单髁置换术与全膝关节置换术治疗膝骨关节炎的早期疗效评价
吴常杰,闫帮楷,李英祥,赵新动,夏欢,冯小兵
摘要:目的 评价单髁置换术(UKA)与全膝关节置换术(TKA)治疗膝骨关节炎的早期疗效差异。方法 纳入2020年6月-2022年2月于新疆生产建设兵团第六师奇台医院就诊的符合手术治疗的膝骨关节炎患者77例,按照治疗方式不同分为UKA组(n=35)和TKA组(n=42)。UKA组予以UKA,TKA组予以TKA,比较兩组临床指标(手术时间、术中出血、术后引流量、住院时间)、膝关节疼痛及活动度[疼痛视觉模拟评分(VAS)、膝关节活动度(ROM)]、预后(WOMAC评分)、经济负担。结果 UKA组手术时间、住院时间短于TKA组,术中出血、术后引流量少于TKA组,但差异无统计学意义(P>0.05);两组术后VAS评分低于术前,ROM高于术前,且UKA组VAS评分、ROM低于TKA组,差异有统计学意义(P<0.05);两组术后1周及1、3、6、12个月WOMAC评分低于术前,且UKA组术后3个月WOMAC评分低于TKA组,差异有统计学意义(P<0.05);UKA组术后总费用评分低于TKA组,其中材料费UKA组低于TKA组,差异有统计学意义(P<0.05)。结论 UKA术式在早期缓解膝骨关节炎患者疼痛、降低WOMAC评分、减轻经济负担方面具有更好的优势,而TKA术式能更好地恢复患者膝关节活动度,因此临床上应综合评价患者预后的差异及经济条件后再选择适宜的手术方式。
关键词:膝骨性关节炎;单髁置换术;全膝关节置换术;膝关节活动度
中图分类号:R687.4 文献标识码:A DOI:10.3969/j.issn.1006-1959.2024.08.021
文章编号:1006-1959(2024)08-0109-05
Early Efficacy Evaluation of Unicompartmental Knee Arthroplasty and Total Knee Arthroplasty
in the Treatment of Knee Osteoarthritis
WU Chang-jie1,YAN Bang-kai1,LI Ying-xiang1,ZHAO Xin-dong1,XIA Huan2,FENG Xiao-bing1
(1.Department of Orthopaedics,Qitai Hospital of the Sixth Division of Xinjiang Production and Construction Corps,
Changji 831800,Xinjiang,China;
2.Department of Nuclear Medicine,Cancer Hospital Affiliated to Xinjiang Medical University,Urumqi 830011,Xinjiang,China)
Abstract:Objective To evaluate the early efficacy of unicompartmental knee arthroplasty (UKA) and total knee arthroplasty (TKA) in the treatment of knee osteoarthritis.Methods From June 2020 to February 2022, 77 patients with knee osteoarthritis who met the surgical treatment in Qitai Hospital of the Sixth Division of Xinjiang Production and Construction Corps were included. According to different treatment methods, they were divided into UKA group (n=35) and TKA group (n=42). UKA group was treated with UKA, and TKA group was treated with TKA. The clinical indexes (operation time, intraoperative bleeding, postoperative drainage volume, hospitalization time), knee joint pain and activity [Visual Analogue Scale (VAS), range of motion (ROM)], prognosis (WOMAC score) and economic burden were compared between the two groups.Results The operation time and hospitalization time of UKA group were shorter than those of TKA group, and the intraoperative bleeding and postoperative drainage volume were less than those of TKA group, but the differences were not statistically significant (P>0.05). The VAS score of the two groups after operation was lower than that before operation, and the ROM was higher than that before operation, while the VAS score and ROM of the UKA group were lower than those of the TKA group, and the differences were statistically significant (P<0.05). The WOMAC score of the two groups at 1 week, 1 month, 3 months, 6 months and 12 months after operation was lower than that before operation, and the WOMAC score of the UKA group at 3 months after operation was lower than that of the TKA group, the differences was statistically significant (P<0.05). The total cost score of the UKA group was lower than that of the TKA group, and the material cost of the UKA group was lower than that of the TKA group, the difference was statistically significant (P<0.05).Conclusion UKA has better advantages in relieving pain, reducing WOMAC score and reducing economic burden in patients with knee osteoarthritis in the early stage, while TKA can better restore the knee joint activity of patients. Therefore, the difference of prognosis and economic conditions of patients should be comprehensively evaluated before selecting the appropriate surgical method.
Key words:Knee osteoarthritis;Unicompartmental knee arthroplasty;Total knee arthroplasty;Range of motion
膝骨性关节炎(knee osteoarthritis, KOA)是一種常见的退化性关节疾病[1]。全膝关节置换术(total knee arthroplasty, TKA)是目前全球公认的治疗KOA方法,该术式主要通过侧向机械轴重定位来矫正内翻畸形。TKA不仅可有效修复关节,而且患者身体重力负荷几乎不受影响[2]。而随着医疗科技的进步,单髁置换术(unicompartmental knee arthroplasty, UKA)逐渐受到临床关注,其主要通过植入假体来治疗受影响的膝关节内变性隔室,同时保留不受影响的隔室。UKA术式对膝骨切除范围小,并为患者提供了一种创伤较小、恢复时间更快的方法[3]。由于目前对两种术式优缺点仍有一定争议,因此本研究旨在分析UKA与TKA治疗膝骨关节炎的早期疗效差异,以期为指导临床治疗提供相关理论依据。
1资料与方法
1.1一般资料 纳入2020年6月-2022年2月新疆生产建设兵团第六师奇台医院需要行膝关节手术治疗的患者77例。纳入标准:符合膝骨关节炎手术适应证[4],局部疼痛明显,需关节置换,且膝关节屈曲挛缩畸形<15°,外翻及内翻畸形<15°;术中探查所见膝关节外侧室及前后交叉韧带形态及功能未见明显受损;患者依从性较好,能够配合后续随访满1年者。排除标准:双侧前后交叉韧带不完整;心肺功能不全不能耐受手术者。按照随机数字发分为UKA组和TKA组。UKA组35例,其中男21例,女14例;年龄52~81岁,平均年龄(67.13±11.42)岁;BMI 7.59~28.12 kg/m2,平均BMI(23.83±4.29)kg/m2。TKA组42例,其中男26例,女16例;年龄53~78岁,平均年龄(65.74±10.83)岁;平均BMI 18.14~29.49 kg/m2,平均BMI(25.12±5.36)kg/m2。两组性别、年龄、BMI比较,差异无统计学意义(P>0.05),可对比。本研究通过我院伦理审核,且所有患者知情同意并签署知情同意书。
1.2方法 两组均采用仰卧位,硬膜外麻醉后,充分暴露术区膝关节。UKA组常规消毒铺单后在髌骨内侧上缘至髌韧带内侧下发做弧形切口,切口充分暴露胫骨结节、胫骨平台内侧缘,清除部分内侧半月板、局部骨赘,避免损伤邻近相关韧带,使用股骨间隙测量器及胫骨锯导引器确定胫骨平台内侧截骨平面,标记后使用摆锯锯片进行胫骨平台内侧截骨,打磨后试模,置入大小相匹配的假体。TKA组取患膝正中切口,切除全半月板、骨赘及前后交叉韧带,定位后行胫骨及股骨平台截骨,安装股骨及胫骨假体。两种术式假体安装后使用生理盐水反复冲洗关节腔,安放引流管后加压包扎。
1.3观察指标 比较两组临床指标(手术时间、术中出血、术后引流量、住院时间)、膝关节疼痛[于术后12个月,采用疼痛视觉模拟评分(visual analogue score, VAS)评估膝关节疼痛,总分0~10分,其中0分为无痛;3分以下为轻微疼痛且患者自诉能忍受;4~6分为患者疼痛且影响睡眠,尚能忍受;7~10分为强烈疼痛,患者难以忍受]、膝关节活动度(range of motion,ROM)(于术前及术后12个月进行评估,测量关节活动时可达到的最大弧度)、预后(于术前、术后1周、术后1、3、6、12个月,采用WOMAC评分[5]进行评估,其中评分>48分为重度;21~48分为中度;<21分为轻度)、经济负担[手术费、检查费、材料费、交通与住宿费及药费(外用药及口服药等),其中材料费包含部分患者二次住院时翻修的费用合计]。
1.4统计学方法 采用SPSS 21.0统计学软件进行数据分析。计量资料以(x±s)表示,采用t检验;计数资料以[n(%)]表示,采用?字2检验。以P<0.05表示差异有统计学意义。
2结果
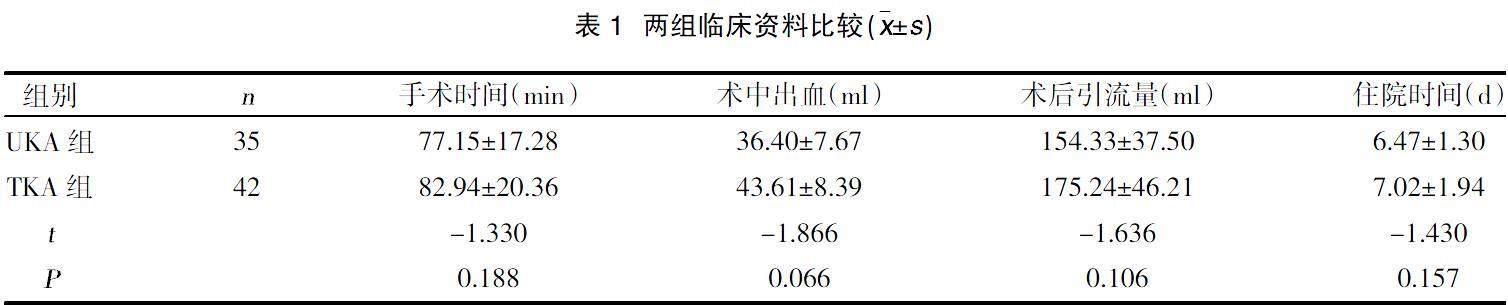
2.1两组临床指标比较 UKA组手术时间、住院时间短于TKA组,术中出血、术后引流量少于TKA组,但差异无统计学意义(P>0.05),见表1。
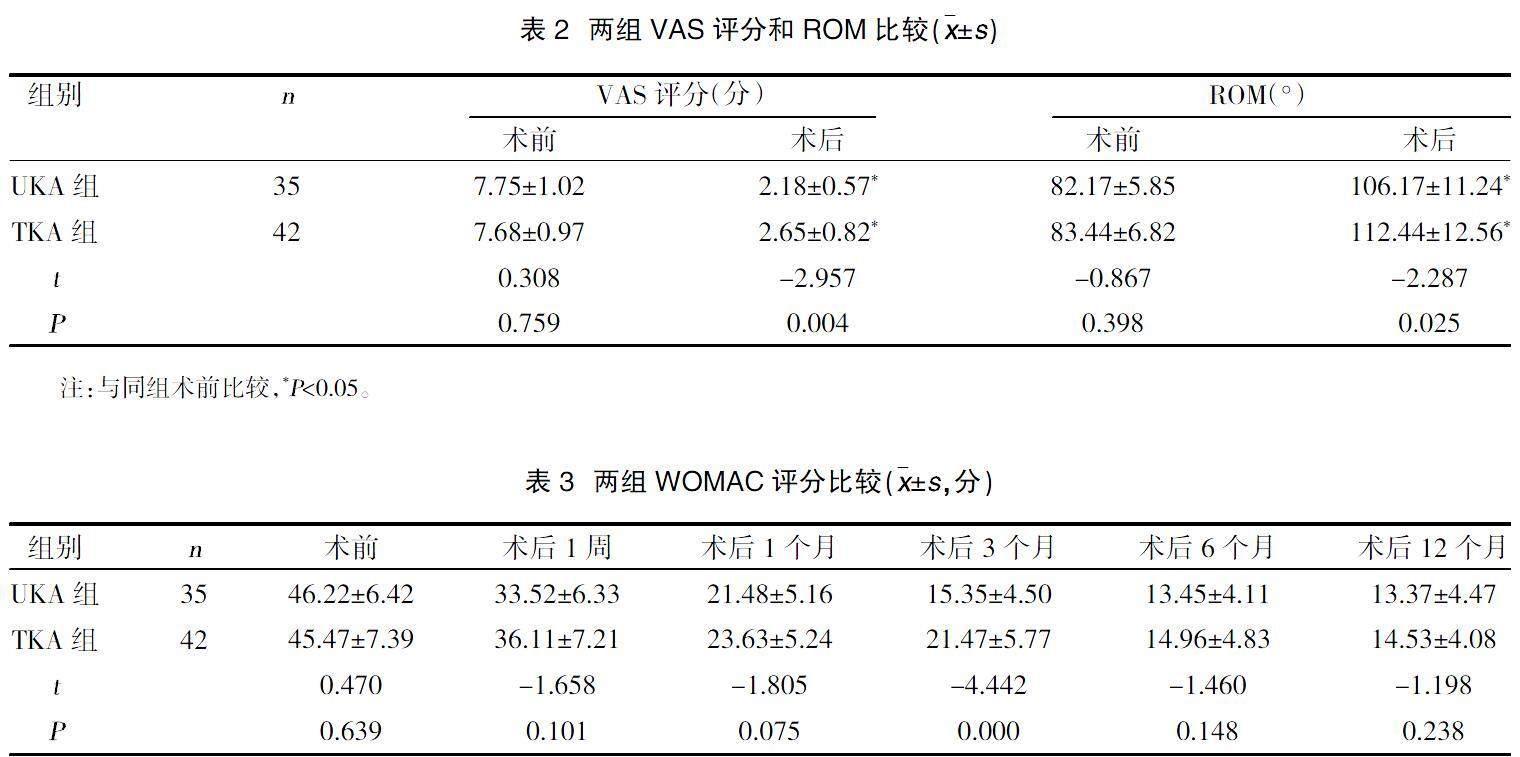
2.2两组VAS评分和ROM比较 两组术后VAS评分低于术前,ROM高于术前,且UKA组VAS评分、ROM低于TKA组,差异有统计学意义(P<0.05),见表2。
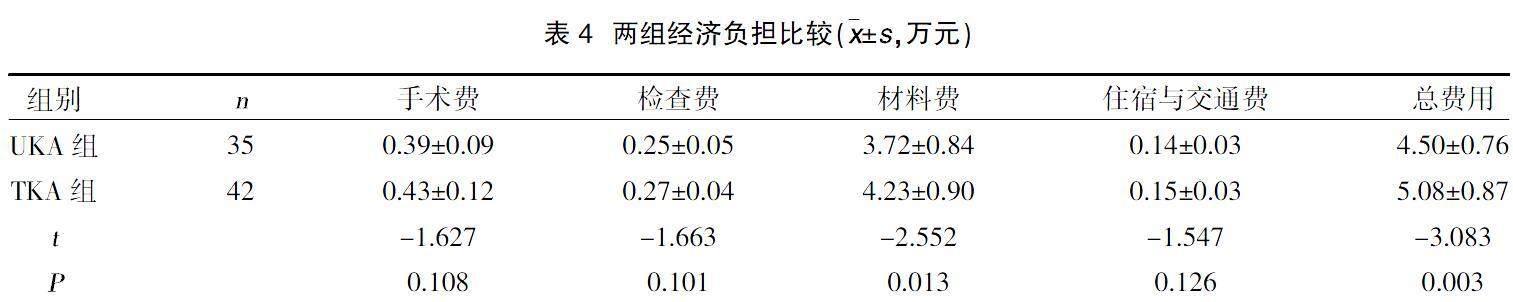
2.3两组WOMAC评分比较 两组术后1周及1、3、6、12个月WOMAC评分低于术前,且UKA组术后3个月WOMAC评分低于TKA组,差异有统计学意义(P<0.05),见表3。
2.4两组经济负担比较 UKA组术后总费用评分低于TKA组,其中材料费UKA组低于TKA组,差异有统计学意义(P<0.05),见表4。
3讨论
KOA的发病机制较为复杂,首先表现为膝关节内分子的代谢异常,然后是解剖和生理紊乱,特征是软骨退化、骨重塑、骨赘形成、关节炎症和正常关节功能丧失,最终导致疾病发生[6-8]。KOA的典型影像学特征为关节软骨和半月板的磨损引起的关节间隙变窄,以及软骨硬化和骨赘形成[9,10]。虽然UKA和TKA均作为治疗膝骨关节炎的有效方法,但两者在手术方式上存在一定差异,如TKA术需要全膝关节的修复,创面较大,过程也相对较为复杂,而UKA仅需要进行局部的关节置换。然而,本研究结果显示,UKA组手术时间、住院时间短于TKA组,术中出血、术后引流量少于TKA组,但差异无统计学意义(P>0.05),这提示对于符合手术要求的患者,UKA及TKA两种手术方式均可以在临床广泛应用[11]。
部分KOA患者病程早期即可出现疼痛,且随着时间推移,疼痛严重程度则越严重[12]。既往研究表明[13],大多数患者在长达6年甚至更长时间的随访观察中发现疼痛症状几乎没有明显改善。本研究结果显示,无论UKA组还是TKA组患者,术后VAS评分均较术前明显降低,这与既往大部分研究结果相仿[14-16]。而进一步比较发现,UKA组术后VAS评分低于TKA组,提示UKA术式在改善患者疼痛方面优于TKA。在治疗膝关节活动度方面,UKA和TKA均能明显改善ROM的度数,但TKA组术后ROM高于UKA组,说明TKA较UKA术式能更好地改善患者术后膝关节的活动范围。
TKA的目的是將机械轴从病理区域转移到正常区室,这可能伴随疼痛缓解和功能改善,从而延迟KOA的进展[17]。但TKA组创面较大,且退化的隔室依然存在,手术后腿部对齐方式存在较大变化,这对于TKA患者可能需要更长的时间来适应。相比之下,UKA是一种膝关节的局部手术,术中植入的假体对膝关节的影响较小,并保留未受影响的小室[18],因此UKA术后的患者恢复更快。Jeon YS等[19]研究发现,接受UKA的患者在6个月时的术后活动水平较TKA患者要快,而两组在12个月和2年的随访中无显著差异。本研究也得出类似的结果,UKA组和TKA组虽然在术后1年的随访中WOMAC评分均能得到改善,但UKA组需要约3个月达到轻度水平,而TKA组患者恢复至相似水平要耗时6个月。Tu Y等[20]研究显示,与TKA相比,UKA组患者早期预后的综合评价优势更突出。而Stukenborg-Colsman C等[21]则进行了更长时间的随访,结果表明两种术式均具有整体优势。基于上述原因,UKA可能较TKA在术后早期提供更好的功能预后,而长期疗效可能无明显差异,故临床上有必要对两组患者的预后进行更长时间的随访。
虽然上述两组术式均能得到令人满意的功能疗效,但由于植入假体材料的特殊性,仍然给患者及其家属带来了较大的经济负担。本研究结果显示,UKA组术后总费用低于TKA组,其中材料费UKA组低于TKA组(P<0.05),与既往研究结果类似[22]。研究显示[23],与TKA相比,UKA的手术部位感染比例较低。TKA组由于手术创面较大,发生绯总神经损伤,腔内感染等并发症的风险更高,继而发生翻修的患者人数增加[24]。Smith WB 2nd等[25]采用统计模型来模拟40、50、60和70岁年龄段接受UKA和TKA手术患者预后的队列研究发现,对于年龄超过50岁的患者,TKA组早期膝关节翻修率明显高于UKA组。因此,TKA组承受更高的经济负担可能与并发症及翻修比例更高有关。
综上所述,UKA和TKA术后早期均能有效改善患者的膝关节的功能,UKA术式在缓解KOA患者疼痛,降低WOMAC评分、减轻经济负担方面具有更好的优势,而TKA术式能更好地恢复患者膝关节活动度,因此临床上应综合评价患者早期预后的差异及经济条件后再选择适宜的手术方式。
参考文献:
[1]Driban JB,Harkey MS,Barbe MF,et al.Risk factors and the natural history of accelerated knee osteoarthritis: a narrative review[J].BMC Musculoskelet Disord,2020,21(1):332.
[2]Hsu KY,Tsai YF,Yeh WL,et al.Triggers and decision-making patterns for receiving total knee arthroplasty among older adults with knee osteoarthritis:A qualitative descriptive study[J].J Clin Nurs,2018,27(23-24):4373-4380.
[3]Briggs KK,Kocher MS,Rodkey WG,et al.Reliability,Validity,and Responsiveness of the Lysholm Knee Score and Tegner Activity Scale for Patients with Meniscal Injury of the Knee[J].J Bone Joint Surg Am,2006,88(4):698-705.
[4]中国医院协会临床新技术应用专业委员会,中华医学会骨科学分会关节外科学组,中国医师协会骨科医师分会骨关节炎学组.中国膝关节周围截骨下肢力线矫正术治疗膝关节骨关节炎临床指南[J].中华骨科杂志,2021,41(23):1655-1672.
[5]Copsey B,Thompson JY,Vadher K,et al.Problems persist in reporting of methods and results for the WOMAC measure in hip and knee osteoarthritis trials[J].Qual Life Res,2018,28(2):335-343.
[6]Driban JB,Price LL,Lu B,et al.The natural history of end-stage knee osteoarthritis:Data from the osteoarthritis initiative[J].Semin Arthritis Rheu,2022,58:152148.
[7]Daszkiewicz K,?覵uczkiewicz P.Biomechanics of the medial meniscus in the osteoarthritic knee joint[J].Peer J,2021,9:e12509.
[8]Xing R,Wang P,Zhao L,et al.Mechanism of TRPA1 and TRPV4 Participating in Mechanical Hyperalgesia of Rat Experimental Knee Osteoarthritis[J].Arch Rheumatol,2017,32(2):96-104.
[9]Mittal S,Pradhan G,Singh S,et al.T1 and T2 mapping of articular cartilage and menisci in early osteoarthritis of the knee using 3-Tesla magnetic resonance imaging[J].Pol J Radiol,2019,84:e549-e564.
[10]Sukerkar PA,Doyle Z.Imaging of Osteoarthritis of the Knee[J].Radiol Clin N Am,2022,60(4):605-616.
[11]Sun X,Su Z.A meta-analysis of unicompartmental knee arthroplasty revised to total knee arthroplasty versus primary total knee arthroplasty[J].J Orthop Surg Res,2018,13(1):158.
[12]Khachian A,Seyedoshohadaei M,Haghani H,et al.Effect of self-management program on outcome of adult knee osteoarthritis[J].Int J Orthop Trauma,2020,39:100797.
[13]Güng?觟r Demir U,Demir AN,Toraman NF.Neuropathic pain in knee osteoarthritis[J].Adv Rheumatol,2021,61(1):67.
[14]Blevins JL,Carroll KM,Burger JA,et al.Postoperative outcomes of total knee arthroplasty compared to unicompartmental knee arthroplasty:A matched comparison[J].Knee,2020,27(2):565-571.
[15]Knifsund J,Niinimaki T,Nurmi H,et al.Functional results of total-knee arthroplasty versus medial unicompartmental arthroplasty:two-year results of a randomised,assessor-blinded multicentre trial[J].BMJ Open,2021,11(6):e046731.
[16]Tille E,Beyer F,Auerbach K,et al.Better short-term function after unicompartmental compared to total knee arthroplasty[J].BMC Musculoskelet Disord,2021,22(1):326.
[17]Tan MWP,Ng SWL,Chen JY,et al.Long-Term Functional Outcomes and Quality of Life at Minimum 10-Year Follow-Up After Fixed-Bearing Unicompartmental Knee Arthroplasty and Total Knee Arthroplasty for Isolated Medial Compartment Osteoarthritis[J].J Arthroplasty,2020,36(4):1269-1276.
[18]Kievit AJ,Kuijer PPFM,de Haan LJ,et al.Patients return to work sooner after unicompartmental knee arthroplasty than after total knee arthroplasty[J].Knee Surg Sport Tr A,2019,28(9):2905-2916.
[19]Jeon YS,Ahn CH,Kim MK.Comparison of HTO with articular cartilage surgery and UKA in unicompartmental OA[J].J Orthop Surg (Hong Kong),2017,25(1):2309499016684092.
[20]Tu Y,Ma T,Wen T,et al.Does Unicompartmental Knee Replacement Offer Improved Clinical Advantages Over Total Knee Replacement in the Treatment of Isolated Lateral Osteoarthritis? A Matched Cohort Analysis From an Independent Center[J].J Arthroplasty,2020,35(8):2016-2021.
[21]Stukenborg-Colsman C,Wirth CJ,Lazovic D,et al.High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis:7-10-year follow-up prospective randomised study[J].Knee,2001,8(3):187-194.
[22]Chisari E,Yu AS,Yayac M,et al.Despite Equivalent Medicare Reimbursement,Facility Costs for Outpatient Total Knee Arthroplasty Are Higher Than Unicompartmental Knee Arthroplasty[J].J Arthroplasty,2020,36(7S):S141-S144.
[23]Yamagami R,Inui H,Jo T,et al.Unicompartmental knee arthroplasty is associated with lower proportions of surgical site infection compared with total knee arthroplasty:A retrospective nationwide database study[J].Knee,2020,28:124-130.
[24]Lombardi AV,Kolich MT,Berend KR,et al.Revision of Unicompartmental Knee Arthroplasty to Total Knee Arthroplasty:Is It as Good as a Primary Result[J]. J Arthroplasty,2018,33(7S):S105-S108.
[25]Smith WB 2nd,Steinberg J,Scholtes S,et al.Medial compartment knee osteoarthritis:age-stratified cost-effectiveness of total knee arthroplasty,unicompartmental knee arthroplasty,and high tibial osteotomy[J].Knee Surg Sports Traumatol Arthrosc,2017,25(3):924-933.
收稿日期:2023-04-13;修回日期:2023-05-10
編辑/杜帆

