Effectiveness and safety of early lens extraction during par plana vitrectomy for proliferative diabetes retinopathy with mild cataract: a randomized clinical trial
Wei-Bo Feng, Lei Zheng, Ying-Qi Li, Yong-Hao Li,4, Guo-Ming Zhang, Xian Wang,Bing-Qian Liu, Ling Jin, Yi-Nuo Huang, Yang-Fan Yang, Zi-Dong Chen, Da-Hui Ma,Qing-Shan Chen, Chao-Jun Qin, Bing-Min Feng, Zhu-Min Yang, Xing Huang,Cheng-Jie Yang, Sheng-Hui Liu, Ming-Xing Wu
1State Key Laboratory of Ophthalmology, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou 510275, Guangdong Province, China
2Shenzhen Eye Hospital Affiliated to Jinan University,Shenzhen 518040, Guangdong Province, China
3The Affiliated Hospital of Guizhou Medical University,Guiyang 550004, Guizhou Province, China
4Guangzhou Aier Eye Hospital, Guangzhou 510000,Guangdong Province, China
Abstract
● KEYWORDS: lens extraction; pars plana vitrectomy;proliferative diabetic retinopathy; cataract; simultaneously operations
INTRODUCTION
Diabetic retinopathy (DR), one of the leading causes of irreversible blindness worldwide, is frequently accompanied by lens opacities[1-4].Pars plana vitrectomy(PPV) and cataract surgery are both necessary for patients with proliferative diabetic retinopathy (PDR), and the procedure can be performed either as a combined approach or as a subsequent approach according to the degree of lens opacity.
Conventionally, a subsequent approach is preferred for patients with PDR and mild cataracts.In these cases, the surgeons may preserve the lenses with accommodation after PPV and perform subsequent phacoemulsification with an intraocular lens (IOL) implantation 9-24mo later due to cataract aggravation[5-14].However, the subsequent approach may have a potential risk of outcomes that fall short of expectations.First, cataract aggravation is almost ineluctable and observed in 79%-95% of phakic patients after PPV[8-14].Complicated cataracts may not only compromise visual rehabilitation in patients with PDR but also obscure the evaluation of retinal conditions after PPV[5-10].In addition, fluctuations in the anterior chamber, zonular dehiscence, macular edema (ME),neovascular glaucoma (NVG), vitreous hemorrhage (VH),and lens subluxation are prevalent during or after the cataract surgery in patients with PDR and history of PPV[15-20], bringing additional challenges and inconveniences for both the surgeons and patients with PDR.
To address the challenges and inconveniences of ineluctable cataract aggravation after PPV alone, a combination of PPV,phacoemulsification, and IOL implantation may be a feasible alternative, which has become more prevalent in recent years.In the combined surgery, the surgeons can have a better surgical view during PPV and access the vitreous base and retinal periphery more easily without a lens.Moreover,simultaneous management of anterior and posterior segment pathologies can not only help patients achieve their best visual outcomes earlier but also reduce the number of surgeries and medical burdens.Several previous studies have been conducted, which demonstrated that the combined surgery was effective and gratifying, with optimal prognoses in patients with PDR and dense cataracts[21-25].
However, early lens extraction during PPV in patients with PDR and mild cataracts remains controversial.Currently,most studies on the combined surgery are retrospective observational studies, focusing on patients with PDR and dense or obvious cataracts obscuring the surgical view[21-25].Few studies have demonstrated the application and benefits of earlier lens extraction during PPV for PDR patients with mild cataracts, and there is a lack of randomized clinical trials comparing these two surgical approaches as well.Nevertheless, another major concern regarding the safety of combined surgeries has also emerged.Some previous studies have mentioned that adverse events, such as NVG, were observed more frequently after the combined surgery than after PPV alone[26-27].In addition, other studies have also proven that with the development of surgical technology and antivascular endothelial growth factor (anti-VEGF), the adverse events of the combined surgery have been controlled well in recent years, and no significant differences were found compared to those with PPV alone[18,24,28].Since contradictory opinions have emerged over the years, debates regarding the safety of different surgical approaches (one combined surgery or two sequential surgeries) need to be addressed.Hence,with the advances in modern surgical technologies, some previous surgical opinions may evolve correspondingly, and further discussion as well as clinical evidence regarding the applications of early lens extraction during PPV for patients with PDR and mild cataracts are required.
Given the current variability in reporting and the associated heterogeneity, there is no unanimity among the surgeons concerning the most effective and safest surgical approach for patients with PDR and mild cataracts.Therefore, we conducted a multicenter randomized clinical trial to ascertain whether the patients with PDR and mild cataracts could also benefit from early lens extraction during PPV and compared the effectiveness and safety of the two conventional sequential surgeries.
SUBJECTS AND METHODS
Ethical ApprovalThis study adhered to the tenets of the Declaration of Helsinki and was approved by the ethics committees of each center (2020KYPJ167, k20201130-03,2021047K).Written informed consent was obtained from each patient after thoroughly describing the experimental procedures and details.The trial was registered at ClinicalTrials.gov(NCT04729023) and followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Study Design and ParticipantsThis multicenter randomized controlled study was conducted in three different hospitals in China: 1) Zhongshan Ophthalmic Center, Sun Yat-sen University; 2) Shenzhen Eye Hospital, Affiliated to Jinan University; 3) The Affiliated Hospital of Guizhou Medical University.A total of 122 patients with PDR (allowing for up to 20% loss) were recruited based on the primary outcome.Patients with PDR and mild cataracts were assessed as potentially eligible based on the inclusion and exclusion criteria.Only one eye per participant was included in this study.
Inclusion criteria: 1) age over 45y, men or women; 2)diagnosed with type 1 or type 2 diabetes; 3) PDR according to the International Severity Scales[29]; 4) mild lens opacities(C3N3P3 or below), according to LOCSIII[30]; 4) best corrected visual acuity (BCVA) ≥1 letter on Early Treatment of Diabetic Retinopathy Study chart (ETDRS) on the day of randomization; 5) able and willing to sign informed consent.Exclusion criteria: 1) long-standing retinal detachment(RD) for more than 3mo; 2) RD for more than one posterior quadrant or macular area involved; 3) combined tractionrhegmatogeneous RD (equal or more than 3 retinal tears and/or at least 1 giant tears); 4) low vision or blind on the other eye; 5) other macular diseases, including diabetic ME, macular epiretinal membrane, age-related macular degeneration, and polypoidal choroidal vasculopathy; 6) ocular trauma; 7) glaucoma; 8) hereditary retinopathy; 9) severe lens opacities before the surgery (LOCSIII: C4N4P4 or above);10) uncontrolled glycemia, blood pressure >180/110 mm Hg,acute congestive heart failure, significant renal disease or other conditions, in the investigators’ opinion, that will preclude participation in this study; 11) history of previous intraocular surgeries or intraocular drug injections.In this study, each patient will receive ultrasound B scan and digital fundus camera for the preoperative evaluation.Participants with RD requiring silicon oil tamponade (macular area involved, longstanding for over 3mo, or combined traction-rhegmatogeneous)will be excluded.Yet those with C3F8or filtered air tamponade will still be included.
Arms and InterventionThis study had two parallel groups:the combined and subsequent groups.In the combined group,participants simultaneously underwent PPV combined with phacoemulsification and IOL implantation.In the subsequent group, participants received PPV first, and subsequent phacoemulsification with IOL implantation was performed 6mo later.
Surgical Procedure
Pars plana vitrectomyAll participants will receive anti-VEGF (0.5 mg; KANGHONG, China) intravitreal injection for 1wk before an extensive 3-port PPV using 25-gauge instrument.All PPV surgeries will be performed by three experienced surgeons in each hospital respectively under retrobulbar local anesthesia.Using non-contact lenses,posterior hyaloid separation, removal of the posterior vitreous membrane and peripheral vitrectomy will be performed, and then manual delamination, dissection, and segment will be used to remove proliferative tissues.Membrane dissection and segmentation will be performed when necessary to eliminate all tangential tractions.Panretinal endophotocoagulation (PRP)will be performed adequately from posterior region up to the ora serrata in four retinal quadrants with the aid of scleral depression under air or fluid condition.Air-fluid exchange and C3F8tamponade will be performed when an iatrogenic retinal tear/rhegmatogenous RD are identified intraoperatively.Triamcinolone acetonide will be injected intraocularly at the end of PPV if conditions allowed.
P h a c o e m u l s i f i c a t i o n a n d I O L i m p l a n t a t i o nPhacoemulsification will be routinely performed through a 3.2-mm clear corneal incision, with implantation of an acrylic foldable IOL (SN60WF, Alcon, USA).The keratometric values, axial length, anterior chamber depth and other biometers are measured preoperatively by optical coherence interferometry like IOL Master 700 (Carl Zeiss Meditec AG,Jena, Germany).The IOL power calculation will be performed using the Barret U II.
After these surgeries, all participants in both groups will receive tobramycin and dexamethasone ophthalmic eye drops(TobraDex, Norvaritis), tobramycin and dexamethasone ointment (TobraDex, Norvaritis), pranoprofen eye drops(Pranopulin, Senju) as postoperative medication.
Randomization and MaskingAll potentially eligible participants were randomly allocated 1:1 to the combined or subsequent groups through block randomization by an independent staff member who did not perform the trial.A statistician not involved in the trial generated three separate random sequences for each hospital using an online random number generator (www.randomization.com), where A and B represent the groups.
This study was an open-label trial.The participants and surgeons were not masked to the treatment assignment.However, the individuals responsible for enrollment, screening,and measurement did not know the randomization assignment.The surgeon was blinded to the assignment until surgery was performed.In addition, the data analysis was compiled by a masked statistician.
Assessment and Follow-upThe primary outcome of this study was the change in the BCVA from baseline to 6mo after PPV.Secondary outcomes included vision-related quality of life measured using the National Eye Institute 25-Item Visual Function Questionnaire[31](VFQ-25, Chinese edition) composite score, postoperative complications,surgical expenses, and duration of work incapacity.NVG,ME, recurrent VH, and recurrent RD were selected as major postoperative complications for analysis.
A one-year follow-up plan was scheduled for each participant.Generally, the follow-up visits were scheduled at 1wk, 1, 3, 6,and 12mo after surgery.If any adverse events or discomfort occurred during the follow-up, the patients could contact their ophthalmologists at any time, regardless of the arranged follow-up plan.At each follow-up visit, postoperative funds evaluation was conducted using fundus photograph and optical coherence tomography (OCT).Evaluations of the glycemia, blood pressure and other general health conditions were conducted during the follow-up period.Corresponding recommendations or monitoring were also provided for each participant to keep them in a stable general health condition.
Statistical AnalysisThe baseline demographic and clinical characteristics of the participants were described as mean±standard deviation (SD) or median [interquartile range(IQR)] for continuous variables and frequency (percentage) for categorical variables.The normality of the continuous data was checked using the Shapiro-Wilk test and histograms.

Table 1 The baseline characteristics for the eligible participants in both groups
The intention-to-treat (ITT) analysis, which included all patients who were involved in the randomization, was applied to the change in the BCVA at the 6-month follow-up(primary outcome) and VFQ-25 scores (secondary outcome).All missing data were imputed using multiple imputations,which created 20 copies of the data, and chained equations imputed missing values.The combined results were obtained using Rubin’s rule.A per-protocol (PP) analysis was also performed, including all participants who completed the trial according to the protocol.A linear regression model calculated the unadjusted mean difference and 95% confidence interval(CI) between the trial arms.Univariate and multivariate linear regression models were used to estimate the adjusted mean difference and 95%CI between the trial arms for the primary outcome.All the variables withP<0.20 in the univariate regression analysis were included in the multivariate regression analysis.The center effect was assessed using the likelihood ratio test, intraclass correlation (ICC), and comparisons of the mean differences in the primary outcomes among centers.The surgical safety, including adverse events and complications,was compared using the Chi-square or Fisher’s exact test among patients whose safety statuses were known.The medical expenses and the time of incapacity to work were compared using a two-sample independentt-test or Wilcoxon rank-sum test.All analyses were conducted using the STATA software (version 16.0; StataCorp, College Station, TX, USA),and the statistical significance was set atP<0.05.
RESULTS
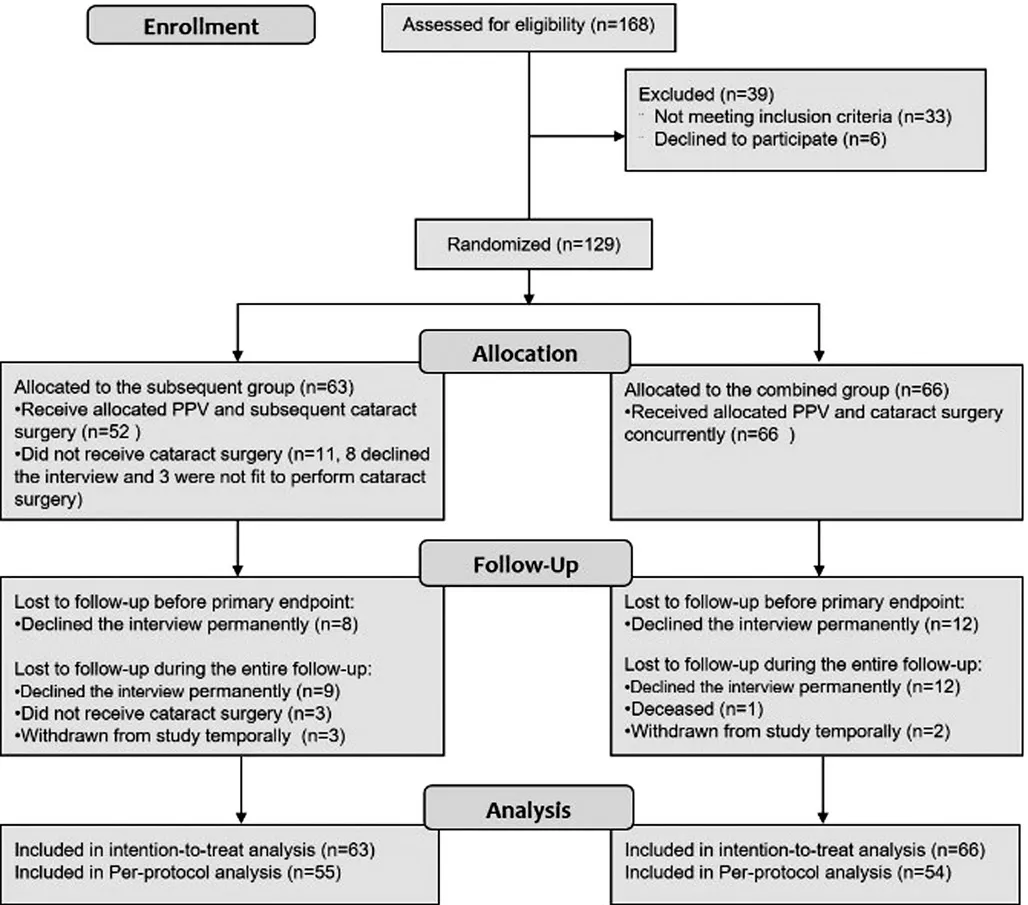
Figure 1 Flow diagram of participants according to CONSORT Statement PPV: Pars plana vitrectomy.
Recruitment, Allocation, and Follow-upFrom February 1st, 2021 to October 28th, 2021, 168 patients with PDR were assessed for eligibility, of which 129 were recruited and randomized (66 and 63 in the combined and subsequent groups, respectively).Generally, the baseline characteristics of the two groups were balanced and the details are provided in Table 1.Most participants strictly adhered to the study protocol and received the corresponding therapy (Figure 1).In the combination group, all 66 participants underwent PPV combined with phacoemulsification.In the subsequent group,all participants received PPV alone, and 52 participants underwent subsequent cataract surgery 6mo later (±1wk).A few participants (n=11) in the subsequent group did not undergo subsequent cataract surgery owing to either loss to follow-up or failure to meet the surgical criteria due to uncontrolled general conditions or complications (three).Nine patients in the combined group and seven in the subsequent group underwent surgery in both eyes; however, only eligible eyes with worsened BCVA were included for each participant.The last follow-up visit was on September 2nd, 2022.A total of 109 (84.50%) patients reached the primary endpoint at 6mo,and specific clinical data were successfully collected from 104 participants (80.6%) at the end of the follow-up.

Table 2 The difference of unadjusted change of BCVA and VFQ-25 scores between groups

Table 3 Intention to treat analysis of linear regression for estimating adjusted mean difference between trial arms on primary outcome(n=129)
Change in BCVA and VFQ-25 Composite ScoresDuring the follow-up period, BCVA in the ETDRS chart was compared from baseline to 6mo after PPV.As shown in Table 2,in the ITT analysis, the median BCVA baseline was the same 10 letters in both groups.Six months after the surgeries, a significant difference (P<0.001) was observed between the combined group (57.58±20.24 letters) and the subsequent group (41.16±22.02 letters).The BCVA improvement from the baseline provided by combined surgery (36.90 letters; 95%CI,30.35-43.45 letters) demonstrated significant superiority(14.50 letters; 95%CI, 5.09-23.91;P=0.003) to PPV alone(22.40 letters; 95%CI, 15.55-29.24).The PP analysis verified the results of the ITT analysis.To avoid interference from other variables, a linear regression was performed to estimate the adjusted mean difference in the change in BCVA between the trial arms (Table 3).In the multivariable linear regression, the adjusted difference (16.43 letters; 95%CI, 8.77-24.08 letters)was still statistically significant (P<0.001) between the two groups.After subsequent cataract surgery, the BCVA in the two groups demonstrated no significant difference at month 12.VFQ-25 composite scores were recorded as another evaluation of the visual function.Consistent with BCVA, there was no significant difference in the VFQ-25 composite scores between the two groups at baseline (Table 2).Six months later, the VFQ-25 composite scores in the combined group significantly improved to a mean of 71.24±16.82, whereas the mean score in the subsequent group were only 59.39±17.49.The improvement in the combined group (17.69; 95%CI,12.98-22.41) was significantly better (11.17; 95%CI, 5.16-17.18;P<0.001) than the subsequent group (6.52; 95%CI, 2.63-10.41).After subsequent cataract surgery, the two groups revealed no significant difference in the VFQ-25 composite scores at month 12.
Safety and Adverse EventsThe most common postoperative complication was ME, followed by NVG, while RD and ME were relatively infrequent (Table 4).These conditions were similar across all three hospitals.In this study, the overall NVG rate after two sequential surgeries was significantly higher (17.65%) compared to one combined surgery (3.77%).Generally, the safety of combined surgery was promising during the entire follow-up period.A few complications emerged, and most were first diagnosed within 6mo after the combined surgery, except for one participant with newly emerging ME during 7-12mo.In the subsequent group,postoperative adverse events were observed after both PPV and cataract surgery.During 1-6mo, similar conditions with infrequent adverse events were found in the subsequent group after PPV alone.However, more frequent occurrences of ME and NVG have been observed after subsequent cataract surgery during 7-12mo.Most NVG cases (77.7%) and nearly half of the ME cases (46.1%) in the subsequent group were first diagnosed within 7-12mo.
Generally, most ME cases were transiently detected 1wk after surgery and recover spontaneously within 1mo.A few cases of refractory or exacerbated ME were treated with intravitreal anti-VEGF or PRP and all of them were successfully treated when BCVA at 6 and 12mo were measured.Four patients with recurrent RD and two with VH received additional PPV.Bilateral fundus fluorescence angiography (FFA) was performed as an additional examination in all NVG patients,and non-perfusion zones on FFA were detected among them.Anti-VEGF therapy, PRP, trabeculectomy,etc., were allocated as treatments according to the severity of the condition.
Operation Details and Intraoperative ComplicationsAll surgical procedures were carefully conducted by experienced surgeons in each hospital, and adequate PRP (from the posterior region up to the ora serrata in four retinal quadrants with scleral depression) was allocated to all participants in both groups during PPV.Postoperative evaluation regarding retina conditions and the PRP treatment during PPV were conductedfor all participants at each follow-up visit using fundus photograph and OCT.No significant differences were found in the PRP spots, total surgical mean time, economic mean expenses and most operation details, except for the duration of work incapacity.In the subsequent group, the duration of work incapacity (22.54±9.11d) was almost twice as much as(P<0.001) that of the combined group (12.44±6.48d).During the surgeries, the most common intraoperative complications were iatrogenic retinal breaks/detachments with 14 cases of unplanned silicone oil tamponade (five in the combined group and nine in the subsequent group), followed by posterior capsular rupture with 6 cases of IOL ciliary sulcus fixation(four in the combined group and two in the subsequent group).No statistic differences of these intraoperative complications were found between the two groups.For the eyes with unplanned silicone oil tamponade, a regular follow-up was scheduled to evaluate the recovery conditions and the oil was removed 3-5mo after vitrectomy.When BCVA at 6 and 12mo were measured, no participants in this study were with silicone oil tamponade.Cataract surgery was not performed at the time of oil removal.

Table 4 Comparison of complications in the two groups n (%)
DISCUSSION
Currently, the guidelines and position statements regarding the indications for lens extraction during PPV in patients with PDR and mild cataract are limited, and decisions regarding surgical approaches are usually made by individual surgeons depending on their own experiences.In this multi-center randomized clinical trial, clinical evidences showed that early lens extraction during PPV could also be a promising surgical approach for patients with PDR and mild cataracts aged >45y.For long-term visual prognosis, there was no significant difference in the BCVA improvement or VFQ-25 composite scores between the two groups at 12mo.However, the combined surgery demonstrated the advantages of earlier recovery for patients with PDR, aged >45y, with mild cataracts.In the early postoperative period, the participants in the combined group with IOL were not superior to those in the subsequent group with mild cataracts.However, as the cataract was exacerbated in the subsequent group, a gradual decrease in BCVA was observed shortly (within 3mo) after PPV alone.Until 6mo, the BCVA improvement in the combined group was significantly superior to that in the subsequent group.In this study, the mean difference in the BCVA improvement 6mo after PPV between the two groups was 14.50 letters, which was almost consistent with previous study results[21-24].After the subsequent cataract surgery, no statistic difference was found between the two groups at 12mo, which also verified that the worsen visual prognosis at 6mo in the subsequent group was due to cataract aggravation and the surgical technique were comparable between the two groups.Since advanced age, diabetes, and intraocular surgery were the risk factors for lens opacities[10-12], cataract aggravation and corresponding compromised visual rehabilitation in patients with PDR aged over 45y were observed within a few months after PPV in our study.Hence, regarding the effectiveness of long-term visual rehabilitation, the combined surgery was comparable to the conventional two-step surgeries (PPV with sequential cataract surgery), but it could help patients achieve their best visual outcomes earlier.From our perspective, patients with PDR and mild cataract aged >45y could also benefit from early lens extraction during PPV.
Regarding adverse events, the safety of the combined surgery is also gratifying.In this study, infrequent occurrences of ME, RD, and VH were found in both groups without significant differences.However, the total NVG rate after two sequential surgeries in the subsequent group was higher than that in the combined group (17.65%vs3.77%).This seems to be contradictory to some previous results that severe inflammation and complications might be induced after combined surgery[26-27].In this study, all eligible patients in both groups received intravitreal anti-VEGF injections 1wk before the PPV surgery, and triamcinolone acetonide was injected intraocularly at the end of PPV surgery if the conditions allowed.Several previous studies have shown that the risk of NVG and inflammation after the combined surgery could be well controlled by using anti-VEGF and advanced surgical techniques[18,24,28].Meanwhile, intraocular injections of steroid hormone drugs could also help control the inflammation in patients with PDR after the combined surgery[32].Hence, in this study, anti-VEGF drugs and triamcinolone acetonide were two major contributors to inflammation control and infrequent occurrences of complications after the combined surgery.However, in the subsequent group, both PPV and subsequent cataract surgery could be the contributors to the overall NVG risk (17.65%).Consistent with the combined group, a few NVG cases were observed infrequently after PPV alone with adequate PRP and anti-VEGF drugs in the subsequent group during 1-6mo.However, NVG cases were observed more frequently after the subsequent cataract surgery during 7-12mo, which became the major contributor to the overall NVG risk (17.65%) in the subsequent group.In previous studies, approximately 11%-20% of patients with PDR were reported to suffer from NVG after PPV or cataract surgery without anti-VEGF intravitreal injections[18-20].In our study, no anti-VEGF injection was administered before the subsequent cataract surgery, and almost consistent results were observed in the subsequent group during 7-12mo.Without additional preoperative anti-VEGF intravitreal injections, the inflammation induced by cataract surgery might be a reason for the higher occurrence of NVG in the subsequent group than in the combined group[33-35].From our perspective, with advanced surgical equipment, meticulous surgical techniques,anti-VEGF drugs, triamcinolone acetonide, and adequate PRP,no additional risks of complications were observed in patients with PDR and mild cataracts aged >45y after the combined surgery.
Another advantage of the combined surgery was its potentially lower cost to the overall health system[36].In our study, no significant differences were found in the total surgical mean time and economic mean expenses.However, the subsequent cataract surgery almost doubled the duration of work incapacity, causing inconvenience and increasing indirect costs to patients with PDR.Furthermore, NVG was frequently observed in patients with PDR after the cataract surgery in the absence of anti-VEGF treatment.To reduce the risk of NVG and avoid dense cataracts, we suggest that the subsequent cataract surgery after PPV should not be delayed too much.Routine FFA examinations in patients with PDR before the cataract surgery may also be beneficial.If a non-perfusion zone is detected, PRP, anti-VEGF intravitreal injections, and other interventions are highly recommended.However, these supplemental examinations and treatments may significantly increase medical costs.
Admittedly, early lens extraction during PPV may not be suitable for every PDR patient and combined surgery also has some downsides, one of which is a higher demand of surgical skills and equipment.In our study, all surgeries were performed by experienced specialists with advanced surgical device and drugs.Intraoperative complications like posterior capsular rupture and iatrogenic retinal breaks were observed occasionally in both groups without statistical difference.Another major concern regarding early lens extraction during PPV is the loss of accommodation.In our study, the average age of the participants was 55-59 years old.For elderly patient with existing presbyopia at baseline, the downside of pseudophakic eye without accommodation was limited.It should also be noted that if silicone oil tamponade was used,lens extraction during PPV might increase risk of silicone oil migration[9].In our study, severe RD with silicone oil tamponade was excluded and most participants received balanced salt solution intraocular tamponade.
This study had some limitations.First, the recruitment numbers in the three hospitals were not well balanced.However, no center-effect was found and the results in different center were homogeneous.Second, the mean age of participants in the two groups was statistically different.However, from clinical perspective, the impact of the mean age difference(4.4y) among elderly patients was minor in this study, and no statistical difference on multivariable linear regression for the primary outcome (Table 3) was found due to age variable.Hence, the baseline characteristics in both groups were still generally balanced.Third, owing to the COVID-19 pandemic,some participants were lost to follow-up.However, the sample size we calculated in study design allowed for up to a 20%loss of participants.The actual loss rate did not exceed 20%and the study results were still reliable and valid.Fourth, there was no regular follow-up in the combined group for 7-11mo.However, ocular examinations were still advised every 3mo in these participants without compulsive requirement and all participants were allowed to contact their ophthalmologist at any time if discomfort emerged.Fifth, the follow-up schedule was limited to 12mo.To investigate the long-term prognosis of PPV combined with cataract surgery, further study with longer follow-up time is required.
In conclusion, we conducted this multi-center randomized clinical trial and some valuable evidences were exhibited that patients with PDR and mild cataract aged >45y could also benefit from early lens extraction during PPV.With advanced surgical technologies, meticulous surgical procedures and adequate PRP, anti-VEGF drugs and triamcinolone acetonide,combined surgery demonstrated no obvious compromised clinical outcomes compared with those of conventional two sequential surgeries.From our perspective, it could be beneficial to combined the PPV and early lens extraction in patients with PDR and mild cataract aged >45y to avoid an inevitable second surgery and achieve their best prognoses earlier.
ACKNOWLEDGEMENTS
The authors thank Xiang Chen MD, PhD (State Key Laboratory of Ophthalmology, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases,Zhongshan Ophthalmic Center, Sun Yat-sen University, China)for assistance with article writing and guidance.We also thank the participants in this study, their families, and the research staffat each center.
Conflicts of Interest: Feng WB,None;Zheng L,None;Li YQ,None;Li YH,None;Zhang GM,None;Wang X,None;Liu BQ,None;Jin L,None;Huang YN,None;Yang YF,None;Chen ZD,None;Ma DH,None;Chen QS,None;Qin CJ,None;Feng BM,None;Yang ZM,None;Huang X,None;Yang CJ,None;Liu SH,None;Wu MX,None.
 International Journal of Ophthalmology2024年3期
International Journal of Ophthalmology2024年3期
- International Journal of Ophthalmology的其它文章
- Meibomian glands segmentation in infrared images with limited annotation
- Artificial intelligence for the detection of glaucoma with SD-OCT images: a systematic review and Meta-analysis
- Overexpression of TRPV1 activates autophagy in human lens epithelial cells under hyperosmotic stress through Ca2+-dependent AMPK/mTOR pathway
- Dry environment on the expression of lacrimal gland S100A9, Anxa1, and Clu in rats via proteomics
- Semaphorin 7A impairs barrier function in cultured human corneal epithelial cells in a manner dependent on nuclear factor-kappa B
- Novel MIP gene mutation causes autosomal-dominant congenital cataract
