Correlation of expression of STAT3, VEGF and differentiation of Th17 cells in psoriasis vulgaris of guinea pig
Xiu-Fen Zheng, Yue-Dong Sun, Xue-Yan Liu
1Department of Dermatology, South Hospital, Southern Medical University, Guangzhou 510000, China
2Department of Dermatology, Zhujiang Hospital, Southern Medical University, Guangzhou 510000, China
Correlation of expression of STAT3, VEGF and differentiation of Th17 cells in psoriasis vulgaris of guinea pig
Xiu-Fen Zheng1*, Yue-Dong Sun2, Xue-Yan Liu1
1Department of Dermatology, South Hospital, Southern Medical University, Guangzhou 510000, China
2Department of Dermatology, Zhujiang Hospital, Southern Medical University, Guangzhou 510000, China
Objective: To investigate the role of T help 17 cells (Th17) and STAT3-VEGF pathway in pathogenesis of psoriasis. Methods: A total of 50 cases of psoriasis guinea pigs and 20 normal guinea pigs were selected. The ratio of Th17/ IL-17 cell in peripheral blood were detected by flow cytometric analysis; STAT3 and VEGF concentrations were measured by immunohistochemistry and Western blot. Results: The expression of Th17 in peripheral blood were significantly increased in psoriasis [(1.76±0.88)%] compared with controls [(0.48±0.27)%] (P<0.05). Th17 related cytokine STAT3 and VEGF were significantly increased in psoriasis compared with controls (P<0.05), and were positively correlated the expression of Th17. Conclusions: The expressions of Th17, STAT3 and VEGF are elevated in psoriasis, which suggests Th17 cells have a potential role in the pathogenesis of psoriasis by STAT3-VEGF pathway.
ARTICLE INFO
Article history:
Received 10 September 2013
Received in revised form 15 October 2013
Accepted 15 December 2013
Available online 20 April 2014
Psoriasis
1. Introduction
Psoriasis vulgaris (Hereinafter referred to as psoriasis) is a common chronic inflammatory proliferative skin disease, and the etiology and pathogenesis are still not clear. More and more studies suggest that its pathogenesis is caused by multiple genes together, in which CD4+T lymphocytes immune dysfunction plays an important role in the pathogenesis. Most traditional researches focus on T help (Th) 1 cells, but in recent years studies suggest that the cytokines of Th17 cells play an important role in the pathogenesis of psoriasis. In this study, immunohistochemical assay, Western blot and flow cytometry analysis were used to detect the STAT3, VEGF, Th17 expression in guinea pigs, to explore the correlation between the psoriasis and the STAT3-VEGF pathway and Th17 cells.
2. Materials and methods
2.1. Establishment of psoriasis model
A total of 70 health guinea pigs were selected, including 20 as the control group, 50 as the model group. Skin of back ear was treated topically with 5% propranolol emulsion, 0.3 mL/time, 3 times/day for 2 weeks. Pigs in the control group were treated with saline. HE staining evaluation revealed successful models.
2.2. Reagents and instruments
Rabbit anti-mouse STAT3, VEGF polyclonal antibody kits, SP and DAB immunohistochemical kit were purchased from Santa-Cruz Company. Rabbit anti-mouse STAT3, VEGF monoclonal antibody were purchased from Thermo Electron Corporation, fluorescent-labeled goat anti-mousesecondary antibody were purchased from gene company. Human lymphocyte separation medium was purchased from Fuzhou Maixin Biotechnology Co., Ltd. Total protein extraction kit was purchased from Invitrogen Corporation. Rotary slicer machine was purchased from Shanghai Yuejin Medical Instrument, flow cytometry was purchased from American BD Biosciences.
2.3. Methods
The lesion tissue of psoriatic guinea pig and skin of back ear of normal guinea pigs was obtained. Then all guinea pigs were sacrificed, and the blood sample was taken from medial canthus vein into the heparin sodium anticoagulative tube.
All skin specimens were divided into two parts. Part of the skin tissues were fixed in 10% formalin. After dehydration, embedding and cutting into sections, immunohistochemical SP method and DAB color were performed. Antigen retrieval under high temperature and pressure was carried out in all specimens, and the staining was performed according to the instructions. A total of 50 mg tissue was obtained from another part and then was detected by Westernblotting. Total protein was extracted. 30 μg total protein was transferred, and BSA blocked. Mouse anti-human STAT3 and VEGF monoclonal antibody were added and incubated overnight. They were washed, then were added with fluorescence-labeled goat anti-mouse second antibody. They were observed under fluorescence scanning system. Two mL venous blood were extracted, and was mixed with 150 μL anticoagulant and 150 μL RPMI1640 cell culture fluid. The cell concentration was adjusted to 2×106/mL. They were inoculated and cultured at 37 ℃ in 5% CO2cell incubator for 4 h. They were washed twice with PBS, and then added with permeabilization wash buffer. After supernatant were removed, 0.5 μg FITC-labeled IL-17 staining was added. They were incubated free of light at 4 ℃ for 30 min, and centrifugated at 1 000 rpm for 5 min, then supernatant were abandoned. Cells were resuspended by 300 μL PBS, and the proportion of Thl7 cells were detected with flow cytometry.
2.4. Results determination
Results were determined by the double-blind method. Brown particles in the cytoplasm and/or nucleus were considered as positive cells of STAT3, while brown particles in the cytoplasm were considered as positive cells of VEGF. Five typical slices were selected and observed under 400 × magnification. At least 1 000 cells were counted, and were calculated by the percentage of positive cells. Cells positive level <25% were considered as negative (-), 25%-75% as the positive (+), above 75% as strongly positive (+ +). The grayscale integral value of each stripe was recorded, statistical analysis was conducted by sample integral value/ internal reference integral value ratio.
2.5. Statistical analysis
The data was analyzed with SPSS 13.0 software. Data were expressed as mean±SD values. The significantly difference between two groups were compared with t test. Correlation was analyzed with the Speraman correlation analysis and linear correlation analysis.
3. Results
3.1. STAT3 and VEGF protein immunohistochemical expression in psoriasis guinea
STAT3 positive expression of psoriasis guinea pigs was 46% (23/50), significantly higher than the normal control group 25% (5/20) (Χ2=4.220, P=0.040). VEGF positive expression of psoriasis guinea pigs was 74% (37/50), significantly higher than the normal control group 40% (8/20) (Χ2=10.611, P=0.001) (Table 1).
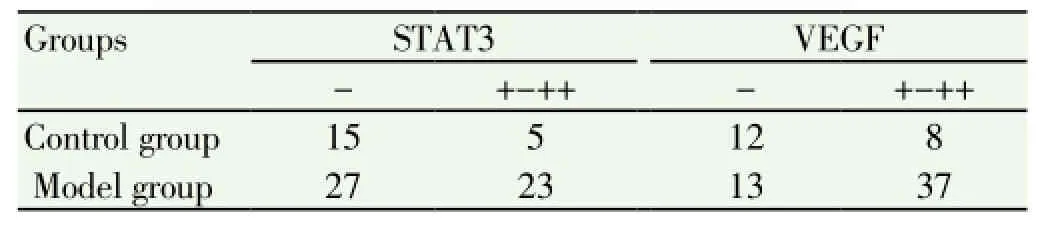
Table 1 STAT3 and VEGF expression in psoriasis guinea pigs.
3.2. Western blot detection of STAT3 and VEGF protein expression in psoriasis guinea pigs
Westem-blotting results showed that in 50 cases of psoriasis guinea pig tissues, the relative expression of STAT3 (STAT3/β-actin) was 2.26±0.54, significantly higher the expression of STAT3 in normal tissue [(0.79±0.22)] (P<0.05). The relative expression of VEGF (VEGF/β-actin) was (1.62 ±0.29), significantly higher than the expression of VEGF in normal tissue [(1.07±0.33)] (P<0.05) (Figure 1).

Figure 1. STAT3, VEGF protein expression.
3.3. Proportion of Th17 cells in peripheral blood
The percentage of Th17 cells in psoriasis guinea pigs was (1.76±0.88)%, significantly higher than the normal control group [(0.48±0.27)%] (P<0.05).
3.4. Correlation of STAT3, VEGF and Th17 cells expression in psoriatic guinea pigs
The statistical analysis showed that the expression of Th17 cells was positively correlated with the pathogenesis of psoriasis (P<0.05,r=0.784), and the expression of Th17 cells in peripheral blood were positively correlated with the STAT3, VEGF protein levels (P<0.05,r=0.665,r=0.684), SSTAT3 and VEGF expression was positively correlated (P<0.05,r=0.647).
4. Discussion
Psoriasis is a common chronic inflammatory skin disease. The incidence rate is high and it is difficult to completely cured. It often affects the young adults[1]. The specifically pathogenesis of psoriasis is still unclear, some studies showed that psoriasis is a inflammatory disease caused by the infiltration of T lymphocyte on the skin which were of persistent existence and recurrent episodes[2,3]. STAT3 signaling pathway is correlated with the cell growth, proliferation and apoptosis, sustained activation of STAT3 can lead to abnormal cell proliferation and malignant transformation. Studies have shown that in human psoriasis, the STAT3 activation is specific[4-6].
Feng et al[5] detected the expression of stat3 and survivin of 52 cases psoriasis by immunohistochemical assay. They considered that stat3 may upregulate the survivin expression then induce the cell proliferation of the psoriatic lesional skin. VEGF is a vascular-specific activity factor. It has a strong function and can be specific for the mitogen of endothelial cells[7] and beneficial to increase vascular permeability. STAT3 can directly regulate the expression of VEGF, and can also indirectly regulate the expression of VEGF. Ye et al[13-15] detected the interleukin IL-17, IL-23, IL-6 and transforming growth factor-β (TGF-β) levels of the psoriasis guinea pig, the result showed high expression of IL-23, IL-6 and TGF-β in the psoriasis guinea pigs. And IL-23 levels were positively correlated with PASE. Th17 cells may correlate with the pathogenesis of psoriasis. So, Th17 cells can play an important role in the pathogenesis of psoriasis by the inflammatory reaction mediated as the psoriasis characteristic T lymphocyte population. Studies showed that STAT3 can induce cell immune response by stimulating the Th17 to secret IL-23[8-12].
In this study, the immunohistochemical assay showed that the positive expression rate of STAT3 and VEGF protein in psoriasis guinea pigs were 46% (23/50), 74% (37/50), both higher than the normal control group. STAT3 is mainly expressed in the cytoplasm and nucleus of whole layer or the middle and lower layer of the epidermis as the pale yellow to brown granules. A small amount is also expressed in some endothelial cells of dermal vascular, but with small or micro-expression in the basal cytoplasm of normal epidermis. VEGF is expressed as pale yellow to brown granules in the basal layer to the granular layer forming cells cytoplasm, but with micro-expression or no expression in the normal epidermis. Meanwhile Western detection showed that the STAT3 and VEGF protein has a high expression in psoriasis vulgaris, which were higher than the normal control group, and the difference was statistically significant.
STAT3 and VEGF expression was positively correlated (P<0.05,r=0.647), which showed that STAT3-VEGF signaling pathways are involved in the pathogenesis of psoriasis. Flow cytometry was used to detect the expression of PBMCTh17 cells in peripheral blood, the results showed that the percentage of the Th17 cells expression in psoriasis guinea pigs were significantly higher than normal control group. That suggested Th17 may play an important role in the psoriasis vulgaris inflammatory injury. Furthermore, this study also found that Th17 cells was positively correlated with the pathogenesis of psoriasis expression (P<0.05,r= 0.784), and the expression of Th17 cells in peripheral blood was positively correlated with STAT3, VEGF protein expression (P <0.05,r= 0.665,r= 0.684). That is, increase in STAT3, VEGF expression in psoriatic lesions can increase the expression of Th17. Thus we speculate that STAT3-VEGF signaling pathway activation can participate in Th17 cell differentiation, which can induce Th17 overexpression and causes the skin’s inflammatory response[16-20], resulting inthe pathogenesis of psoriasis.
In summary, STAT3, VEGF, and Th17 have close correlation with the pathogenesis of psoriasis. After some stimulation of the cell, STAT3 is phosphorylated and bound to the promoter region of downstream gene VEGF, which can promote the overexpression of VEGF, thereby enable the over differentiation of Th17 cells with an active function, resule in the occurrence of psoriasis. So, this pathway may be an important target for therapeutic intervention of psoriasis.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Zhao B. Clinical dermatology. Jiangsu: Science and Technology Press; 2001, p. 762-764.
[2] Chang SX, Chen YF. Th17 cells and psoriasis. Skin STD J Neurol 2010; 17(1):71-74.
[3] Yan XS, Feng YS. Research progress of Th17 cells and silver crumbs disease. Heilongjiang Med J 2009; 22(4): 461-463.
[4] Huang H, Liu Hj, Tu YT. The expression of transcriptional activation factor - 3 and vascular endothelial growth factor in ordinary psoriasis skin. Chin J Dermatol 2007; 40(3): 175-176.
[5] Feng SJ, Gao SJ, Li HR, Ma J, Li P. The expression of Stat3 and Survivin in the lesions of psoriasis vulgaris and their correlation. Hebei Med J 2012; 34(2): 165-166.
[6] Creamer D, Sullivan D, Bicknell R, Barker J. Angiogenesis in psoriasis. Angiogenesis 2002; 5(4): 231-236.
[7] Xu Q, Briggs J, Park S, Niu G, Kortylewski M, Zhang S, et al. Targeting Stat3 blocks both HIF-1α and VEGF expression induced by muhiple oneogenic growth signaling pathways. Oncogene 2005; 24(36): 5552-5560.
[8] Chen X, Liu ZX, Wu Y, Liu HJ, Li JW. Expression of the cytokines associated with Th17 cell in the psoriatic lesions. Chin J Leprosy Skin Dis 2008; 24(3): 176-178.
[9] Lowes MA, Kikuchi T, Fuentes-Duculan J, Cardinale I, Zaba LC, Haider AS, et al. Psoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cells. J Invest Dermatol 2008; 128(5): 1207-1211.
[10] Zhong DQ, Lin L, Luo Q. The expression and clinical significance of guinea pigs peripheral blood psoriasis vulgaris Th17 cells. Skin Venereal Dis Diagnostics 2012; 19(3): 154-156.
[11] Kagami S, Rizzo HL, Lee JJ, Koguchi Y, Blauvelt A. Circulating Th17, Th22, and Th1 cells are increased in psoriasis. J Invest Dermatol 2010; 130(5):1373-1383.
[12] Zheng DC, Chang SX, Huang LN. Using Quantum Dots Doublelable Immunofluorescence to Study Skin Lesions Localization of Th17 Cells in Psoriatic Patients. Skin STD J Neurol 2011; 18(2): 97-99.
[13] Ye P, Huang WL, Zheng L. A research on correlation between Th17 related cytokines and psoriasis vulgaris. Chongqing Med 2013; 42(15): 1706-1710.
[14] Miossec P. IL-17 and Thl7 cells in human inflammatory diseases. Microbes Infect 2009; 11(5): 625-630.
[15] Meglio P, Dicesare A, Laggner U, Chu C-C, Napolitano L, Villanova F, et al. The IL23R R381Q gene variant protects against immune-mediated diseases by impairing IL-23-induced Th17 effector response in humans. PLoS One 2011; 6(2) e17160.
[16] Durant L, Watford WT, Ramos HL, Laurence A, Vahedi G, Wei L, et al. Diverse targets of the transcription factor STAT3 contribute to T cell pathogenicity and homeostasis. Immunity 2010; 32(5): 605-615.
[17] Liu JK, Duan YZ, Cheng XM, Xie W, Long HX, Lin ZH, et al. IL-17 is associated with poor prognosis and promotes angiogenesis via stimulating VEGF production of cancer cells in colorectal carcinoma. Biochem Biophysical Res Comm 2011; 407(10): 348-354.
[18] Nishihara M, Ogura H, Ueda N. IL-6-gp130-STAT3 in T cells directs the development of IL-17+Th with a minimum effect on that of Treg in the steady state. Int Immunol 2007; 19(6): 695-702.
[19] Yang HL, GuoYZ, Sun R. Expression of PSTAT3 and VEGF and its significance in psoriasis vulgaris. Chin Med Guide 2012; 8(34): 194-197.
[20] Kagami S, Rizzol HL, Lee JJ, Koguchi Y, Blauvelt A. Circulating Th17,Th22,and Th1 cells are increased in Psoriasis. J Invest Dermatol 2010; 130(5): 1373-1383.
ment heading
10.1016/S1995-7645(14)60046-8
*Corresponding author: Xiu-Fen Zheng, M.M., Department of Dermatology, South Hospital, Southern Medical University, Guangzhou 510000, China.
Tel: 13425825180
E-mail: xiufenggogo@126.com
Foundation project: It is supported by Guangdong Medical Research Project (No B2012240).
T help 17 cells
STAT3-VEGF pathway
 Asian Pacific Journal of Tropical Medicine2014年4期
Asian Pacific Journal of Tropical Medicine2014年4期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Effect of bone marrow mesenchymal stem cells on the Smad expression of hepatic fibrosis rats
- Effect of anesthesia on cognitive status and MMP-2 expression in rats
- Ultrasonic diagnosis and vasoactive substances examination in patients with cirrhosis
- Effect of low intensity pulsed ultrasound on repairing the periodontal bone of Beagle canines
- Effect of RSCs combined with COP-1 on optic nerve damage in glaucoma rat model
- Expression of PI3-K, PKB and GSK-3β in the skeletal muscle tissue of gestational diabetes mellitus
