Rosmarinic acid improves tracheal smooth muscle responsiveness and lung pathological changes in ovalbumin-sensitized rats
Vahideh Abbasnia ,Mohsen Foadoddini ,Delaram Eslimi Esfahani ,Mohammad Reza Khazdair ,Shahrbanoo Oryan
1Department of Biology,Payame Noor University,Tehran,Iran
2Cardiovascular Diseases Research Center,Birjand University of Medical Sciences,Birjand,Iran
3Department of Animal Sciences,Faculty of Biological Sciences,Kharazmi University,Tehran,Iran
ABSTRACT Objective: To evaluate the effect of rosmarinic acid on tracheal smooth muscle responsiveness and lung pathological changes in ovalbumin-sensitized rats.Methods: Rats were randomly divided into six groups: the control group,the asthmatic group,and the asthmatic groups treated with dexamethasone (1 mg/kg;oral gavage) or three doses of rosmarinic acid (0.5,1,and 2 mg/kg;oral gavage).For induction of asthma,rats received intraperitoneal injections and inhalation of ovalbumin.After 21 days,bronchoalveolar lavage fluid and lung samples were collected for histopathological analyses.Moreover,total and differential white blood cell counts were determined.Results: The rosmarinic acid-treated group had significantly lower tracheal smooth muscle responses to methacholine than the asthmatic group.In addition,rosmarinic acid reduced white blood cell count and the percentages of eosinophils,monocytes,and neutrophils while increasing the percentage of lymphocytes.Ovalbumin-induced lung pathological changes were significantly improved by treatment with rosmarinic acid.Conclusions: Rosmarinic acid improves tracheal smooth muscle responsiveness and lung pathological changes in ovalbuminsensitized rats.
KEYWORDS: Rosmarinic acid;Asthma;Ovalbumin;Tracheal responsiveness;Inflammation;White blood cell
Significance
Rosmarinic acid is a hydroxylated compound found in various plants and has various biological activities.The current study shows that rosmarinic acid alleviated bronchial asthma by improving tracheal smooth muscle responsiveness and lung injury.Therefore,rosmarinic acid may be further investigated as a natural component for treating allergic asthma.
1.Introduction
Asthma is a persistent inflammatory condition affecting the respiratory system,wherein numerous cells and cellular components contribute to its progression[1].Chronic inflammation is accompanied by increased airway responsiveness,usually reversible by itself or treatment.There are primarily two classifications of factors involved in the development and occurrence of asthma,which include factors related to the host (genetic factors,obesity,and gender) and environmental factors (allergens,infectious agents,smoking,occupational sensitivities,and air pollution)[2].Mast cells,eosinophils,T lymphocytes,dendritic cells,macrophages,and neutrophils are all inflammatory cells that contribute to the development of asthma[3].These cells release mediators such as chemokines,leukotrienes,cytokines,histamine,and prostaglandins,leading to asthma symptoms.Asthma is a disease characterized by an abnormal increase in the response of the airways to a broad group of physical,chemical,pharmacological,and immunological inhalation stimuli[4,5].Increased airway responsiveness refers to a situation where a weak stimulus that does not cause a response in healthy people causes an increase in the airway response in asthmatic people.This response may include coughing,increased mucus secretion,or shortness of breath,but the primary response in asthma is acute airway narrowing[6,7].Asthma treatments depend mainly on symptom relief,which can cause adverse effects.Hence,current research must concentrate on natural remedies for anti-asthma that have minimal adverse reactions[8].Rosmarinic acid (RA) is a manmade compound that is widely present in various plants belonging to the Lamiaceae family.This compound is caffeic acid and 3,4-dihydroxyphenylacetic acid[9].RA has a wide range of medicinal effects,including anti-apoptotic and anti-tumor effects,and has positively improved nervous system diseases such as Parkinson’s disease,Alzheimer’s disease,and cerebral ischemia.This phenolic compound is also highly effective in reducing inflammation and oxidative stress,making it a powerful antioxidant[10].The antiinflammatory effects of RA have been demonstrated through in vitro and in vivo studies in various inflammatory diseases such as arthritis,colitis,and atopic dermatitis[9].In the current investigation,we evaluate the protective effect of RA on pathological changes in the lung,airway response and lung fluid inflammatory cells of a mouse model with ovalbumin (OVA)-induced bronchial asthma.
2.Materials and methods
2.1.Materials
RA and methacholine hydrochloride (Met) were acquired from Sigma Chemical Ltd,U.K.Formalin (37%) was procured from Merck KGaA,Darmstadt,Germany.
2.2.Induced sensitization in animals
A previously described method was used to sensitize animals to OVA[11].We sensitized rats to OVA (98% pure,Sigma,St.Louis,MO,USA) by intraperitoneal injection on days 1,2,and 3 with 0.9%sterile saline containing 100 mg Al(OH)3as an adjuvant.A 403B Air-compressing nebulizer was utilized for 20 min each day over the course of 6,9,12,15 and 21 days.Following this,the nebulizer was employed to administer an aerosol of OVA (2%) for a total of 21 days.Animals were exposed to aerosols while breathing,generally in a closed chamber with dimensions 30 cm × 20 cm × 20 cm.In the control group,saline was substituted for the OVA solution rather than the central solution.
2.3.Animal groups
A total of 48 male Wistar rats,weighing approximately (200 ±20) g,were accommodated in the School of Medicine at Birjand University of Medical Sciences,located in Birjand,Iran.These rats were kept under standard conditions maintained at a temperature of(22 ± 2) ℃,and a 12-hour light-dark cycle.During the experiment,rats were allowed free access to food and water.We randomly divided the animals into six groups (n=8) as follows: Ⅰ.Control group: Saline was administered intraperitoneally (i.p.) and inhaled(exposed);Ⅱ.Sensitized group (asthma): OVA was administered i.p.and inhaled;Ⅲ.dexamethasone-treated group: Sensitized rats treated with dexamethasone (1 mg/kg;oral gavage);Ⅳ-Ⅵ.RAtreated group with different doses: Sensitized rats were administered 0.5,1,and 2 mg/kg RA by oral gavage[12,13].
2.4.Procedures for preparing tissues
Following the last challenge,the trachea of rats was dissected 24 h after they were anesthetized with ketamine hydrochloride (50 mg/kg,i.p.).Almost four cartilages were acquired from the trachea ring.It was suspended in a Krebs-Henseleit perfusate solution including;sodium chloride (112 mM/L),potassium chloride (4.72 mM/L),magnesium sulfate (0.5 mM/L),calcium chloride (2.5 mM/L),sodium bicarbonate (25 mM/L),and dextrose (11 mM/L) in a 10 mL organ bath.During the Krebs reaction,a gas mixture of 95% O2and 5%CO2was used[14].After being suspended in 1 g of isotonic tension,tissues were washed every 15 min with a Krebs-Henseleit solution to equilibrate for at least 1 h.A power lab system measured contraction responses (Power Lab 8/30,ML870,AD Instruments,Australia).
2.5.Measurement of the response of the trachea to methacholine
The induction of tracheal smooth muscle contractions by methacholine hydrochloride was examined using cumulative log concentration-response curves.During each 2 min,consecutive concentrations were applied,and the contractions induced by each concentration were recorded at the end of the 2 min[15].The response curves of methacholine hydrochloride were utilized to measure the concentrations of methacholine hydrochloride that resulted in 50%of the maximum responses (EC50).
2.6.Measurement of inflammation in the bronchoalveolar lavage fluid (BALF)
A saline wash of 1 mL was administered five times to the left lungs of anesthetized animals after their lungs were dissected.A hemocytometer (Nanomohit Parse) (in a Burker chamber) was used to count in the BALF stained with Turk solution (Merck,Germany109277).A Neubauer Lam light microscope was used to count the total number of white blood cells (WBCs).A centrifuge(Pol ideal Pars) was then used to remove the supernatant from the remaining BALF by spinning the mixture at 2 000 g for 10 min at 4 ℃.Wright-Giemsa stain was applied to the smear prepared from the cells.Under a light microscope (Olympus CX-23 Japan),400 cells were counted for differential cell analysis using staining and morphological criteria,and the percentage was calculated.
2.7.Evaluation of pathological changes
A buffered formalin 10% solution was used to fix the right lung with the remaining trachea.Drying was achieved by passing the tissue through ethanol 70% to 100%,and clearing was accomplished using xylol.Hematoxylin-eosin (H&E) was used to stain the paraffin blocks of tissues.A light microscope (Olympus CX-23 Japan) was then used to examine the tissues.Lung pathological changes were scored as 0 (the absence of changes),1 (mild changes),2 (local changes),and 3 (severe changes)[16].
2.8.Statistical analysis
The total and differential WBC counts were represented as mean ± standard error of the mean (SEM).One-way analysis of variance (ANOVA) with Tukey-Kramer post-test was used for comparisons between three treatment groups (RA,OVA-sensitized,and dexamethasone-treated) and control animals.The median (Q1,Q3) values of the pathological lung change score was also used.Comparison of the data between groups was done using independentsample Kruskal-Wallis test with post hoc multiple comparisons.An analysis of significance was performed at the level of P<0.05.
2.9.Ethical statement
Ethics approval was obtained from the IR.BUMS.REC.1400.272 committee.
3.Results
3.1.Tracheal responsiveness to methacholine
The concentration-response curves of all sensitized groups exhibited a leftward shift in comparison to the curves of the control group.In contrast to the sensitized group,the curves of the dexamethasonetreated groups and three RA-treated groups shifted to the right (Figure 1).Administration of dexamethasone and a higher dose of RA (2 mg/kg) showed significantly higher EC50than that of the asthmatic group(P<0.01).
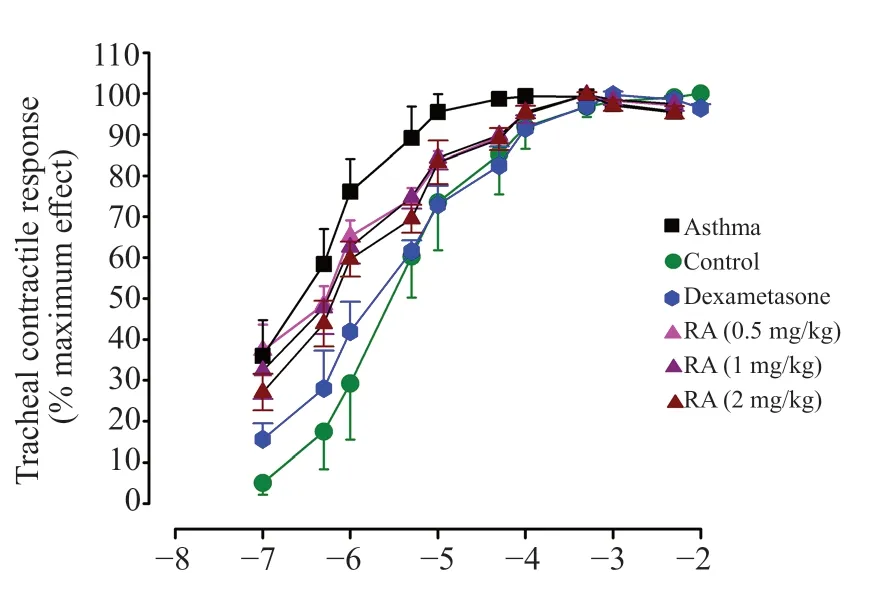
Figure 1.Cumulative log concentration-response curves of methacholineinduced contraction of smooth muscle in isolated trachea in sensitized rats treated with different doses of rosmarinic acid.RA: rosmarinic acid.
3.2.Total WBCs in BALF
A notable increase in the average count of WBC was observed in BALF of the asthmatic group (P<0.01).RA at different doses significantly lowered OVA-induced increase in WBC (P<0.01)(Table 1).
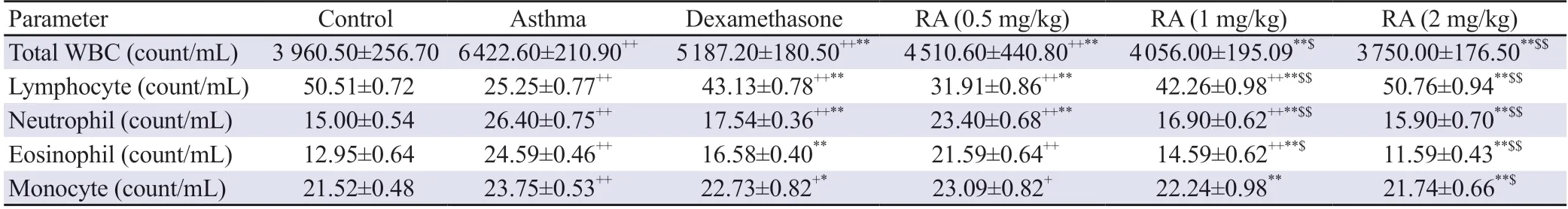
Table 1.Total and differential WBC count in bronchoalveolar lavage fluid of mice.
3.3.Differential WBCs in BALF
In the asthma group,the percentage of neutrophils,eosinophils,and monocytes was markedly higher compared to the control group,while that of lymphocytes was reduced (P<0.01).Treatment with RA significantly lowered OVA-induced increased neutrophils,eosinophils,and monocytes while increasing lymphocytes (P<0.05)(Table 1).
3.4.Histological results
Inflammation and hypertrophy of the lungs were found in OVAsensitized groups.According to the scoring of pathological changes,all OVA-induced groups had more significant pathological changes than the control group (Figure 2).Dexamethasone and RA improved these changes,especially when given at higher dosages.
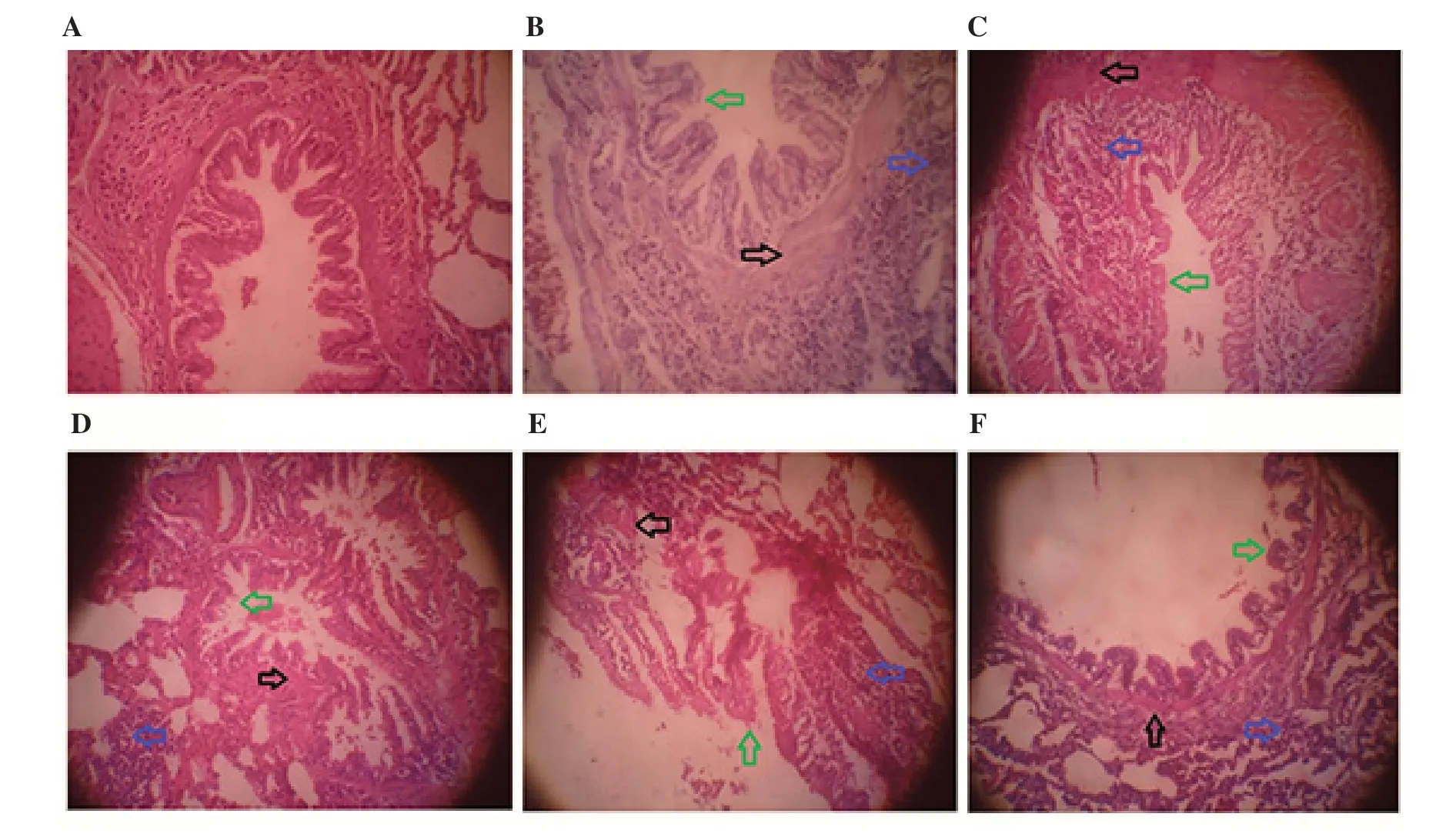
Figure 2.The lung pathological changes in control (A),asthma (B),and sensitized rats treated with dexamethasone (C) and rosmarinic acid (0.5,1,and 2 mg/kg) (D,E,and F,respectively) (magnification: ×400).Inflammation (blue arrow),muscle hypertrophy (black arrow),and mucine (green arrow).
The untreated sensitized group exhibited significant inflammation,muscle hypertrophy,and mucus plaques compared to the control group (P<0.05) (Table 2).RA improved OVA-induced histological changes in a dose-dependent manner (P<0.05) (Figure 2).
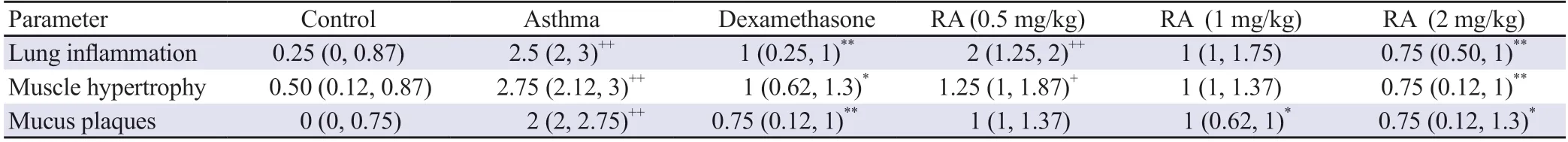
Table 2.The pathological changes observed after treatment with rosmarinic acid.
4.Discussion
Asthma,as a chronic inflammatory disease,is a major global health problem that can be prevented or controlled by complementary medicine.The inflammation of the respiratory tracts and the release of inflammatory cells and mediators contribute significantly to the increased responsiveness of the respiratory tracts[17].The presence of elevated levels of inflammatory cells,particularly eosinophils,has a significant impact on the manifestation and intensity of both chronic asthma and sudden asthma attacks[18].However,structural changes to the respiratory tract,including epithelial damage,sub-mucosal fibrosis,hypergenesis of the smooth muscle of the airways,and hypertrophy and hyperplasia of goblet cells,increase mucus production[19].According to the current study,the asthmatic lungs show increased inflammation (indicating inflammatory cell infiltration),hypertrophy of smooth muscles of the respiratory tract,and mucus plaques in the bronchioles and bronchi.The findings are similar to those from previous studies in asthmatic patients and experimental asthmatic animals due to the slowness of mucous membrane cells and the accumulation of mucus[20,21].
Since chronic inflammation is responsible for damage in the respiratory tract,treatments targeting lung inflammation can also slow the stages of structural changes if prescribed promptly and rapidly[22].Studies have demonstrated the protective effects of RA on heart disease[23].Furthermore,RA has been shown to have antiviral,antibacterial,and anti-inflammatory properties[24].RA possesses strong anti-inflammatory properties[25],as evidenced by clinical trials of patients with seasonal allergic rhinoconjunctivitis[26]and animal experiments of ear edema models[27].Researchers also showed that RA reduces histamine levels in allergic rhinitis[28].
In the present study,our findings demonstrated a noteworthy decrease in WBC as well as the percentages of eosinophils,monocytes,and neutrophils in the sensitized animals treated with RA.On the contrary,there was a notable rise in the proportion of lymphocytes observed in these groups when compared to the asthmatic group.Similar to our results,Shakeri et al.[29] reported that curcumin and Curcuma longa have a preventive effect on total and differential WBC in an animal model of asthma.
RA reduced neutrophils and eosinophils in the ear edema model[30].Additionally,Ocimum gratissimum and RA were evaluated in a mouse model of respiratory allergic reactions caused by Blomia tropicalis.This experiment showed a similar result to our current study,where RA significantly decreased total inflammatory cells,neutrophils,and eosinophils[31].Moreover,based on histological observations,the asthmatic group had severe inflammatory reactions,muscle hypertrophy with inflammatory cell infiltration,and mucus secretion,consistent with previous studies[32].
In another study,it was observed that administration of RA resulted in a decrease in inflammation and mucus production in the lung tissue of mice[33],which is consistent with the present study.Asthmatic rats exhibit structural changes in their respiratory tracts that correlate with inflammation in lung pathology.The structural changes in the lung are probably caused by inflammation[34].The current study shows that RA has an anti-inflammatory effect,which improves almost all lung changes.Furthermore,the smooth muscle response of ovalbumin-sensitized rats to methacholine was improved by treatment with different doses of RA.
In this study and other studies,the reduction of tracheal smooth muscle-specific and non-specific responsiveness after treatment with RA indicates that this compound with anti-inflammatory effects can alleviate asthma.Liang et al.demonstrated that RA at doses of 5,10,and 20 mg/kg (one hour before exposure to ovalbumin) inhibited inflammation and reduced airway responsiveness in asthmatic mice[35],which is consistent with the results of the present study.The various inflammatory agents,including reactive oxygen species(ROS),histamine,and arachidonic acid metabolism byproducts,can modify the airways.These modifications can lead to several changes such as the proliferation of goblet cells,enlargement of the submucosal glands,vascular congestion,thickening of the airway wall,increased smooth muscle mass and airway epithelial,and the development of mucous plaques that obstruct medium and small bronchi.Irreversible airflow obstructions characterize asthma due to structural changes in the airways[36].Eosinophils are the main source of endogenous oxidants that the epithelium of the respiratory tract produces[20].Asthma exacerbations are linked to heightened permeability of the pulmonary blood vessels,damage to the airway epithelium,and increased bronchial hyperactivity as a result of these oxidants.As a result of the increase in respiratory responsiveness in asthma[19],inflammation has been proven to be directly related to a reduction in the diameter of the respiratory tracts.
Additionally,previous studies have demonstrated that RA has antiinflammatory effects and reduces histamine and interleukin-4[33].Myricetin as a flavonoid found in many plants could exert an antiallergic effect against OVA-induced allergic rhinitis in mice via attenuated elevated serum levels of histamine,immunoglobulin E,leukotriene C4 and interleukins[37].The present study found that RA decreased inflammatory cells and lung pathological changes as well as reduced respiratory tract responsiveness to methacholine.It can be concluded from this study that RA effectively improves asthma symptoms caused by ovalbumin.However,the therapeutic benefits of RA on asthma need to be studied further in clinical trials.
Due to financial limitations,the levels of immunological (IgE,IgG,cytokines) and oxidative stress parameters as well as functional variables (lung function measured by plethysmography) were not measured in the current study.
In conclusion,the present study showed the ameliorative effect of RA on tracheal smooth muscle responsiveness and inflammatory cells in the BALF and lung pathological changes in OVA-sensitized rats.Therefore,RA could potentially be regarded as a therapeutic agent to be used for the improvement of asthma symptoms.However,further study is required to verify its efficacy.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Acknowledgments
The authors thank MS Lotfi,a pathological expert for her advice in preparation of pathological samples.
Funding
The authors received no extramural funding for the study.
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors’ contributions
VA conducted the experiments and obtained the data.DEE,MF,and SO helped to the study design and edited the manuscript.MRK designed and supervised the study,analyzed the data and prepared the manuscript.All authors are responsible for the design and evaluation of the study,read and approved the final manuscript.
 Asian Pacific Journal of Tropical Biomedicine2024年3期
Asian Pacific Journal of Tropical Biomedicine2024年3期
- Asian Pacific Journal of Tropical Biomedicine的其它文章
- Pyronaridine combined with diminazene aceturate inhibits Babesia in vitro and in vivo
- Icariin ameliorates viral myocarditis by inhibiting TLR4-mediated ferroptosis
- Capsosiphon fulvescens suppresses LPS-stimulated inflammatory responses by suppressing TLR4/NF-κB activation in RAW264.7 murine macrophages
- Th17/Treg balance and macrophage polarization ratio in lower extremity arteriosclerosis obliterans
