Outcomes and variables that impact pneumatic retinopexies
Maria V.Castanos, Daniel Vail, Oscar Otero-Marquez, Yash Shah, Avnish Deobhakta
New York Eye and Ear Infirmary of Mount Sinai, New York
10003, New York, USA
Abstract
● KEYWORDS: retina; pneumatic retinopexy;rhegmatogenous retinal detachment
INTRODUCTION
Rhegmatogenous retinal detachment (RRD) is a common ocular emergency, primarily managed with three methods of intervention: scleral buckle (SB)[1], pars plana vitrectomy (PPV)[2], and pneumatic retinopexy (PR)[3-4].The management of RRD has evolved over time, but currently the most common method of repair is PPV[5].The only method that can be completed as an in-office procedure, rather than in the operating room, is PR[6].
First described in 1986 by Hilton and Grizzard[7], PR was introduced as a method to repair RRDs without the need for taking patients to the operating room.It consists of an intravitreal injection of an expandable gas bubble which acts as a tamponade, followed by the application of laser to the retinal breaks.Proponents argue this method has faster visual restoration[8-9], decreased morbidity secondary to anesthesia[8],decreased cost[10-11], lower post operative complications[12], and a lower rate of cataract progression[13-14].
Indications for PR were originally defined by Tornambe and Hilton[15]in a multicenter, randomized, controlled clinical trial.These indications included the presence of one or more retinal breaks within one clock hour in the upper two thirds of the retina, and a sufficiently clear media to rule out the presence of other breaks.Since then, these indications have been expanded to include multiple quadrants, larger breaks, and even moderate proliferative vitreoretinopathy (PVR)[10,16].
Several studies have shown favorable outcomes of PR and support the use of this technique as primary management in patients who fit its established criteria[17-20].In 2019, the Pneumatic Retinopexy Versus Vitrectomy for the Management of Primary Rhegmatogenous Retinal Detachment Outcomes Randomized Trial (PIVOT)[8]compared PR versus PPV in the management of RRD.They defined specific anatomic criteria for patients included in the trial, which were the following:a single retinal break or group of breaks, no larger than one clock hour in the detached retina, all breaks in detached retina to lie above the 8 and 4 o’clock meridian, and breaks or lattice degeneration in attached retina at any location were allowed.They excluded patients with inferior breaks in the detached retina, media opacities, and PVR grade B or worse, with a total of 176 patients enrolled in the study, 81% of patients who underwent PR and 93% of patients who underwent PPV achieved primary anatomic reattachment.Notably, superior visual acuity (VA) within the first 12mo of follow up were reported for the PR group.Given these results, the authors concluded that PR is a viable primary method to manage RRDs.
The purpose of this study is to evaluate the efficacy of PR in patients undergoing PR as primary treatment for RRD and analyze the factors associated with success and failure in the studied population.
SUBJECTS AND METHODS
Ethical ApprovalThis study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the New York Eye and Ear Infirmary of Mount Sinai (STUDY-22-009900).Informed consent was was not required given retrospective nature of the study.The present study was a retrospective, single center study, based on a chart review of patients treated at New York Eye and Ear Infirmary of Mount Sinai between January 2017 and December 2021.An electronic medical record search was performed based on a combination of International Classification of Disease (ICD-10) and Current Procedural Terminology (CPT)codes.The ICD codes identified patients with RRD and the CPT codes identified laser procedures, vitrectomies, and PR.Only patients with RRD with PR as primary management method were included.Patients with previous PPV, SB,or RRD were excluded as well as patients with tractional,serous, or exudative retinal detachments.The minimum required follow up time after PR was defined as 1mo.The following data were taken from medical records: age, sex,days to presentation, gas used for procedure, lens status, VA at presentation, location, size, number of tears, macula, and fovea status (meaning whether the macula and fovea were attached at the time of initial presentation).Outcome data included anatomical success, VA, new or missed breaks noted intraoperatively that were not noted preoperatively,subsequent procedures performed, and duration of follow up.VA was taken at presentation, postoperative day one (POD1),postoperative week one (POW1), postoperative month one(POM1), and postoperative month three (POM3).Additionally,whether the PR was done to temporarily reattach the retina prior to scheduled PPV (“temporizing pneumatic”) was also recorded.
The primary outcome was single operation success, defined as anatomical reattachment after PR without requiring subsequent PPV or SB.Patients requiring re-bubble or multiple laser procedures were still considered a single operation success.A key secondary outcome measured best corrected visual acuity(BCVA) after PR.A separate risk analysis was done to identify and stratify risks associated with success and failure of PR.
Statistical AnalysisWe tabulated the total number of retinal breaks noted at patients’ initial exam, as well as the number and location of breaks noted in operative reports for all patients who were taken to the operating room for PPV or SB.The locations of breaks were defined in clock hours, and were additionally categorized by quadrant.We stratified the distribution of breaks according to the initial operative plans for patients to determine if patients undergoing temporizing PR had a different distribution of retinal breaks than patients receiving primary PR without plans for re-operation.
We illustrate the time to failure of primary PR across patients who did and did not meet PIVOT criteria using Kaplan Meier curves, with time-to-failure representing time from patients’initial procedure until they received surgical intervention, if needed.We specified Cox proportional hazards models to assess patients’ risk of pneumatic failure based on PIVOT criteria after adjusting for phakic status, fovea status, and patients’ time to presentation from their initial symptom onset.
RESULTS
A total of 179 eyes from 179 patients were included for the final analysis (Table 1).Mean time from symptom onset to presentation was 5.35d (median 3d), and mean time from presentation to PR was 0.15d (median 0).Average presenting VA was 0.76 logMAR (Snellen 20/100).The mean time from PR to PPV was 17.22d with a median of 6d.
The VAs at both presentation and POM1 for patients who underwent primary PR successfully were 0.58 (20/80) and 0.18 (20/32) respectively (Figure 1).The VAs at presentation and POM1 for patients who underwent primary PR and subsequent PPV were 0.92 (20/160) and 1.03 (20/200)respectively.The VAs at presentation and POM1 for patients who underwent a temporizing pneumatic were 1.24 (20/320)and 0.88 (20/160), respectively.VA at POM3 was available for 109 patients (60.89%) and was 0.22 (20/32), 0.68(20/100), and 0.75 (20/100), for successful PR, PR and PPV,and temporizing PR, respectively.
Patients who met PIVOT criteria had a statistically significant decreased risk of primary PR failing [hazard ratiov (HR) 0.29,P<0.01; Figure 2].Similarly, patients with fovea-on detachments at the time of presentation were less likely to fail primary PR(HR-0.53,P=0.02; Figure 3).Notably, phakic status and days to presentation did not show any statistically significant effect on outcome of primary PR.

Table 1 Study demographics n (%)
For patients who underwent PPV (n=96), information in the operative report regarding intraoperative exam and location of identified breaks was available for 60 patients (62.5%).Discordance between the pre-operative exam and the intraoperative exam was substantial—48 patients who received PPV(50%) had either new or missed breaks listed in their operative report that were not noted in the initial exam.Interestingly, the majority of missed breaks were located temporally in both the right (n=34 of 45 total missed breaks, 76%) and left (n=32 of 47 total missed breaks, 68%) eyes (Figure 4).
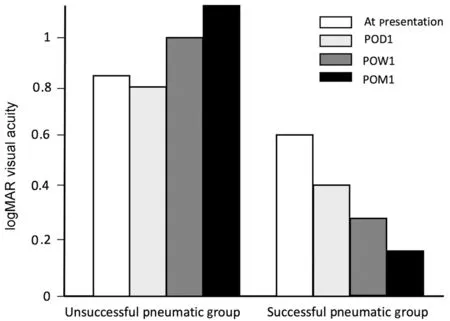
Figure 1 Visual acuity progression of both groups POD1: Postoperative day one; POW1: Postoperative week one; POM1: Postoperative month one.

Figure 2 Kaplan Meier survival curve by PIVOT criteria PR:Pneumatic retinopexy.
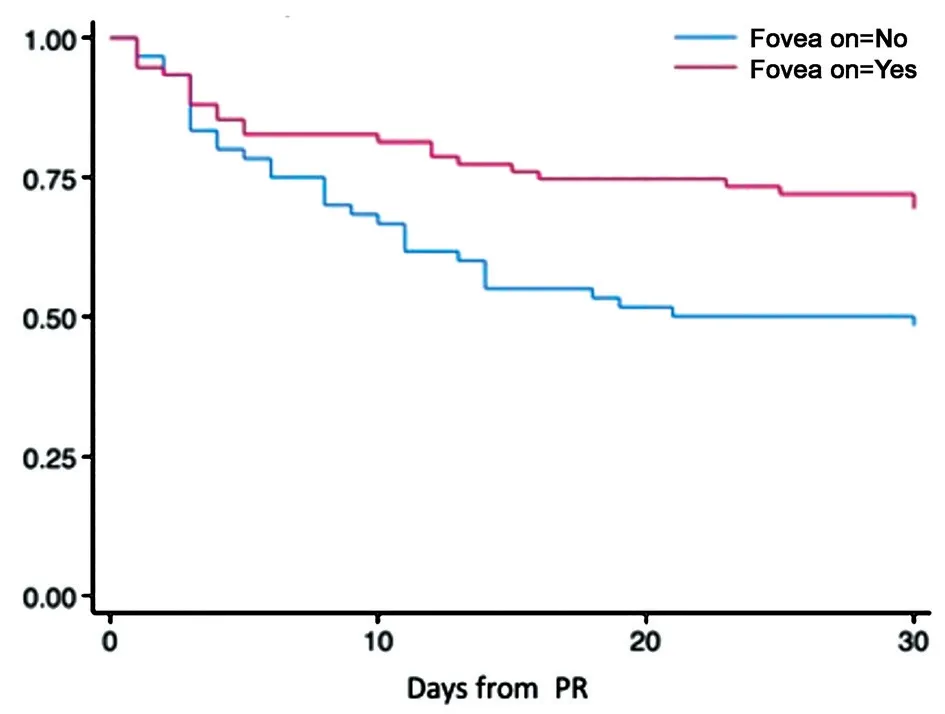
Figure 3 Kaplan Meier survival curve by fovea status PR: Pneumatic retinopexy.
DISCUSSION
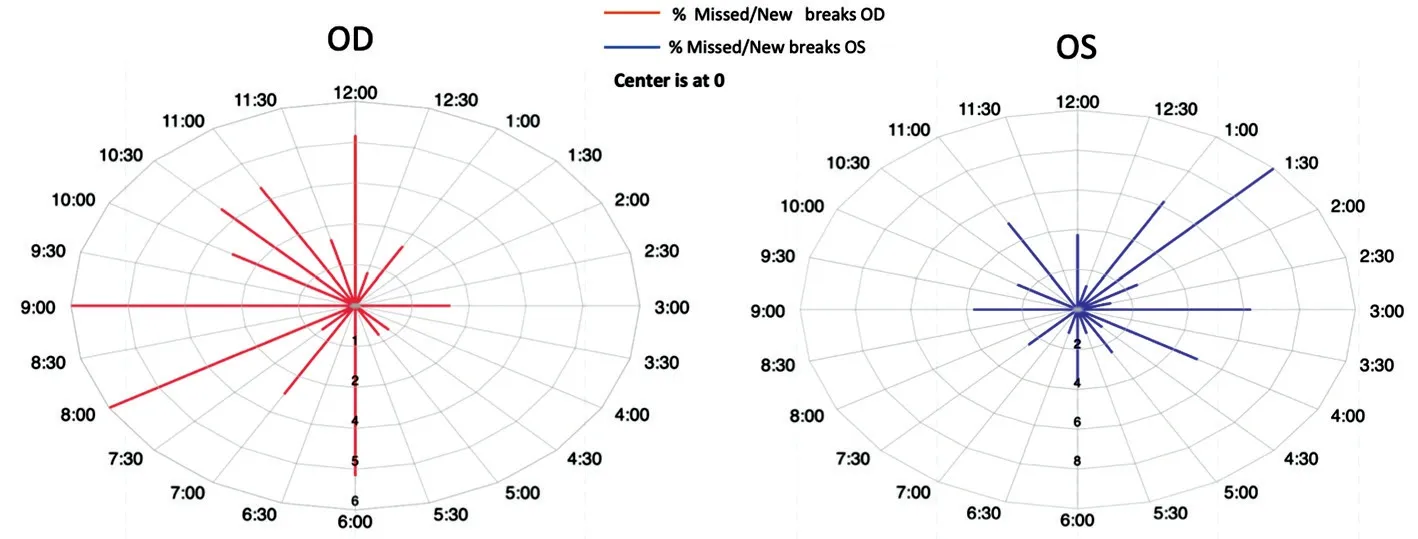
Figure 4 Map of total missed/new breaks on both eyes.
The single operation success rate for PR in the present study is 46.37%, with 53.63% requiring secondary surgery.When correcting this number for temporizing pneumatics,the single operation success rate of our study was 51.87%,with 48.12% requiring secondary PPV or SB.Correcting for temporizing pneumatics when considering success rate was considered reasonable given that the PR was done as a prelude to PPV.Regardless, the success rate of the current study is lower than that which was previously reported in the literature.The PIVOT trial[8]reported 81% single operation success acknowledging, in similar fashion to the present study,that secondary interventions such as additional laser or rebubbling should be considered a successful outcome.In their paper, Tornambe and Hilton[15]reported an 82% success rate.However, a more recent multicenter study[19]from the IRIS registry reported a single operation success of 68.5%, and a study similar to the present study by Zaidiet al[18]performed at a single academic center, had a single operation success rate of 66%.
Previous studies have proposed that patients that undergo PR tend to have faster VA restoration than those that undergo primary PPV or SB.A key finding in the PIVOT trial was that patients who had PR achieved superior VA when compared to those that underwent PPV at every point up to the 12mo follow up wherein BCVAs from both groups aligned.Similarly, in our study, patients with successful PR had better BCVA, both at POM1 and POM3, than those that required further surgery.At the 3mo follow up, the BCVA for the successful PR group was 20/32, while the unsuccessful PR group was left with a VA of 20/100.The VA achieved by the successful PR cohort correlates with previous studies, particularly the PIVOT trial which reported a final BCVA of 20/25 in patients with a successful PR[8].Additionally, in a study published in 2021[21],patients who underwent PR had a final mean Snellen VA of 20/44.Of note, it is possible that the difference in BCVA in our two cohorts could be attributed to the fact that patients that failed the initial PR had worse BCVA at presentation than those that were successful.Regardless, the group who failed PR still showed significant improvement between presentation and follow up.This finding seemingly indicates that in some selected cases, PR can be pursued initially and if it fails,a subsequent procedure can be done with improvement in visual acuity.Similarly, when we look at the 19 temporizing pneumatic patients, they had an average Snellen VA at presentation of 20/320 and an average POM3 Snellen VA of 20/160.The temporizing pneumatic group had improvement in VA but further studies should be done to compare with patients that undergo only PPV.Previous studies have suggested that PR does not adversely affect visual potential in case additional surgery is needed[15,17,22-26].
In our analysis, the PIVOT criteria and fovea status were found to significantly decrease the risk of primary PR failure(HR=0.29,P<0.05, HR=0.53,P<0.05; Figures 2 and 3).The PIVOT criteria, derived from the PIVOT trial, establishes which patients qualify for PR based on initial exam and location of breaks.From our cohort, the PIVOT criteria was met by 66.29% of all patients and by 89.15% of patients who had successful PR.Macula status has been studied in previous papers[8,15,27-29]and they have not shown any correlation with PR outcome.However, fovea status specifically has not been studied by previous authors.In our cohort, fovea-on status conferred a decreased risk of PR failing, which was somewhat confounding.We hypothesize that part of the explanation was that surgeons were more prone to taking patients to the OR when the fovea was off, thus ensuring a PR failure in those cases.
Several characteristics such as myopia, phakic status[30], days to presentation[31], and age have been described as risk factors for anatomic failure of PR.Interestingly, in our study these factors did not increase the risk of failure for PR.Notably however, the operative exam was available for 66% of patients who underwent PPV, and a discordance in pre-operatively noted breaks with those found during the operation were found in 50% of the cases.New or missed breaks have been reported in previous studies and range from 16% to 28% of cases[18,27,32-33].These breaks are important since, had they been noted pre-operatively, they often would exclude a patient from a primary PR criterion initially and thus changed the course of management.In our study, the majority of new or missed breaks were found temporally for both right and left eyes (Figure 4).If these breaks are considered as missed in the initial exam, we hypothesize that the temporal area poses a difficulty to the examiner due to the interposition of the nose.On the other hand, if the breaks are considered to be new breaks, one study proposed this could be a complication from the gas bubble causing traction on the vitreous body[18].In their original paper, Tornambe and Hilton[15]described the risk of new breaks with PR to be 13%.Indeed, one study showed that new or missed breaks are a significant factor resulting in poor outcomes for PR, increasing the risk of failure by three to fivefold[27].
The present study has limitations.The retrospective nature of the study limits the availability and standardization of the data collected, as well as creates issues with controlled comparisons.In addition, our long term follow up is limited given that many patients are either lost to follow up or sometimes return to the referring provider.
In conclusion, this study demonstrates the effectiveness of PR in patients who meet PIVOT criteria.It additionally shows that PR can sometimes be done as a temporizing measure in patients that require further surgery and cannot be taken to an operating room in a timely manner.It also demonstrates that a good initial exam for possible missed breaks, particularly in the temporal locations of the affected eye, may be virtuous in preventing potential anatomic failure with PR.As always,further studies should be conducted to look into additional factors that could impact PR outcomes.
ACKNOWLEDGEMENTS
Conflicts of Interest: Castanos MV,None;Vail D,None;Otero-Marquez O,None;Shah Y,None;Deobhakta A,None.
 International Journal of Ophthalmology2024年3期
International Journal of Ophthalmology2024年3期
- International Journal of Ophthalmology的其它文章
- Meibomian glands segmentation in infrared images with limited annotation
- Artificial intelligence for the detection of glaucoma with SD-OCT images: a systematic review and Meta-analysis
- Overexpression of TRPV1 activates autophagy in human lens epithelial cells under hyperosmotic stress through Ca2+-dependent AMPK/mTOR pathway
- Dry environment on the expression of lacrimal gland S100A9, Anxa1, and Clu in rats via proteomics
- Semaphorin 7A impairs barrier function in cultured human corneal epithelial cells in a manner dependent on nuclear factor-kappa B
- Novel MIP gene mutation causes autosomal-dominant congenital cataract
