改良无管化经皮肾镜碎石取石术治疗2~3cm肾下盏结石后肾下盏解剖结构的变化及对术后清石率的影响
【摘 要】目的:探讨改良无管化经皮肾镜碎石取石术(percutaneous nephrolithotomy,PCNL)治疗2~3 cm肾下盏结石后肾下盏解剖结构变化及对术后清石率的影响。方法:选取2020年9月至2023年9月西南医科大学附属医院泌尿外科收治的300例2~3 cm肾下盏结石患者作为研究对象,经改良无管化PCNL治疗术后疗效将患者分为清除组(n=253)和残余组(n=47),对2组患者一般资料进行单因素分析,采用限制性三次样条回归法分析肾下盏解剖结构参数变化与术后结石残余的关系;采用逐步logistic回归分析进行影响因素分析,并基于此构建列线图预测模型,绘制校准曲线、受试者工作特征(receiver operating charac? teristic,ROC)曲线对模型的诊断效能进行评估。结果:2组患者在肾功能不全史(P=0.017)、肾下盏长度(infundibular length,IL)(P<0.001)、结石数量(P=0.025)、结石CT值(P=0.001)、肾下盏宽度(infundibular width,IW)(P<0.001)、手术时间(P=0.002)、肾盂漏斗部夹角(infundibulopelvic angle,IPA)(P<0.001)、肾盂肾下盏高度(pelvic caliceal height,PCH)(P<0.001)、血尿酸(uric acid,UA)(P<0.001)、尿素氮(blood urea nitrogen,BUN)(P=0.014)方面差异有统计学意义(P<0.05);logistic回归显示调整后IL、PCH、IW、IPA仍是术后结石残余的危险因素;逐步logistic回归分析结果显示结石数量、结石CT值、IL、PCH是影响患者经改良无管化PCNL治疗肾下盏结石残余的独立危险因素,IW、IPA是保护因素(均P<0.05);利用以上影响因素进行列线图预测模型构建,得到回归方程为Logit(P)=-2.567+0.110 9×X1+1.170×X2-0.226×X3+0.023×X4-0.442×X5+0.714×X6,其一致性指数0.893(95%CI=0.878~0.901),ROC曲线分析显示,模型AUC为0.888(95%CI=0.869~0.897),灵敏度为0.827,特异度为0.795,区分度较好;校准曲线提示该模型准确度较高。结论:改良无管化PCNL治疗2~3 cm肾下盏结石是一种安全有效的方法,肾下盏结石患者可通过充分考虑解剖结构方面影响因素进行合理制定治疗方案,从而进行针对性预防,提高患者术后结石清除率。
【关键词】改良无管化经皮肾镜碎石取石术;2~3 cm肾下盏结石;肾下盏解剖结构;清石率;影响
【中图分类号】R699【文献标志码】A【收稿日期】2023-12-05
基金项目:四川省卫生和计划生育委员会科研课题资助项目(编号:XNYK-201801-69)。
Changes in the anatomical structure of the lower renal calyx after the treatment of 2-3 cm lower renal calyx stones with improved tubeless percutaneous nephrolithotomy and impact on postoperative stone clearance rate
Wu Tao,Wang Liang
(Department of Urology,Affiliated Hospital of Southwest Medical University)
【Abstract】Objective:To investigate the changes in the anatomical structure of the lower renal calyx after the treatment of 2-3 cm lower renal calyx stones with improved tubeless percutaneous nephrolithotripsy(PCNL) and impact on postoperative stone clearance rate. Methods:A total of 300 patients with 2-3 cm lower renal calyx stones admitted to the Department of Urology,Affiliated Hospital of Southwest Medical University between September 2020 and September 2023 were selected as the study subjects. After improved tubeless PCNL treatment,the patients were divided into clearance group(n=253) and non-clearance group(n=47). Univariate analysis was performed on the general information of two groups of patients. The restricted cubic spline regression method was used to analyze the relationships between changes in anatomical parameters of the lower renal calyx and postoperative stone residue. Stepwise logistic regression was conducted to analyze influencing factors. Based on this,a nomogram prediction model was constructed. The receiver op? erating characteristic curve and calibration curve were drawn to evaluate model diagnostic effectiveness. Results:There were signifi? cant differences between the two groups in history of renal dysfunc?tion(P=0.017),infundibular length(P<0.001),number of stones(P=0.025),CT value of stones(P=0.001),infundibular width(P< 0.001),surgical time(P=0.002),infundibulopelvic angle(P<0.001),pelvic calyceal height(P<0.001),uric acid(P<0.001),and blood urea nitrogen(P=0.014). Logistic regression showed that adjusted infundibular length,pelvic calyceal height,infundibular width,and infundibulopelvic angle were still risk factors for postoperative stone residue. The results of stepwise logistic regression showed that the number of stones,CT value of stones,infundibular length,and pelvic calyceal height were independent risk factors affecting lower renal calyx stone residue in patients treated with improved tubeless PCNL,while infundibular width and infundibulopelvic angle were protec? tive factors(P<0.05). The influencing factors mentioned above were used to construct a nomogram prediction model. The regression equation was:Logit(P)=-2.567+0.110 9×X1+1.170×X2-0.226×X3+0.023×X4-0.442×X5+0.714×X6,with a consistency index of 0.893(95%CI=0.878-0.901). The receiver operating characteristic curve showed that the area under the curve was 0.888(95%CI=0.869-0.897),the sensitivity was 0.827,and the specificity was 0.795,indicating high discrimination ability. The calibration curve indicated that the model had high accuracy. Conclusion:Improved tubeless PCNL is a safe and effective method for the treatment of 2-3 cm lower renal calyx stones. Patients with lower renal calyx stones should fully consider anatomical factors before formulating treatment plans,and targeted preventive measures should be taken in clinical practice to increase the stone clearance rate after PCNL surgery.
【Key words】improved tubeless percutaneous nephrolithotripsy;2-3 cm lower renal calyx stones;anatomical structure of the lower re? nal calyx;stone clearance rate;influence
泌尿系结石在泌尿系统相对比较常见,多会引起血尿、感染、腰疼及肾功能下降,甚至是肾衰竭,且易反复[1]。研究显示在泌尿系结石发病率中肾结石大约为40%~50%,而肾结石中肾下盏结石约占36%。其治疗方法是从肾脏取出结石,去除病灶,进而解除结石造成的梗阻,以达到对肾功能的保护[2-3]。近年来,随着医疗水平逐渐地提升,经皮肾镜碎石术(percutaneous nephrolithotomy,PCNL)因其手术创伤相对较小、术后康复快、临床疗效好等优势在临床治疗肾结石中可作为首选手段,但是肾下盏结石由于肾脏独特的解剖等因素,与其他部位相比其治疗效果并不是十分满意,特别是对于2~3 cm肾下盏结石患者,PCNL术后仍有部分结石未清除,需要进行再次手术以及其他后续治疗,并且PCNL在治疗过程中采用的鞘管相对较大,容易引起术后出血、疼痛、住院时间长等并发症,严重影响其生活质量[4-6],但近年随着无管化PCNL的开展,已经较大程度地降低了这些并发症的发生,但其在清除2~3 cm肾下盏结石方面疗效尚不确定,因此,本研究选取西南医科大学附属医院300例2~3 cm肾下盏结石患者进行研究,旨在探讨改良无管化PCNL治疗2~3 cm肾下盏结石后其肾下盏解剖结构变化及对术后清石率的影响,为临床诊断治疗提供参考依据。
1 资料与方法
1.1 研究对象
选取2020年9月至2023年9月本院泌尿外科收治的 300例2~3 cm肾下盏结石为患者作为研究对象,经改良无管化PCNL治疗术后疗效将患者分为清除组(n=253)和残余组(n=47)。其中清除组男性137例,女性116例,年龄26~66岁,平均年龄(45.45±15.00)岁,残余组男性29例,女性18例,年龄27~67岁,平均年龄(48.32±12.95)岁。研究对象均已签署知情同意书,项目通过伦理审查委员会批准(编号:ZYGZY2020-LL-03)。
1.2 纳排标准
纳入标准:①符合肾下盏结石的诊断标准且结石直径为2~3 cm;②年龄≥18岁;③术后行常规抗感染治疗;④尽量为本地区患者、依从性好,临床资料完整。排除标准:①术侧泌尿系既往手术史;②合并肾肿瘤、肾结核者;③手术中止、更改手术方式者;④处于妊娠阶段者。
1.3 方法
1.3.1 一般资料收集 通过电子病历单收集患者一般资料及生化指标,包括体质指数(body mass index,BMI)、性别、年龄、既往史(高血压等)等指标。
1.3.2 实验室指标检查 所有研究对象禁食8~12 h,次日晨空腹抽取肘静脉血8 mL,送检验科化验。采用自动生化分析仪(日立7150,日本东京)检测血浆总胆固醇(total choles? terol,TC)、高密度脂蛋白胆固醇(high density lipoprotein cho? lesterol,HDL-C)、三酰甘油(triglyceride,TG)、低密度脂蛋白胆固醇(low density lipoprotein cholesterol,LDL-C)指标;采用全自动血液分析仪(曼库尔特DxH800,美国贝克)检测白细胞计数(white blood cell count,WBC);采用酶联免疫吸附(enzyme-linked immunosorbent assay,ELISA)法检测血尿酸(uric acid,UA)、尿素氮(blood urea nitrogen,BUN)水平,所有操作依据试剂盒说明进行。
1.3.3 治疗方法 所有研究对象均行改良无管化PCNL治疗,取截石卧位,在输尿管镜、膀胱镜下行患侧输尿管置5 Fr输尿管导管,并留置20 Fr三腔气囊尿管,固定好输尿管导管,然后接输液器,并改体位为俯卧位,垫高腹部以固定肾脏,结合术前CT分析、术中彩超定位穿刺点,在彩超引导下,采用两步穿刺法穿刺,成功后置入0.032英寸斑马导丝,进行皮肾通道建立。沿经皮肾通道剥皮鞘置入9.5 Fr输尿管镜或肾镜,并及时调整灌注泵压力、流速,确保视野足够清晰并寻找结石,使用15~40 W功率钬激光碎石并冲洗出、钳取结石碎片,不放置造瘘管,采用无管化,拔出操作鞘并进行穿刺切口缝合。
1.4 观察指标
肾下盏解剖结构参数包括肾下盏长度(infundibular length,IL)、肾盂漏斗部夹角(infundibulopelvic angle,IPA)、肾下盏宽度(infundibular width,IW)、肾盂肾下盏高度(pel? vic caliceal height,PCH),具体计算及测量方法如下,IPA:肾盂中轴与结石所在下盏中轴交界处的内夹角;IL:肾下盏最远端至肾盂下极中心点的距离;IW:肾下盏漏斗部最窄处的距离;PCH:肾下盏底部水平至肾盂下极中心点的垂直距离[7-8],见图1。本研究中PCNL术后8周行泌尿系统X线片或CT检查,未见残余结石或残余结石最大径≤4 mm定义为结石清除组,否则为残余组。

1.5 统计学方法
采用SPSS 22.0统计软件统计对所有数据进行分析。计数资料以例数(百分比)表示,采用χ2检验;计量资料用均数±标准差(x±s)表示,采用t检验。影响因素采用逐步logistic回归分析,列线图预测模型采用R3.3.2软件和rms软件包构建。采用校准曲线、受试者工作特征(receiver operating characteristic,ROC)曲线分别评价模型的准确度和区分度。检验水准α=0.05。采用受限三次样条拟合logistic回归模型探索潜在的非线性关联,如果模型χ2的P≤0.01,则假定样条函数有效。检验水准α=0.05。
2 结 果
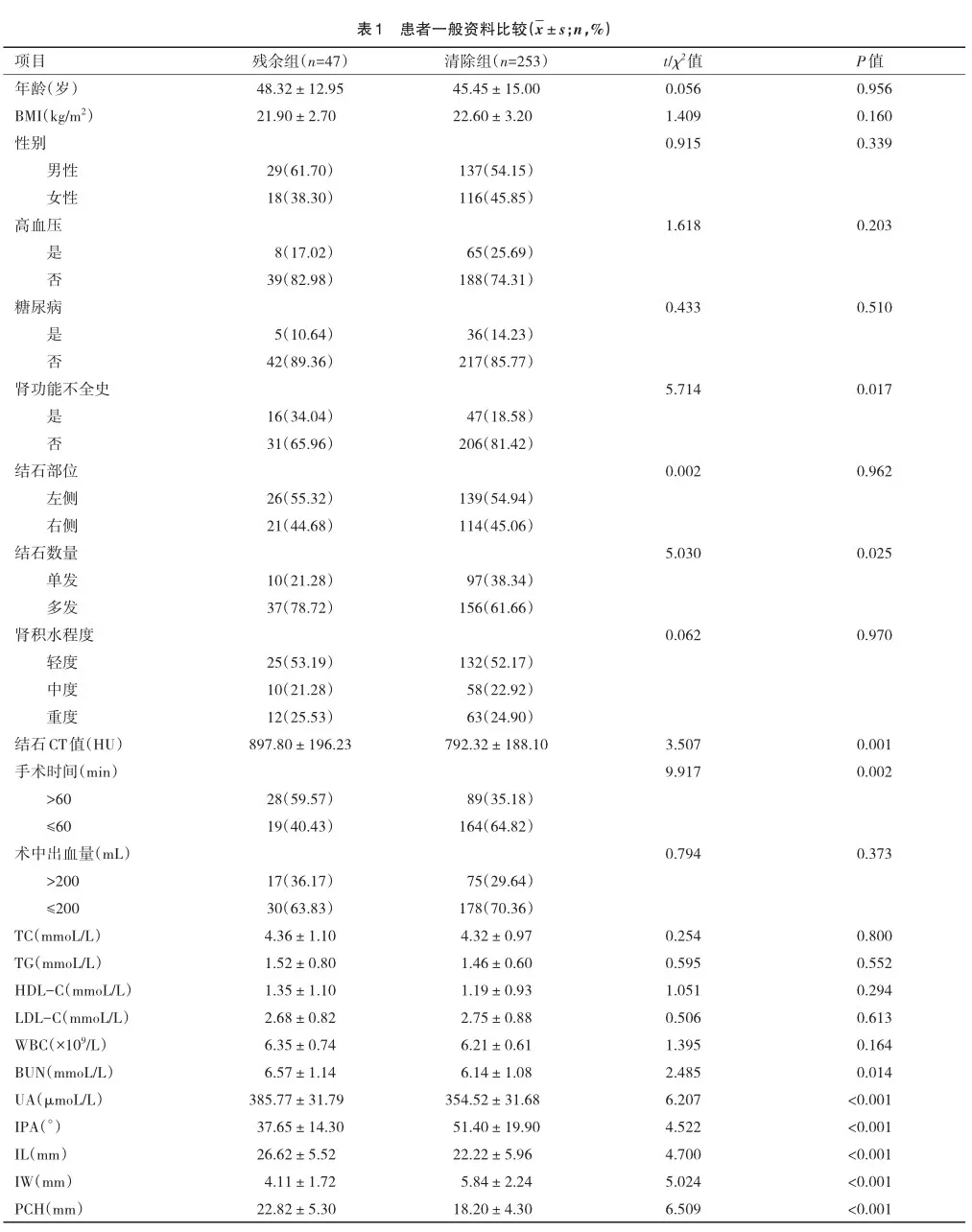
2.1 2组患者一般资料对比
2 组患者肾功能不全史比例(χ2=5.714,P=0.017)、手术时间长(χ2=9.917,P=0.002)、多发结石(χ2=5.030,P=0.025)明显提高,结石CT值(t=3.507,P=0.001)、IL(t=4.700,P< 0.001)、PCH(t=6.509,P<0.001)、UA(t=6.207,P<0.001)、BUN(t=2.485,P=0.014)明显增加,IW(t=5.024,P<0.001)、IPA(t= 4.522,P<0.001)明显减低,差异有统计学意义;其余指标 2组比较差异均无统计学意义(P>0.05),见表1。
2.2 肾下盏解剖结构参数变化与术后结石残余的独立相关性
将肾下盏解剖结构参数(IL、IW、PCH及IPA)作为分类变量和连续变量2种方式探讨其与术后结石残余的相关性,结果显示,在未校正logistic回归模型中,IL、IW、PCH、IPA与术后结石残余显著相关,经调整年龄,性别等因素后(模型2)IL、PCH、IW、IPA仍是术后结石残余的危险因素,见表2。
2.3 肾下盏解剖结构参数变化与术后结石残余风险之间的非线性关联
为了证明肾下盏解剖结构参数变化与术后结石残余风险之间的非线性关联,本研究采用限制性三次样条针对总样本绘制OR和95%CI的图,结果表明肾下盏解剖结构参数变化与术后结石残余呈明显的相关性,见图2。
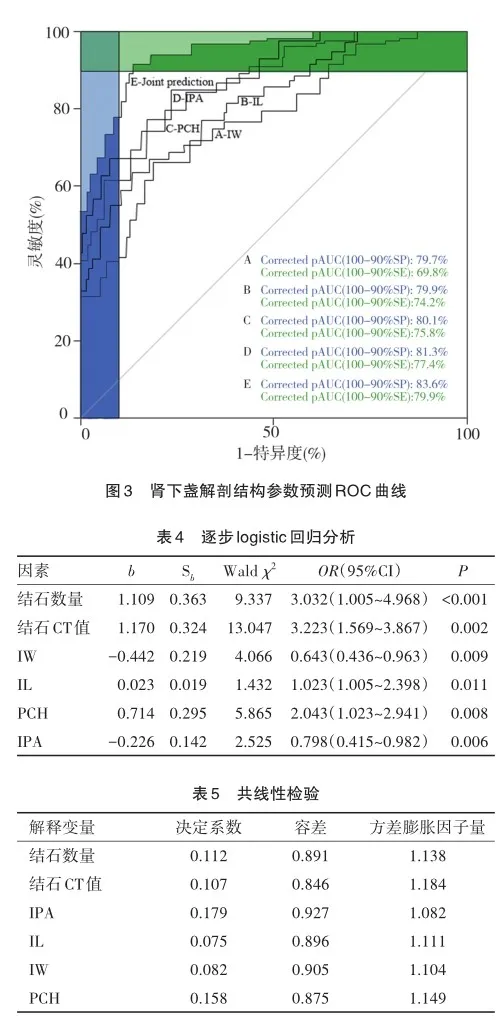
2.4 肾下盏解剖结构参数对术后结石残余的预测价值
采用ROC曲线分析肾下盏解剖结构参数对术后结石残余的预测价值,结果显示肾下盏解剖结构参数(IL、IW、PCH、IPA)及联合预测的曲线下面积(area under the curve,AUC)分别为0.798(95%CI=0.673~0.829)、0.774(95%CI=0.671~ 0.811)、0.739(95%CI=0.660~0.807)、0.787(95%CI=0.682~ 0.835)、0.876(95%CI=0.716~0.893),其联合预测价值AUC优于任何单一参数单独诊断(Z二者联合-IPA=2.093,P=0.038; Z二者联合-IL=2.649,P=0.019;Z二者联合-IW=2.931,P=0.006;Z二者联合-PCH= 2.513,P=0.023),分别见表3,图3。
2.5 逐步logistic回归分析
以P<0.05为变量筛选的标准,最终纳入肾功能不全史、结石数量、结石CT值、手术时间、UA、BUN、IPA、IL、IW、PCH共10个因素为自变量,以患者肾下盏是否结石残余为因变量赋值(0=否;1=是)后进行逐步logistic回归分析,最终筛选出最佳因子。本研究结果显示结石数量、结石CT值、IL、PCH是影响患者经改良无管化PCNL治疗肾下盏结石残余的独立危险因素,IW、IPA是保护因素(P均<0.05),见表4。
2.6 多重共线性检验
将表5中的危险因素进行共线性检验,其中方差膨胀因子越高则多重共线性的影响越严重,越接近于1则多重共线性影响越轻。该结果表明,各解释变量方差膨胀因子均<10,容差均>0.2,提示解释变量与其余解释之间不存在多重共线性,各解释变量之间相互独立,见表5。
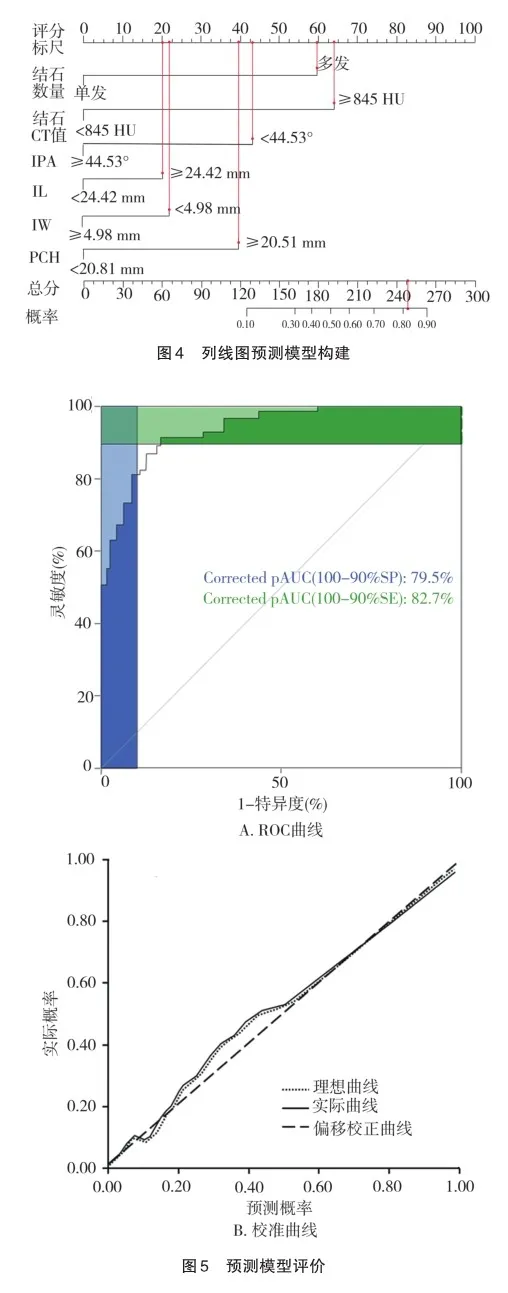
2.7 列线图预测模型构建
将表5中影响患者术后结石残余的因素构建预测模型,得到回归方程为Logit(P)=-2.567+0.110 9×X1+1.170×X2-0.226×X3+0.023×X4-0.442×X5+0.714×X6,P=elogit(P)/[1+ elogit(P)],其中X1为结石数量(多发=1;单发=0),X2为结石CT值(≥845 HU=1;<845 HU=0),X3为IPA(<44.53°=1;≥44.53°=0),X4为IL(≥24.42 mm=1;<24.42 mm=0),X5为IW(<4.98 mm=1;≥4.98 mm=0);X6为PCH(≥20.51 mm=1;<20.51 mm=0),绘制列线图。例如患者,女,年龄48岁,结石数量对应赋分为59.28分,结石CT值对应赋分为63.01分,IPA对应赋分为42.97分,IL对应赋分为20.00分,IW对应赋分为22.35分,PCH对应赋分为39.94分,6项独立影响因素总分为247.55,对应风险值为0.82,预测患者术后结石残余的概率为82%,见图4。
2.8 模型评价
根据预测概率P与患者术后结石残余的关系建立ROC曲线,结果显示模型C-index值为0.893(95%CI=0.878~ 0.901),模型AUC为0.888(95%CI=0.869~0.897),灵敏度为0.827,特异度为0.795,表明该预测模型的区分度较好,校准曲线表明理想曲线与实际曲线贴合程度较高,表明该预测模型在预测患者术后结石残余的风险值上表现出良好的一致性,见图5。

3 讨 论
肾结石是泌尿外科多发病,患者可出现肾区绞痛、尿路堵塞、肾积水等多种并发症,对患者的肾脏功能及生活质量造成严重影响[9-10]。而肾下盏处在肾盏的最低处,由于其空间位置相对较低,因而在重力作用的促进下更易造成肾结石的发生发展,同时部分患者肾下盏由于解剖结构特殊,再加上肾下盏形成的结石其质地相对较硬,因而加剧了临床治疗的难度,严重影响了患者的预后[11-12]。
近年来,PCNL术由于创伤小、并发症较少、住院时间相对较短、术后恢复较快等优势,成为目前治疗肾结石的首选方法之一,特别是在治疗复杂性肾结石方面,优势更加明显[13-14]。但传统PCNL术后往往为了填塞止血皮肾通道、促进肾脏的引流作用以及若发现残余结石需行PCNL时可免去再次穿刺,常留置输尿管支架管等,增加了患者术后疼痛感,进而推迟了出院时间,同时输尿管内支架也可进行引流作用,能够替代肾造瘘管[15-17]。因此,临床进行开展完全无管化PCNL研究,能够避免因置管造成的不适等[18-19]。而结石清除率在反映患者结石治疗效果方面具有显著的效果,本研究通过对300例肾下盏结石患者行改良无管化PCNL治疗,术后结石残留率为15.67%,整体治疗效果较好,并对2组单因素分析存在差异的因素进一步进行逐步logistic回归分析结果显示结石数量、结石CT值、IPA、IL、IW、PCH是影响患者经改良无管化PCNL治疗肾下盏结石残余的独立危险因素(P<0.05)。分析原因如下:多发结石往往手术时间比较长,集合系统解剖复杂、多通道取石、分期手术的概率相对增大,这使得患者术后出血风险增加,影响了PCNL的清石率[20];而结石CT值与结石硬度密切相关,CT值越高提示碎石效率降低,进而导致粉碎时间相对延长[21];IPA、IL、IW、PCH均是肾下盏解剖结构的表示,经皮肾镜可调整的角度有限,IPA越狭小,IW越窄,致使部分结石无法寻到或无法粉碎,促使结石残留可能性增加;而IL越长,PCH越高,其手术治疗难度增加,其手术时间也相应增加,增加了并发症的发生风险,也不利于残余结石的排出,同时PCH越高可能影响下盏感染性尿液引流,增大了感染风险[22-25]。另外,本研究基于影响肾下盏结石疗效的影响因素,构建了列线图预测模型,对结石数量、结石CT值、IPA、IL、IW、PCH量化评分并评估风险,得到回归方程为Logit(P)=-2.567+1.109*结石数量+1.170*结石CT值-0.226*IPA+0.023*IL-0.442*IW+ 0.714*PCH,并经Bootstrap自抽样进行验证,结果表明模型C-index为0.893(95%CI=0.878~0.901),AUC为0.888(95%CI=0.869~0.897),提示该预测模型区分度相对较高;校准曲线显示该模型预测的准确度相对较高。另外,本研究存在一定局限性,基于研究时间及现条件限制,其研究样本量较小,且对采用改良无管化PCNL的患者,本研究是经过一定适应证筛选的,因而在结果方面可能存在一定的偏倚,后续有待进一步进行大规模研究对本研究结论进行证实。
综上所述,经改良无管化PCNL治疗2~3 cm肾下盏结石,相对安全有效,临床上治疗2~3 cm肾下盏结石患者时可重点关注其肾下盏解剖结构参数,充分评估术后结石残留风险,及时调整治疗方案,进而提高患者的生活质量。.
参 考 文 献
[1] Ye Z,Wu C,Xiong Y,et al. Obesity,metabolic dysfunction,and risk of kidney stone disease: a national cross-sectional study[J]. Aging Male,2023,26(1):2195932.
[2] 姜华龙,李 萍,严跃龙,等. 半无管化单次微通道经皮肾镜与输尿管软镜治疗15~20 mm肾下盏结石的对比分析[J]. 临床泌尿外科杂志,2019,34(9):683-688. Jiang HL,Li P,Yan YL,et al. Comparison between half tubeless singlesession mini-invasive percutaneous nephrolithotomy and retrograde in? trarenal surgery for lower-pole renal calculus with diameter of 15-20 mm[J]. J Clin Urol,2019,34(9):683-688.
[3] 索 杰,段万里,邓 骞,等. 肾下盏解剖对软式输尿管镜治疗肾下盏结石术后清石率的影响及预测模型构建[J]. 现代泌尿外科杂志,2021,26(11):914-917. Suo J,Duan WL,Deng Q,et al. Effects of subcalyx anatomy on stone clearance of lower pole stones treated with flexible ureteroscopy and con? struction of prediction model[J]. J Mod Urol,2021,26(11):914-917.
[4] Jiang PB,Brevik A,Clayman RV. The life and death of percutane? ous stone removal:“looking back-looking forward”[J]. Urol Clin North Am,2022,49(1):119-128.
[5] Liu Y,Zhu W,Zeng GH. Percutaneous nephrolithotomy with suc? tion:is this the future?[J]. Curr Opin Urol,2021,31(2):95-101.
[6] van den Broeck T,Zhu XY,Kusters A,et al. Percutaneous nephro? lithotomy with intraoperative computed tomography scanning improves stone-free rates[J]. J Endourol,2021,35(3):267-273.
[7] Ito H,Kawahara T,Terao H,et al. The most reliable preoperative assessment of renal stone burden as a predictor of stone-free status after flexible ureteroscopy with holmium laser lithotripsy:a single-center ex? perience[J]. Urology,2012,80(3):524-528.
[8] Resorlu B,Oguz U,Resorlu EB,et al. The impact of pelvicaliceal anatomy on the success of retrograde intrarenal surgery in patients with lower pole renal stones[J]. Urology,2012,79(1):61-66.
[9] Dresner SL,Iremashvili V,Best SL,et al. Influence of lower pole infundibulopelvic angle on success of retrograde flexible ureteroscopy and laser lithotripsy for the treatment of renal stones[J]. J Endourol,2020,34(6):655-660.
[10] Richard F,Marguin J,Frontczak A,et al. Evaluation and compari? son of scoring systems for predicting stone-free status after flexible ureteroscopy for renal and ureteral stones[J]. PLoS One,2020,15(8):e0237068.
[11] 闻玉钢,李金永,邢维思,等. 肾脏解剖结构对经皮肾镜取石术后结石残留的影响[J]. 宁夏医学杂志,2021,43(11):961-964. Wen YG,Li JY,Xing WS,et al. The effects of renal anatomy on residual stones after percutaneous nephrolithotomy[J]. Ningxia Med J,2021,43(11):961-964.
[12] 曾 佩,刘 莹. 不同肾盂漏斗部夹角肾下盏结石病人采用不同术式的疗效及疗效相关因素分析[J]. 临床外科杂志,2022,30(1):78-81. Zeng P,Liu Y. Analysis of curative effect and curative effect-related factors of different surgical procedures for patients with inferior calyx calculi with different funnel angles of the renal pelvis[J]. J Clin Surg,2022,30(1):78-81.
[13] Zhu SS,Fan YP,Hu X,et al. Correlation analysis between renal anatomical factors and residual stones after an ultrasound-guided PCNL[J]. Front Surg,2023,10:1121424.
[14] 黄 静,程树林,程 艳,等. 完全无管化经皮肾镜取石术治疗直径1cm及以下肾结石[J]. 西部医学,2020,32(4):527-531. Huang J,Cheng SL,Cheng Y,et al. Efficacy of totally tubeless percuta? neous nephrolithotomy in the treatment of renal calculi with diameter≤1cm[J]. Med J West China,2020,32(4):527-531.
[15] Lin FY,Li BJ,Rao T,et al. Presence of a novel anatomical struc? ture may cause bleeding when using the Calyx access in minipercutaneous nephrolithotomy[J]. Front Surg,2022,9:942147.
[16] Lei J,Huang K,Dai YB,et al. Evaluating outcomes of patientcentered enhanced recovery after surgery(ERAS) in percutaneous neph? rolithotomy for staghorn stones:an initial experience[J]. Front Surg,2023,10:1138814.
[17] 王 磊. 采用经皮肾镜取石术与传统开放性手术对肾结石患者并发症发生率的对比研究[J]. 当代医学,2020,26(11):146-147. Wang L. Comparative study on the incidence of complications in pa? tients with kidney stones using percutaneous nephrolithotomy and tradi? tional open surgery[J]. Contemp Med,2020,26(11):146-147.
[18] 谢英金,向 菲,赵墨林,等. 改良无管化经皮肾镜碎石取石术对肾输尿管上段结石患者围术期指标、术后疼痛和并发症的影响[J]. 实用医院临床杂志,2021,18(6):115-118. Xie YJ,Xiang F,Zhao ML,et al. The effect of modified tubeless percuta? neous nephrolithotomy on perioperative indicators,postoperative pain and complications of patients with renal upper ureteral calculi[J]. Pract J Clin Med,2021,18(6):115-118.
[19] 祝广峰,汪 涌,窦小亮,等. 完全无管化微通道经皮肾镜对比输尿管(软)镜治疗输尿管上段嵌顿性结石50例疗效分析[J]. 现代泌尿外科杂志,2020,25(10):910-914. Zhu GF,Wang Y,Dou XL,et al. Surgical experience of totally tubeless mini-percutaneous nephrolithotomy vs. flexible ureteroscopic lithotripsy for upper ureteral incarcerated calculi[J]. J Mod Urol,2020,25(10):910-914.
[20] 周剑芳,高 诚,阳东荣. S. T. O. N. E. 评分与肾结石经皮肾镜术后清石率及并发症的相关性分析[J]. 中华腔镜泌尿外科杂志(电子版),2021,15(2):121-125. Zhou JF,Gao C,Yang DR. Correlation analysis between S. T. O. N. E. score and stone clearance rate or the complications in renal calculi pa? tients treated with percutaneous nephrolithotomy[J]. Chin J Endourol Electron Ed,2021,15(2):121-125.
[21] 杨 杰,王坤杰,王 佳. 经皮肾镜碎石取石术清石率影响因素分析[J]. 四川大学学报(医学版),2019,50(3):445-447. Yang J,Wang KJ,Wang J. Analysis of influencing factors on stone re? moval rate of percutaneous nephrolithotomy[J]. J Sichuan Univ Med Sci Ed,2019,50(3):445-447.
[22] Inoue T,Hamamoto S,Okada S,et al. Single-session impact of high-power laser with Moses technology for lower pole stones in retro? grade intrarenal surgery:retrospective study[J]. J Clin Med,2022,12(1):301.
[23] 朱学华,杨明钰,夏海缀,等. 机器学习模型在预测肾结石输尿管软镜碎石术后早期结石清除率中的应用[J]. 北京大学学报(医学版),2019,51(4):653-659. Zhu XH,Yang MY,Xia HZ,et al. Application of machine learning mod? els in predicting early stone-free rate after flexible ureteroscopic litho? tripsy for renal stones[J]. J Peking Univ Health Sci,2019,51(4):653-659.
[24] 谭 军,杨国胜. 肾下盏解剖结构在输尿管软镜治疗肾下盏结石中的研究进展[J]. 现代泌尿外科杂志,2019,24(4):320-324. Tan J,Yang GS. Research progress of anatomical structure of inferior re? nal calyx in the treatment of calculus of inferior renal calyx by ureteros? copy[J]. J Mod Urol,2019,24(4):320-324.
[25] Karim SS,Hanna,Geraghty R,et al. Role of pelvicalyceal anatomy in the outcomes of retrograde intrarenal surgery(RIRS) for lower pole stones:outcomes with a systematic review of literature[J]. Uro? lithiasis,2020,48(3):263-270.
(责任编辑:李青颖)
本文引用格式:
吴 韬,王 亮. 改良无管化经皮肾镜碎石取石术治疗2~3 cm肾下盏结石后肾下盏解剖结构的变化及对术后清石率的影响[J]. 重庆医科大学学报,2025,50(2):183-190.