribute to the development and progression of coronary atherosclerotic heart disease.
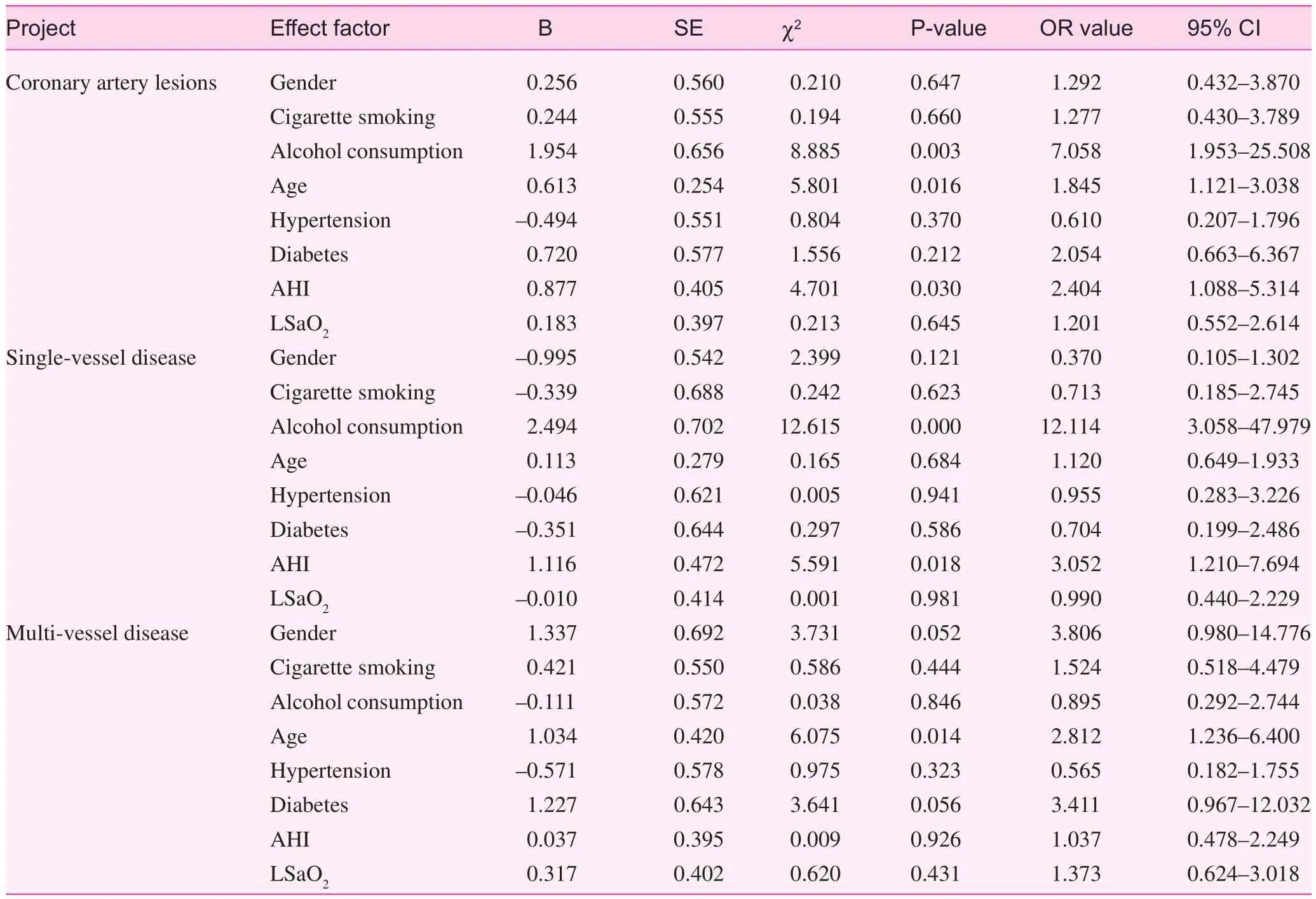
Table 4. Factors inf uencing coronary artery disease (CHD), and single- and multi-vessel lesions
Logistic regression analysis on the single- and multivessel lesions showed that alcohol consumption and AHI are risk factors for single-vessel lesions and age is a risk factor for multi-vessel lesions. In combination with the comparison among the three groups in terms of the results of coronary angiography, we found that exacerbation of the OSAHS conditions was more likely to induce single-vessel coronary lesions, and in single-vessel lesions, the left anterior descending artery and the right coronary artery were the most vulnerable vessels. Based on the analysis, the possible factors are as follows: the important pathologic changes of the cardiac target organ damage in patients with OSAHS change was left ventricular hypertrophy [14, 15]. Left ventricular hypertrophy led to an increase in myocardial oxygen consumption, but the blood supply of coronary arteries could be increased according to the ratio instead of the myocardial mass, and the “ischemia-reperfusion” injury induced by the long-term hypoxia/re-oxygenation process, platelet activation and aggregation, and local inf ammatory responses could all aggravate the coronary artery lesions. Fang et al. [16] showed that when there is an increase in the degree of left ventricular hypertrophy, the cardiac arteriolar diameter and lumen area decrease, the wall becomes thickened, and the coronary f ow reserve drops. Regarding cardiac reserve, the left anterior descending arteries are mainly distributed in the left ventricular anterior wall and anterior papillary muscles and cardiac apex, with a small portion of right ventricular anterior wall, and the two-thirds of the interventricular septum. The right coronary arteries are distributed in the posterior wall of two ventricles and one-third posterior to interventricular septum. Therefore, the anterior descending branch of coronary arteries and the right coronary arteries distributed in the leftventricle and interventricular septum are more easily damaged, resulting in lesions in the anterior descending artery and the right coronary artery.
To summarize, OSAHS is an independent risk factor for coronary artery disease. The exacerbation of OSAHS conditions are more apt to lead to coronary single-vessel lesions. In single-vessel lesions, the left anterior descending artery and the right coronary artery are the most involved vessels. This may be related to the anatomic distribution of the left anterior descending artery and the right coronary artery. Alcohol consumption, age, and AHI are the major risk factors for coronary artery disease. Alcohol consumption and AHI are major risk factors for single-vessel lesions. Age is the main risk factor for multi-vessel lesions. Due to the limited sample size, the correlation between other risk factors and coronary artery disease can be further statistically analyzed with expansion of the sample size. Currently, it is recommended that elderly patients with moderate-to-severe OSAHS consume alcohol in moderation, and active measures should be taken to control the disease for proper prevention and treatment of OSAHS.
Conf ict of interest
The authors declare no conf ict of interest.
1. Schafer H, Koehler, Ploch T, Hermann Peter J. Coronary artery lesions and upper airway obstruction. Sleep Res 1995;4 Suppl:185–9.
2. Group of Science of Sleep Respiratory Disturbance of Chinese Society of Respiratory Diseases of Chinese Medical Association. Guidelines for diagnosis and treatment of obstructive sleep apnea– hypopnea syndrome (2011 Revised Edition). Chin J Tubercul Res Dis 2012;35:9–12.
3. Revision Committee of “Chinese Hypertension Prevention Guideline” Guidelines for Chinese Hypertension Prevention Guideline 2010. Chin J Hypertens 2011;19:701–43.
4. Xie JT, Liu J, Zhou SP, Zhu SJ, Leng AW. Interpretation of guidelines for diabetes diagnosis and treatment in 2009 issued by American Diabetes Association. Chin General Prac 2009;12:1255–7.
5. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 2002;165:1217–39.
6. Milleron O, Pillière R, Foucher A, de Roquefeuil F, Aegerter P, Jondeau G, et al. Benef ts of obstructive sleep apnoea treatment in coronary artery disease: a long-term follow-up study. Eur Heart 2004;25:728–34.
7. The Report of an American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome def nition and measurement techniques in clinical research. Sleep 1999;22:667.
8. Liu PM, Dosieah S, Zheng HS, Huang ZB, Lin YQ, Wnag JF. Relationship between alcohol drinking and coronary artery disease in East Asian men. Chin J Cardiol 2010;38:1038–44.
9. Parish JM, Somers VK. Obstructive sleep apnea and cardiovascular disease. Mayo Clin Proc 2004;79:1036–46.
10. Ding SF, Liu HY, Meng K, Liu T, Wang L, Fan J, et al. Exploration on relationship between obstructive sleep apnea hypopnea syndrome and coronary artery disease. Chin J Tuberculosis Res Dis 2008;31:529–31.
11. Ip MS, Lam B, Chan LY, Zheng L, Tsang KW, Fung PC, et al. Circulating nitric oxide is suppressed in obstructive sleep apnea and is reversed by nasal continuous positive airway pressure. Am J Respir Crit Care Med 2000;162:2166–71.
12. Phillips BG, Somers VK. Sleep Disordered breathing and risk factors for cardiovascular disease. Curr Opin Pulm Med 2002;8:516–20.
13. B okinsky G, Miller M, Ault K, Husband P, Mitchell J. Spontaneous platelet activation and aggregation during obstructive sleep apnea and its response to therapy with nasal continuous positive airway pressure. A preliminary investigation. Chest 1995;108:625–30.
14. Li CM, Shi S, Zhu XM. Study on cardiac structure and its diastolic function of patients with obstructive sleep apnea-hypopnea syndrome. J Med Imaging 2009;19:1262–4.
15. Hedner J, Ejnell H, Caidahl IC. Left ventricular hypertrophy independent of hypertension in patients with obstructive sleep apne. Hypertension 1990;8:941–6.
16. Pei F, Li XY, Fang Y, Shi HY, Diao HJ. Pathological characteristics of heart and kidney arterioles in old patients with primary hypertension and left ventricular hypertrophy. Chin J Cardiol 2008;36:872–7.
The Second Department of Cardiology, the First Aff liated Hospital of Xinjiang Medical University, Urumchi, 830054, Xinjiang, China
Ding Huang
The Second Department of Cardiology, the First Aff liated Hospital of Xinjiang Medical University, Urumchi, 830054, Xinjiang, China
E-mail: sunbinky2012@163.com
10 September 2014;
Accepted 15 November 2014
 Family Medicine and Community Health2014年4期
Family Medicine and Community Health2014年4期
- Family Medicine and Community Health的其它文章
- Effects of psycho-scene-drama on empathic ability of patients with chronic schizophrenia
- Effect of core stability training on balance in elderly women
- Risk factors for post-operative delirium in elderly Chinese patients
- A case-control study on family environment characteristics of accident-prone children
- The Community Hub: a proposal to change the role of Residential Aged Care Facilities (RACFs)
- Family Medicine and Community Health
