临床局限性前列腺癌根治性切除与观察等待预后比较的Meta分析
罗 游 付生军 王志平 杨 立
兰州大学第二医院泌尿外科,兰州大学第二医院泌尿外科研究所,
甘肃省泌尿系疾病临床医学中心,甘肃省泌尿系疾病重点实验室(兰州 730000)
临床局限性前列腺癌根治性切除与观察等待预后比较的Meta分析
罗 游 付生军 王志平 杨 立*
兰州大学第二医院泌尿外科,兰州大学第二医院泌尿外科研究所,
甘肃省泌尿系疾病临床医学中心,甘肃省泌尿系疾病重点实验室(兰州 730000)
目的比较临床局限性前列腺癌行根治性切除(radical prostatectomy, RP)和观察等待(watchful waiting, WW)对患者生存的影响。方法通过计算机检索Medline、Cochrane Library、ISI web of knowledge、SinoMed文献检索平台,搜集国内外2014年7月前发表的关于早期前列腺癌根治性切除与主动监测的预后的随机、半随机对照试验或观察性研究,预后评价指标包括总体死亡、前列腺癌特异死亡;由2位研究者根据纳入与排除标准独立进行文献筛选、资料提取和质量评价后,采用RevMan5.2进行统计分析。结果纳入3个随机对照试验和10个临床队列研究,其中RCT共1 537例、队列研究共186 590例患者;Meta分析结果显示两种治疗方法(RP/WW)的总体死亡(ACM)风险为HR=0.59 [95%CI(0.51,0.69),P<0.00001],前列腺癌特异死亡(CSM)风险HR=0.43 [95%CI(0.32,0.58),P<0.00001],且不论RCT组还是队列研究组,结果均一致倾向RP。结论 早期前列腺癌根治性切除可减少总体死亡及前列腺癌特异死亡风险,对于早期局限性前列腺癌选择观察等待应当十分慎重。
前列腺肿瘤/外科学; 存活率分析; 综述; Meta分析
前列腺癌是男性泌尿系统常见的恶性肿瘤,其发病率逐年上升,2013年美国统计新发病例238 590例,位居男性肿瘤第一位,也是第二大肿瘤死亡原因[1]。随着前列腺特异性抗原(PSA)检测的普及,前列腺癌的发病率呈显著增加趋势,同时,也带来了前列腺癌根治手术的增加,对于是否因此而造成早期前列腺癌的过度诊断与治疗,以及PSA筛查的必要性均存在着争议[2,3]。前列腺癌的治疗手段主要以治愈性目的为主,包括根治性前列腺切除(radical prostatectomy, RP)、放疗,伴或不伴雄激素去势治疗,治愈性治疗方案常伴随着发生率较高的阳痿、尿路功能障碍、生活质量的显著降低以及高昂的治疗费用等[4-9]。观察等待(watchful waiting, WW)的定义是指在病程监测过程中,当患者症状或PSA水平出现进展时予以姑息性治疗[10],其内容与观察性治疗基本一致或可认为是其另一种表达方式,观察等待是保守治疗策略的一种。前列腺癌“缓慢、惰性”的自然史表现可能并未使治愈性手段获得更显著疗效优势,也使得观察等待成为可能[11,12]。虽然观察等待在欧洲泌尿科学会(EAU)及美国国立综合癌症网络(NCCN)均已被写进前列腺癌诊疗指南[10,13],但对于根治性切除与观察等待两者的预后效果在不同文献报道存在差异[14,15]。本文拟对早期局限性前列腺癌的不同干预效果进行系统评价及分析,为临床早期前列腺癌的治疗决策提供参考。
资料与方法
一、文献纳入与排除标准
(一)纳入标准
(1)研究类型为随机或非随机对照研究;(2)经病理或细胞学确诊为早期或局限性的前列腺癌患者(T1~2Nx~0Mx~0),不限年龄、种族;(3)文章内容包含有RP和WW两者统计数据的临床研究;(4)结局内容包括总体和(或)疾病特异死亡预后指标;(5)语种限定为中文及英文。
(二)排除标准
(1)标题摘要虽描述为临床局限性前列腺癌但实际包含了大量T3及以上分期的高风险前列腺癌的研究;(2)最长随访时间低于5年的研究;(3)重复发表的文献。
二、评价指标
评价两种不同干预措施效果的结局指标有:总体死亡风险和前列腺癌特异死亡风险。
三、检索策略
计算机检索Medline、Cochrane Library、ISI we of knowledge、SinoMed平台2014年7月前发表的关于早期RP与WW对比预后的相关文献,同时查询纳入文献的参考文献。英文检索式:radical prostatectom AND(observational therapy OR watchful waiting O expectant management OR deferred treatment OR delaye therapy OR conservative management)AND(earl prostate cancer OR localized prostate cancer OR low ris prostate cancer)AND(mortality OR survival),限定语种为英语。 中文检索式:(早期前列腺癌 OR 局限性前列腺癌 OR 低危前列腺癌 OR 低风险前列腺癌)AND(根治 OR 手术)AND (观察等待 OR 观察等待 OR 延缓治疗 OR 保守治疗 OR 监测)。
四、文献的筛选、数据提取和质量评价
由两位研究者根据纳入与排除标准独立进行文献筛选、资料提取与质量评价,并进行交叉核对,如遇分歧则通过讨论或征求第三方的意见解决。数据的提取尽量以文献原始数据为准,当资料不全或未详细描述时采用以下两种方法获取数据:(1)邮件联系作者获得原始数据;(2)对于文献未明确给出相关数据的可采用Tierney等[16]提出的数据提取方法和EXCEL表格计算HR和95%CI值;并参考AHR的一篇循证综述提供的结果[17]。质量评价RCT采用Cochrane 系统评价员手册5.1.0[18]中随机试验的偏倚风险评估工具,观察性研究采用NOS(Newcastle Ottawa Scale)量表对纳入研究的质量进行评价,5星以上考虑有较高质量。
五、统计分析
采用RevMan 5.2软件进行meta分析。本文研究预后问题均使用计数资料,采用风险比(HR)作为效应量。以各效应量及其95% CI表示结果。首先采用x检验对纳入研究结果进行异质性检验。若P≥0.1且I≤50%,提示各研究结果间无统计学异质性,采用固定效应模型进行Meta分析;若P<0.1但I2≤50%,提示各研究结果间存在异质性,但在可接受范围内,采用随机效应模型行Meta分析;若P<0.1或P≥0.1且I2>50%,认为各研究结果间异质性较大,对其异质性来源进行分析,并对可能导致异质性的因素进行亚组分析,若无明显临床异质性,采用随机效应模型进行Meta分析。Meta分析的检验水准设为α=0.05,Meta分析结果采用森林图呈现。
结 果
一、文献检索结果
通过相关检索式初检出715篇相关文献,逐层筛选后最终纳入3个随机对照试验(RCT)和10个队列研究涉及共18篇文献[14,15,19-34],包括188 127例患者,根治性前列腺切除105 213例,观察等待82 914例。18篇均为英文文献,无中文文献。筛选流程及结果如图1,纳入文献基本特征如表1。
二、纳入研究的质量评价
如表1显示RCT中美国退伍军人管理局泌尿外科研究合作组(VACURG)[23,24]试验偏倚风险较高,而前列腺癌干预与对比研究(PIVOT)[14]和斯堪地那维亚前列腺癌研究4组(SPCG-4)[15,19-22]的偏倚风险分别为中度、低度;队列研究质量评价均在可接受范围。
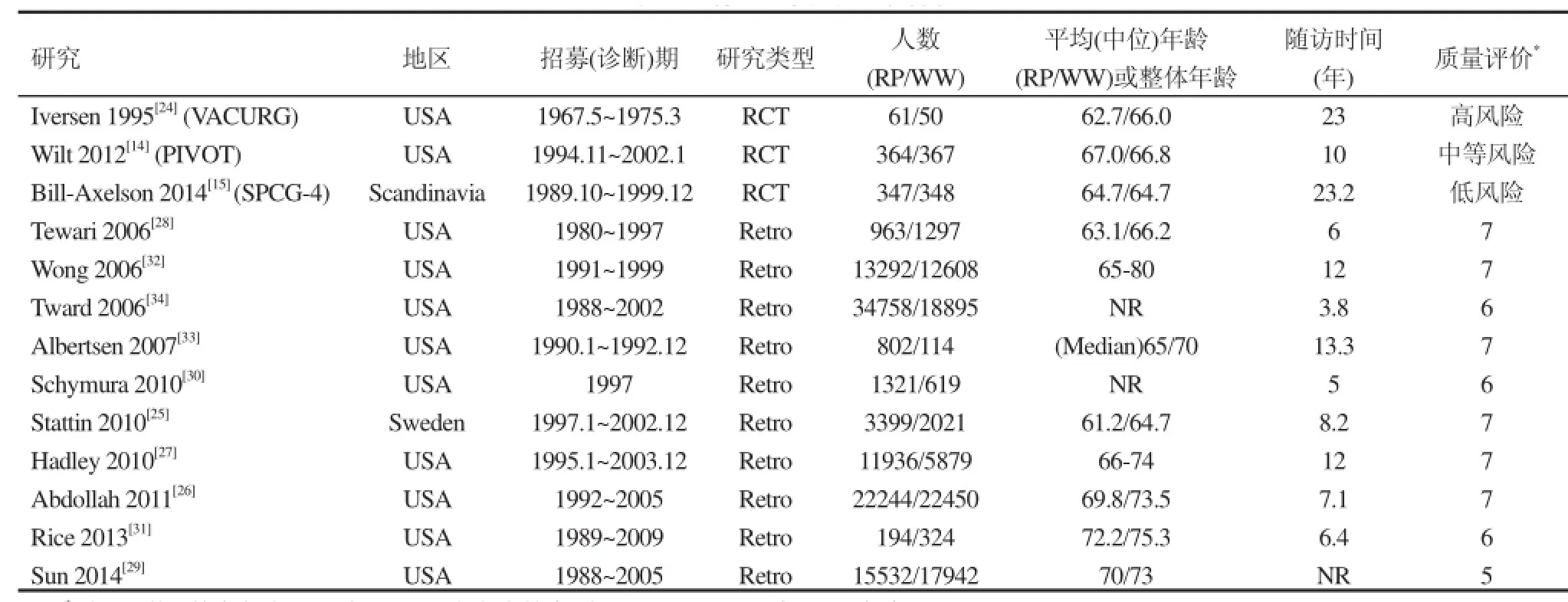
表1 纳入研究的基本特征

图1 文献筛选流程及结果
三、Meta分析结果
(一)总体死亡
3个RCT和8个队列研究的合并效应及11个研究的总体效应均显示RP对比WW显著减少总体死亡(ACM)风险HR=0.59 [95%CI(0.51,0.69),<0.00001],见图2。
(二)肿瘤特异死亡
2个RCT和7个队列研究的合成效应以及9个研究的总体效应均显示RP组前列腺癌特异死亡(CSM)要显著低于WW组 HR=0.43 [95%C(0.32,0.58),P<0.00001],见图3。
(三)敏感性分析
在Meta分析时发现,Iversen 1995[24]因年代太久、随访质量低而被敏感性剔除后,所有结果仍然显示不论RCT组还是非随机对照试验(NRCT)组、ACM还是CSM均显著支持RP(结果未展示)。
(四)发表偏倚
图4和图5显示合并效应中线两侧研究数量接近,无明显发表偏倚见。;在敏感性分析时的同样未见显著发表偏倚(漏斗图未给出)。
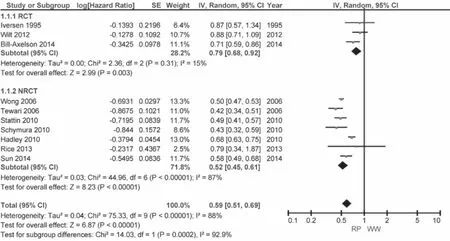
图2 总体死亡--研究类型分组
图3 前列腺癌特异死亡--研究类型分组
讨 论
对于早期局限性前列腺癌的保守治疗策略分为两类即“观察等待”和“主动监测”,两者的最大区别在于对疾病进展的处理策略,主动监测倾向于治愈性治疗方案如根治、放疗,而观察等待在疾病进展时往往予以姑息性处理如TURP、姑息性去势治疗;其次在随访中主动监测可能更多涉及穿刺活检。NCCN指南2014最新版指出主动监测(AS)适用于极低、低风险并且生存期望≥10年的早期前列腺癌患者,推荐监测频率PSA不低于6个月,直肠指检及穿刺活检不低于12个月,除非在有临床提示的情况下;而观察等待无特定的适应指证,一般在T1-2期且寿命期望<10年的可以考虑,也适用于各种治疗反应不佳的患者[10]。
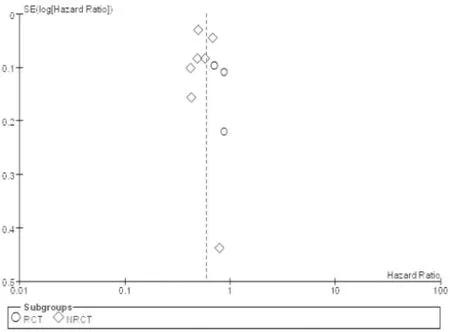
图4 总体死亡漏斗图
勃起功能障碍(ED)和尿路功能障碍是根治性手术的两大并发症,对于相对年轻人群及性生活需求显著的患者尤为重要。Bill-Axelson等[19]的研究报道手术后1年ED率58.1%,尿瘘率32.2%;对于ED目前提倡神经保留手术,保留神经有利于术后性功能的恢复[35],但保留神经手术带了来手术切缘肿瘤阳性率增加的风险[36],术后应用磷酸二酯酶-5型抑制剂有助于改善勃起功能及其恢复[37-39]。生活质量也是治疗方案选择的重要影响因素,研究表明手术后的生活质量RP对比WW明显变差[5,40,41],表现在性行为的不满意带来的心理障碍、社交活动的心理负担、焦虑、抑郁等方面。医疗费用也是值得考虑的另一个决定因素,保守治疗对比根治手术能够相对减少治疗费用[8]。
从本研究结果看来无论是总体死亡还是前列腺癌特异死亡,根治手术均优于观察等待。但其中两个十分重要的RCT结果却不尽相同,PIVOT实验结果显示不论ACM还是CSM,RP与WW的预后无显著差异,而SPCG-4在ACM和CSM上均显著支持RP。对于这两个研究结果的差异,有学者认为该差异是因为PIVOT是PSA时代的产物而SPCG-4研究在前PSA时代,从而PIVOT研究包含了更多的经PSA筛选的T1c期患者。另一方面,PSA带来的另一个影响是作为前列腺癌进展的监测指标,或许能有益于患者的管理而提高生存,但这两个研究的跟踪随访中均有PSA监测指标。Vuong等[42]对这两个研究比较分析后认为期望寿命以及随访时间的不同是PIVOT难以证实RP受益的重要原因。而Xia等[43]的假设分析认为PSA筛选时代的前置期和过度诊断是PIVOT显示很低绝对受益的原因,因而不能作为RP无效的有力证据。作者对这两个研究的随机化服从情况比较分析可以看出PIVOT研究中不服从随机到WW组(75/367)远高于SPCG-中的不服从率(30/348),P<0.0001;同样不服从随机到RP组比例PIVOT(83/364)比SPCG-4(54/347)却无显著差异,P=0.098。这可能是PIVOT无法显示出RP受益的重要原因。

图5 前列腺癌特异死亡漏斗图
本研究的局限性表现在纳入研究中仅3个RCT,且质量参差不齐,其余均为回顾性队列研究,同时纳入的队列研究中部分存在观察地区的交叉,这些可能造成不同程度的风险偏倚;另一方面,研究结果仅限于总体人群,因不同研究以不同分层方式报道亚组结果而无法进行亚组合成分析(比如不同肿瘤风险、Gleason评分、PSA水平等),亚组分析可能能够更加细致的探讨观察等待的适应人群。
本Meta分析结果提示:RP对总体和前列腺癌特异死亡均有显著优势,早期前列腺癌根治性切除可减少总体死亡及前列腺癌特异死亡风险,对于早期局限性前列腺癌选择观察等待应当十分慎重,治疗方案的选择需要结合患者其他因素综合考虑。
1 Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA:A Cancer Journal for Clinicians2013; 63(1): 11-30.
2 Xia J, Gulati R, Au M,et al. Effects of Screening on Radical Prostatectomy Eff cacy: The Prostate Cancer Intervention Versus Observation Trial.J Natl Cancer Inst2013; 105(8): 546-550
3 Loeb S, Bjurlin MA, Nicholson J,et al.Overdiagnosis and Overtreatment of Prostate Cancer.Eur Urol2014 65(6): 1046-1055
4 Bill-Axelson A, Garmo H, Holmberg L,et al. Long-termDistress After Radical Prostatectomy Versus Watchful Waiting in Prostate Cancer: A Longitudinal Study from the Scandinavian Prostate Cancer Group-4 Randomized Clinical Trial.Eur Urol2013; 64(6): 920-928
5 Johansson E, Steineck G, Holmberg L, et al. Long-term quality-of-life outcomes after radical prostatectomy or watchful waiting: the Scandinavian Prostate Cancer Group-4 randomised trial.Lancet Oncol2011; 12(9): 891-899
6 Steineck G, Helgesen F, Adolfsson J,et al. Quality of life after radical prostatectomy or watchful waiting.N Engl J Med2002; 347(11): 790-796
7 Perlroth DJ, Bhattacharya J, Goldman DP,et al. An Economic Analysis of Conservative Management Versus Active Treatment for Men with Localized Prostate Cancer.J Natl Cancer Inst Monogr2012; 2012(45): 250-257
8 Corcoran AT, Peele PB, Benoit RM. Cost Comparison Between Watchful Waiting With Active Surveillance and Active Treatment of Clinically Localized Prostate Cancer.Urology2010; 76(3): 703-707
9 Konety BR, Cowan JE, Carroll PR. Patterns of primary and secondary therapy for prostate cancer in elderly men: analysis of data from CaPSURE.J Urol2008; 179(5): 1797-1803
10 NCCN. NCCN Clinical Practice Guidelines in Oncology (Version I.2014): Prostate Cancer[EB/OL]. [2014-06-28]. http://www.nccn.org/professionals/physician_gls/pdf/ prostate.pdf.
11 Popiolek M, Rider JR, Andren O,et al. Natural History of Early, Localized Prostate Cancer: A Final Report from Three Decades of Follow-up.Eur Urol2013; 63(3): 428-435
12 Elliott SP, Meng MV, Elkin EP,et al. Incidence of urethral stricture after primary treatment for prostate cancer: data From CaPSURE.J Urol2007; 178(2): 529-534
13 Mottet N, Bastian PJ, Bellmunt J,et al. Guidelines on Prostate Cancer [EAU 2014][EB/OL]. [2014-06-28]. http://www.uroweb.org/guidelines/online-guidelines/ ?no_cache=1.
14 Wilt TJ, Brawer MK, Jones KM,et al.Radical Prostatectomy versus Observation for Localized Prostate Cancer.N Engl J Med2012; 367(3): 203-213
15 Bill-Axelson A, Holmberg L, Garmo H,et al. Radical prostatectomy or watchful waiting in early prostate cancer.N Engl J Med2014; 370(10): 932-942
16 Tierney JF, Stewart LA, Ghersi D,et al.Practical method for incorporating summary time-to-event data into metaanalysis.Trials2007; 8(1): 16
17 Ip S, Dahabreh IJ, Chung M,et al.An evidence review o active surveillance in men with localized prostate cancer.Evid Rep Technol Assess (Full Rep)2011; (204): 1-341
18 Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011][EB/OL]. http://www.handbook.cochrane.org/.
19 Bill-Axelson A, Holmberg L, Ruutu M,et al. Radical prostatectomy versus watchful waiting in early prostat cancer.N Engl J Med2011; 364(18): 1708-1717
20 Bill-Axelson A, Holmberg L, Ruutu M,et al. Radical prostatectomy versus watchful waiting in early prostate cancer.N Engl J Med2005; 352(19): 1977-1984
21 Holmberg L, Bill-Axelson A, Helgesen F,et al. A randomized trial comparing radical prostatectomy with watchfu waiting in early prostate cancer.N Engl J Med2002 347(11): 781-789
22 Bill-Axelson A, Holmberg L, Filen F,et al. Radical Prostatectomy Versus Watchful Waiting in Localized Prostate Cancer: the Scandinavian Prostate Cancer Group-4 Randomized Trial.J Natl Cancer Inst2008; 100(16): 1144-1154
23 Graversen PH, Nielsen KT, Gasser TC,et al. Radical prostatectomy versus expectant primary treatment in stages I and II prostatic cancer. A f fteen-year followup.Urology1990; 36(6): 493-498
24 Iversen P, Madsen PO, Corle DK. Radical prostatectomy versus expectant treatment for early carcinoma of the prostate. Twenty-three year follow-up of a prospectiv randomized study.Scand J Urol Nephrol Suppl1995; 172: 65-72
25 Stattin P, Holmberg E, Johansson J E,et al. Outcomes in Localized Prostate Cancer: National Prostate Cancer Register of Sweden Follow-up Study.J Natl Cancer Inst2010; 102(13): 950-958
26 Abdollah F, Sun M, Schmitges J,et al. Cancer-Specif c and Other-Cause Mortality After Radical Prostatectomy Versus Observation in Patients with Prostate Cancer: Competing-Risks Analysis of a Large North American Population-Based Cohort.Eur Urol2011; 60(5): 920-930
27 Hadley J, Yabroff KR, Barrett MJ,et al. ComparativeEffectiveness of Prostate Cancer Treatments: Evaluating Statistical Adjustments for Confounding in Observational Data.J Natl Cancer Inst2010; 102(23): 1780-1793
28 Tewari A, Raman JD, Chang P,et al. Long-term survival probability in men with clinically localized prostate cancer treated either conservatively or with definitive treatment (radiotherapy or radical prostatectomy).Urology2006; 68(6): 1268-1274
29 Sun M, Sammon JD, Becker A,et al.Radical prostatectomy vs radiotherapy vs observation among older patients with clinically localized prostate cancer: a comparative effectiveness evaluation.BJU Int2014; 113(2): 200-208
30 Schymura MJ, Kahn AR, German RR,et al. Factors associated with initial treatment and survival for clinically localized prostate cancer: results from the CDC-NPCR Patterns of Care Study (PoC1).BMC Cancer2010; 10: 152
31 Rice KR, Colombo ML, Wingate J,et al. Low risk prostate cancer in men >/= 70 years old: to treat or not to treat.Urol Oncol2013; 31(6): 755-760
32 Wong Y, Mitra N, Hudes G,et al.Survival Associated With Treatment vs Observation of Localized Prostate Cancer in Elderly Men.JAMA2006; 296(22): 2683-2693
33 Albertsen PC, Hanley JA, Penson DF,et al. 13-Year Outcomes Following Treatment for Clinically Localized Prostate Cancer in a Population Based Cohort.J Urol2007; 177(3): 932-936
34 Tward JD, Lee CM, Pappas LM,et al. Survival of men with clinically localized prostate cancer treated with prostatectomy, brachytherapy, or no definitive treatment-Impact of age at diagnosis.CANCER2006; 107(10): 2392-2400
35 Suardi N, Moschini M, Gallina A,et al.Nerve-sparing approach during radical prostatectomy is strongly associated with the rate of postoperative urinary continence recovery.BJU Int2013; 111(5): 717-722
36 Roder MA, Thomsen FB, Christensen IJ,et al. Risk factors associated with positive surgical margins following radical prostatectomy for clinically localized prostate cancer: can nerve-sparing surgery increase the risk?.Scand J Urol2014; 48(1): 15-20
37 Gandaglia G, Gallina A, Suardi N,et al. Preoperative erectile function is the only predictor of the use of a high number of phosphodiesterase type-5 inhibitors afte bilateral nerve-sparing radical prostatectomy.Int J Impot Res2014; 26(6): 201-204
38 Montorsi F, Brock G, Stolzenburg JU,et al.Effects of Tadalafil Treatment on Erectile Function Recovery Following Bilateral Nerve-sparing Radical Prostatectomy: A Randomised Placebo-controlled Study (REACTT).Eur Urol2014; 65(3): 587-596
39 Wang X, Wang X, Liu T,et al.Systematic review and meta-analysis of the use of phosphodiesterase type 5 inhibitors for treatment of erectile dysfunction following bilateral nerve-sparing radical prostatectomy.PLoS One2014; 9(3): e91327
40 Couper J W, Love A W, Dunai J V,et al. The psychologica aftermath of prostate cancer treatment choices: a comparison of depression, anxiety and quality of life outcomes over the 12 months following diagnosis.Med J Aust2009; 190(7 Suppl): S86-S89
41 Litwin MS, Lubeck DP, Spitalny GM,et al. Mental health in men treated for early stage prostate carcinoma.Cancer2002; 95(1): 54-60
42 Vuong W, Sartor O, Pal S. Management of localized prostate cancer: the pendulum swings (back to the middle).Asian J Androl2014; 16(4): 570-571
43 Xia J, Gulati R, Au M,et al.Effects of Screening on Radica Prostatectomy Eff cacy: The Prostate Cancer Intervention Versus Observation Trial.J Natl Cancer Inst2013; 105(8): 546-550
(2014-08-30收稿)
Radical prostatectomy versus watchful waiting for clinically localized prostate cancer: A Meta-Analysis
Luo You, Fu Shengjun, Wang Zhiping, Yang Li*Department of Urology, Lanzhou University Second Hospital; Institute of Urology, Lanzhou University Second Hospital; Institute of Gansu Nephro-Urological Clinical Center; Key laboratory of urological disease of Gansu province, Lanzhou
730000, China
Yang Li, E-mail: yuze250@163.com
ObjectiveTo compare the survival effect of clinically localized prostate cancer treated by radical prostatectomy (RP) and watchful waiting (WW) .MethodsRandomized controlled trials or observational studies were searched from database of Medline, Cochrane Library, ISI web of knowledge and SinoMed for the evaluation of prognosis of clinically localized prostate cancer treated by RP versus WW. Prognosis evaluation parameter included all-cause mortality and prostate cancer specif c mortality. The latest retrieval date was July 2014. The data extraction and the quality assessment of included studies were independently conducted by 2 reviewers. RevMan5.2 software was used to perform data synthesis.Results3 RCTs involving 1 537 patients (772 RP versus 765 WW) and 10 retrospective cohort studies involving 186 590 patients (104441 RP versus 82149 WW) were enrolled f nally. The results of meta-analysis showed that both the hazard of allcause mortality and prostate cancer specif c mortality in RP group were signif cantly lower than that of WW group, all-cause mortality risk was HR=0.59 [95%CI (0.51, 0.69),P<0.00001], and prostate cancer specif c mortality risk was HR=0.43 [95%CI (0.32, 0.58),P<0.00001]. All outcomes favored radical prostatectomy regardless of study type stratification.ConclusionRadical prostatectomy reduces the hazard of all-cause mortality and cancer specif c mortality of clinically localized prostate cancer, which may push more deliberations when physicians take watchful waiting in consideration.
prostatic neoplasms/surgery; survival analysis; review, systematic; Meta-analysis
10.3969/j.issn.1008-0848.2014.12.005
R 737.25
*通讯作者, E-mail: yuze250@163.com