Classification of congenital cataracts based on multidimensional phenotypes and its association with visual outcomes
Yuan Tan, Ying-Shi Zou, Ying-Lin Yu, Le-Yi Hu, Ting Zhang, Hui Chen, Ling Jin, Duo-Ru Lin,Yi-Zhi Liu, Hao-Tian Lin, Zhen-Zhen Liu
State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases, Guangzhou 510060, Guangdong Province,China
Abstract
● KEYWORDS: classification; congenital cataract;phenotype; visual acuity; cluster analysis
INTRODUCTION
Congenital cataracts affect 1-10 out of every 10 000 children globally[1]and are among the primary treatable causes of childhood blindness.The accurate diagnosis of congenital cataracts, along with appropriate treatment measures, contributes to preserving patients’ vision and enhancing their quality of daily life[2-5].
However, considerable phenotypic heterogeneity is a hallmark of congenital cataracts, which can coexist with various other ocular conditions, such as iris/choroid/lens/optic nerve coloboma, microcornea, microphthalmos, anterior segment dysgenesis, persistent fetal vasculature, optic atrophy, and retinal dystrophy[6-7].Congenital cataracts do not constitute a single category, which might underpin the ongoing debate regarding the selection of surgical procedures and postoperative refractive correction methods[8-10].Efforts to develop classification systems for congenital cataracts to better inform treatment are impeded by an overly specific focus on lens phenotypes[11-12].The existing classification systems do not indicate vision prognosis, which limits their utility in guiding the treatment of congenital cataracts[11-13].Multidimensional phenotyping is a state-of-the-art,comprehensive approach aimed at improving our understanding of disease mechanisms, diagnostic decision-making, and patient stratification and has the potential to provide clinicians with optimized therapeutic intervention strategies[10].Multidimensional phenotyping has already informed clinical treatments for ocular diseases, including amblyopia and uveitis[14-15].However, to our knowledge, no multidimensional phenotypic cluster analysis of patients with congenital cataracts has been performed.Therefore, this study aimed to develop an innovative and clinically meaningful classification system for multidimensional congenital cataract phenotypes based on cluster analysis, which may help indicate categories of visual prognoses and guide clinicians in tailored treatment choices.
SUBJECTS AND METHODS
Ethical ApprovalThis study was conducted according to the principles of the Declaration of Helsinki.Ethics approval was obtained from the Institutional Review Board of the local ethics committee (2013PRLL001).Written informed consent was obtained from the legal guardians of all patients.
Study PopulationThis retrospective study included patients diagnosed with congenital cataracts and undergoing surgical treatment, from January 5, 2005, to November 11, 2021.All patients were diagnosed with congenital cataracts at the age of 12mo or younger[16-17].Patients who did not undergo intraocular lens implantation, had a follow-up period of fewer than six months, or lacked follow-up visual acuity or fundus examination results were excluded.
Data CollectionAt the baseline and follow-up visits, all patients underwent comprehensive ophthalmic examinations by experienced pediatric ophthalmologists.Following the World Health Organization’s standard ophthalmic examination record scheme for preventable and treatable causes of childhood blindness[18], abnormalities detected in the patients’ eyes were classified according to anatomical locations, including the anterior segment (not including the lens), lens, retina (not including the macula or retinal vessels), macula, optic nerve,retinal vessels, and choroid.For noncooperative children,ophthalmic examinations were performed after sedation with orally or rectally administered 10% chloral hydrate.
The characteristics of the anterior segment and cataract morphology were identified based on the patients’ records of slit-lamp examination at diagnosis.The definition of abnormalities in the anatomical structure of the anterior segment included pupillary remnants and iris adhesions.Some eyes presented with microcornea [defined as a cornea with a diameter of less than 10 mm or a diameter two standard deviations (SDs) below the mean according to postconceptional age] or microphthalmos (defined as an axial length two SDs below the mean according to postconceptional age), which were also classified as anterior segment abnormalities[6].Based on the location of lens opacification after pupil dilation, cataract morphology was categorized into total lens opacification (total cataract), opacification confined to the center of the lens and not involving the anterior or posterior capsule (interior cataract), and opacification involving the anterior or posterior capsule (anterior or posterior cataract)[12].
Fundus abnormalities measured by fundus photography and optical coherence tomography (OCT) after inducing cycloplegia were collected from the patients’ medical records.The definition of morphological abnormalities of the retina included fundus tessellation and peripapillary atrophy[19].The definition of morphological abnormalities of the optic nerve included an abnormal vertical cup-to-disc ratio (≥0.5)[20],optic disc edema, optic disc coloboma, and morphological characteristics such as torted, tilted, and oval optic discs,optic disc pits, a double ring sign[21], and medullary fibers[22].The definition of morphological abnormalities of the macula included an altered foveal reflex[23], macular atrophy, and macular coloboma.Choroidal abnormalities referred to choroid coloboma[6].Finally, the definition of retinal artery and vein abnormalities included abnormally dilated, tortuous, twisted,or ectopic blood vessels[24]and bleeding[25].
Other important ophthalmic examinations included baseline axial length measurements and best-corrected visual acuity(BCVA) follow-up examinations.The baseline axial length measurements were performed before cataract surgery under topical anesthesia using A-scan ultrasonography (Aviso;Quantel Medical, France) or an IOL Master 500 instrument(Carl Zeiss Meditec AG, Germany).BCVA was considered the best-corrected vision measured in logMAR using ETDRS charts at 4 m.For noncooperative infants and children, Lea Symbols charts were used.At the last of multiple visual acuity test visits, BCVA was categorized into good vision (<0.7 logMAR)and poor vision (≥0.7 logMAR) based on established visual acuity criteria for diagnosing severe amblyopia in children[26].Information on demographics and family history of congenital cataracts was collected from the patients’ legal guardians using questionnaires.
Statistical AnalysisTo identify potential congenital cataract categories, hierarchical cluster analysis, an unsupervised algorithm clustering technique, was performed to identify homogeneous congenital cataract categories.The preliminary variables included in the analysis were ocular phenotypic parameters of congenital cataracts and demographic characteristics.
An unsupervised random forest was used to select the most relevant variables in the dataset.Variables associated with the greatest mean decrease in the Gini score were retained.Subsequently, an unsupervised hierarchical cluster analysis was performed using the “hclust” function in R software based on the dissimilarity matrix obtained from the “distmix”function from the kmed package (using Gower distances).Clusters were identified based on a dendrogram resulting from the hierarchical cluster analysis, which was cut using a higher relative inertia loss criterion.Notably, hierarchical clustering does not require any prior classification, thus facilitating a more detailed examination of heterogeneity within and between clusters.Prior to the random forest analysis, all missing data were inputted using the multiple imputation by chained equations algorithm.Distinct congenital cataract categories were named according to their respective cluster numbers.
A comparison of demographic and clinical characteristics between clusters was conducted using inter-eye correlationadjusted generalized estimating equations (GEE).In cases of limited sample sizes, which precluded the application of the GEE model, Fisher’s exact test was used.Data normality was evaluated through visual inspection of the histograms and the Kolmogorov-Smirnov test.GEE models were also used to describe the characteristics of the BCVA groups.The threshold of statistical significance was set at a two-sidedPvalue of<0.05.Odds ratios (OR) were estimated to measure the effect sizes of the comparisons.
All analyses were performed using RStudio with R software version 4.2.2.The packages used included dplyr, tidyverse,MICE, compareGroups, JLutils, kmed, and Clusters (https://www.r-project.org).The analyses were conducted from March 2, 2023 to October 15, 2023.
RESULTS
Cohort AttributesA total of 301 patients (527 eyes) were screened.Of those, 164 patients (54.49%; 299 eyes) were included in the analysis.The inclusion-exclusion process is shown in Figure 1.The general characteristics of the patients and their eyes are presented in Table 1.Among the study population, 115 (70.12%) patients were male, and 47 (28.66%)had a family history of congenital cataracts.The median age(interquartile range) at diagnosis was 3.0 (2.0-4.0)mo.A total of 144 patients (87.80%) were diagnosed with bilateral congenital cataracts, whereas 20 (12.20%) were diagnosed with unilateral congenital cataracts.The mean±SD baseline axial length was 20.06±2.06 mm (range: 15.40-25.10 mm).The median (interquartile range) age at cataract extraction was 6.0 (4.0-11.0)mo.Fifteen eyes presented with anterior segment abnormalities.Regarding cataract morphology, 124 eyes had total cataracts, 141 had interior cataracts, and 9 had posterior cataracts.Based on the results of any postoperative follow-up fundus photography or OCT examination, choroidal abnormalities were observed in 9 eyes, macular abnormalities were detected in 18 eyes, optic nerve abnormalities were found in 184 eyes, retinal abnormalities were detected in 200 eyes,and retinal vascular abnormalities were observed in 40 eyes(Table 1).

Figure 1 Flowchart of patient inclusion and exclusion.
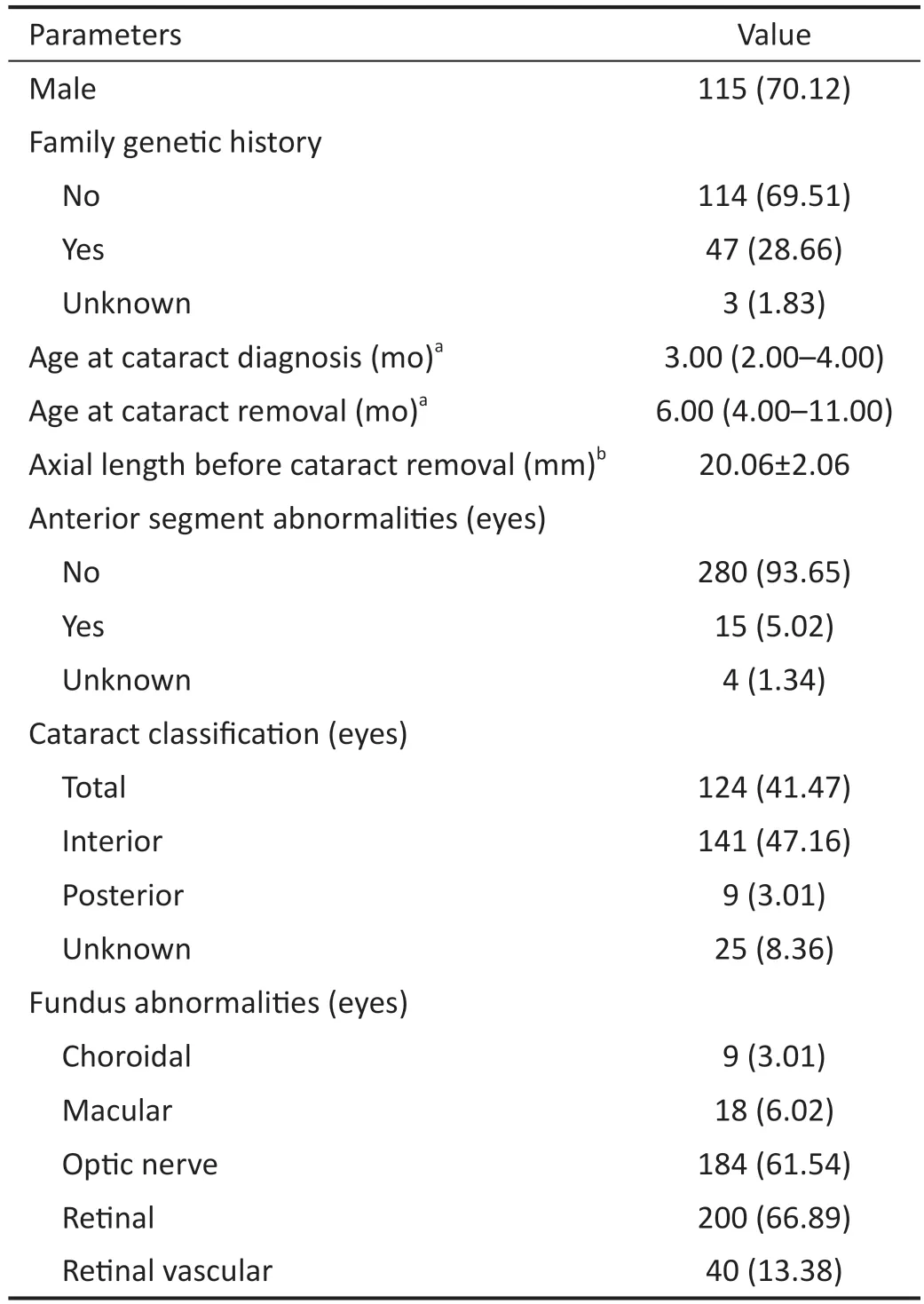
Table 1 Primary demographic and clinical characteristics of the study population n (%)
Congenital Cataract ClustersAccording to the hierarchical cluster analysis, the most suitable congenital cataract clustering consisted of two clusters (relative loss=0.79; Figure 2).Cluster 1 included 96 eyes, and Cluster 2 comprised 203 eyes.The sex distributions in Cluster 1 [73 males (76.04%)] and Cluster 2 [137 males (67.49%)] were similar (P>0.05).Clusters 1 and 2 also had similar proportions of reported family history of congenital cataracts (30.21%vs30.05%) and abnormal pregnancy history (34.38%vs35.47%; allP>0.05).Likewise,the ages at diagnosis (Cluster 1: 3.00mo; Cluster 2: 3.00mo)and the ages at cataract removal (Cluster 1: 5.00mo; Cluster 2:7.00mo) were comparable (allP>0.05; Table 2).

Figure 2 Dendrogram illustrating the two congenital cataract clusters The eyes are represented at the bottom of the dendrogram and grouped based on their level of similarity.Each node in the tree contains a group of similar data, and the nodes are grouped according to their similarities.
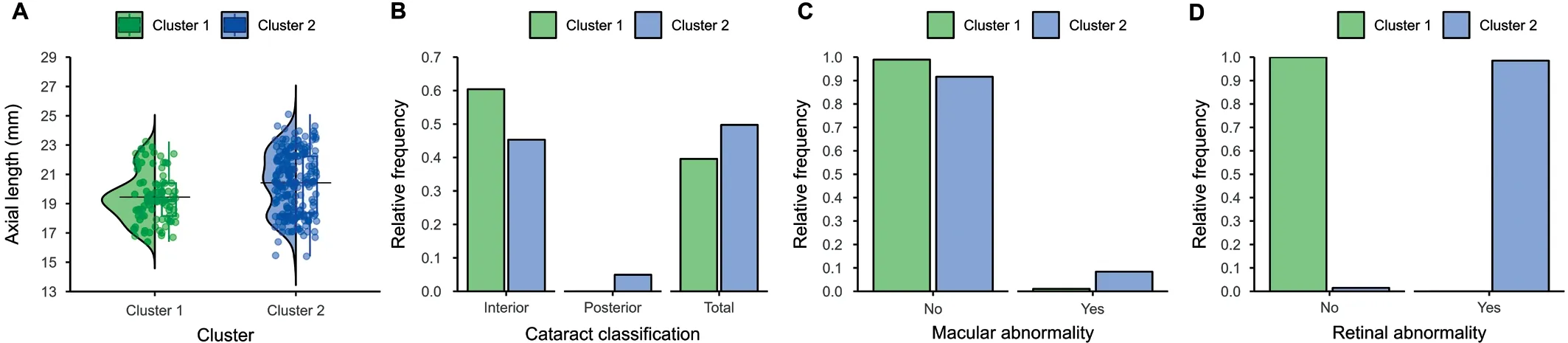
Figure 3 Clinical features of the two clusters.
A comparison of clinical characteristics (Table 2, Figure 3)showed that Cluster 1 had a significantly shorter baseline axial length than Cluster 2 (mean±SD, 19.44±1.68 mmvs20.42±2.10 mm;P=0.005).Moreover, Cluster 1 had significantly lower proportions of macular abnormalities [1 (1.04%)vs17 (8.37%);P=0.003], no retinal abnormalities [0vs200(98.52%);P<0.001], no posterior polar cataracts [0vs10(4.93%);P=0.034], and a significantly higher frequency of interior cataracts [58 (60.42%)vs92 (45.32%);P=0.028] than Cluster 2 (Table 2, Figure 3).
Visual Outcomes of the Patients in the Two ClustersThe overall mean±SD follow-up time was 6.10±2.67y, and Clusters 1 and 2 had similar mean follow-up times (mean±SD,6.41±2.78yvs6.84±2.82y;P=0.424).In both clusters, the longer the follow-up time, the higher the probability of achieving good vision [BCVA of <0.7 logMAR; OR (95%CI),1.13 (1.03-1.25);P=0.013].At the end of the follow-up period,69 of the 96 eyes (71.88%) in Cluster 1 and 116 of the 203 eyes(57.44%) in Cluster 2 achieved good vision.A GEE model that adjusted only for inter-eye associations showed that the OR of achieving good vision for Cluster 1 relative to Cluster 2 was 1.89 (95%CI, 1.11-3.23;P=0.020).After adjusting for age at vision measurement and inter-eye associations, the OR was 2.20 (95%CI, 1.25-3.81;P=0.006; Table 3).
DISCUSSION
Using a hierarchical clustering analysis, this large-sample study performed a binary classification (Clusters 1 and 2) of congenital cataracts based on multidimensional phenotypic characteristics.Cluster 2 had a greater baseline axial length and was more likely to present with posterior cataracts and macular and retinal abnormalities.Moreover, its BCVA at the last follow-up was inferior to that of Cluster 1.
The two congenital cataract clusters identified exhibit significant differences in multidimensional phenotypes.Notably, our classification extends beyond lens phenotypes to explain the considerable variability in visual prognoses.Indeed,our results preliminarily indicate that a group of patients with congenital cataracts is characterized by a greater baseline axial length, more frequent posterior cataracts and macular and retinal abnormalities, and a poorer visual prognosis (Cluster 2).Conversely, patients who do not exhibit these features usually have a better visual prognosis (Cluster 1).
By identifying two clusters of eyes with congenital cataracts exhibiting significantly different ocular characteristics and visual outcomes, we developed a clinically meaningful classification for congenital cataracts to help identify individuals with different prognoses and further provide individualized treatment regimens.In a clinical scenario, the following criteria can be used to determine whether a case belongs to Cluster 1 or Cluster 2: If there are posterior cataracts or retinal abnormalities, the case belongs to Cluster 2.If the axial length of a child under the age of one year is greater than 19.44 mm, or if there are macular abnormalities, it is highlylikely that the case belongs to Cluster 2.Otherwise, it belongs to Cluster 1.Considering the greater risk of a poor visual prognosis for patients belonging to Cluster 2, close monitoring and more aggressive early treatment may be recommended to achieve better outcomes[27].Moreover, emphasis should be placed on educating parents of children belonging to Cluster 2 about congenital cataracts and the role that they can play in managing the condition and educating their children about the importance of adherence to treatment.Improved visual outcomes were generally observed in eyes from cluster 1 following cataract surgery, which could suggest the feasibility of reduced postoperative follow-up for these eyes.

Table 2 Characteristics of the two clusters (164 patients, 299 eyes)
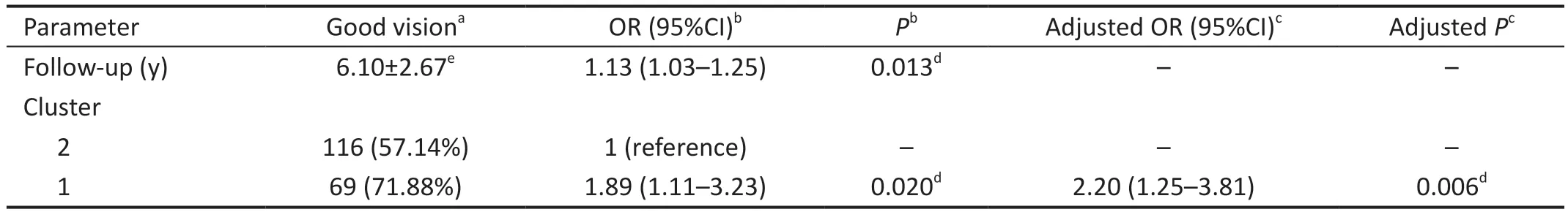
Table 3 Odds ratios of good vision
The axial length is considered an important predictor of pathological changes in the eye[28]and a significant ocular biometric feature that is relevant to congenital cataract management.The axial length of our patients ranged from 15.40 to 25.10 mm, which is very close to the range of 14.22 to 23.57 mm reported previously for patients with congenital cataracts within one year age[29].Previous research on factors related to the axial length in children with congenital cataracts has found no significant differences in axial length between Caucasian and African-American infants during the first year of life or a notable sex-based variation[30].In this study, Cluster 2, which had poorer vision than Cluster 1, had a greater axial length.One possible explanation is that a greater axial length is associated with greater light deprivation caused by cataracts, since more exposure to light slows the growth of the axial length[31].Another possible explanation is that a greater axial length reflects a poor innate condition of the eye,foreshadowing other pathological manifestations[32].Further research is needed to determine the relationship between the axial length and the visual prognosis of patients with congenital cataracts.Notably, in patients with total cataract, preoperative assessments of the fundus are not applicable, making the axial length the principal determinant.A comprehensive prospective study with a larger sample size is necessary to validate our observations in the future.
No prior studies have compared visual prognoses across categories of congenital cataracts.Our study suggests that posterior cataracts may be associated with a less favorable visual acuity prognosis.Clinically, cataracts involving the posterior capsule are associated with greater surgical difficulty and a higher risk of severe complications[33], which may further impact visual acuity outcomes[34-35].Therefore,ophthalmologists should exercise caution and prudence when devising surgical treatment plans for congenital cataracts that involve the posterior capsule.Furthermore, as such cataracts have been linked to genetic variations, such asGJA8[36], they may serve as diagnostic markers, guiding the discovery of genetic factors related to congenital cataracts.
This study sheds light on the underexplored area of fundus abnormalities in patients with congenital cataracts, who are often excluded from or overlooked in congenital cataract cohorts[37].Our findings indicate that more than 50% of patients present with fundus abnormalities, highlighting the importance of a thorough fundus assessment following cataract extraction to guide further treatment.Case report has linked genetic factors to the co-occurrence of congenital cataracts and retinal abnormalities[38].Potential explanations for the co-occurrence of congenital cataracts and fundus abnormalities may include genetic variations associated with conditions such as Alport syndrome or the presence of early-onset high myopia.Acquiring genetic data may enable us to definitively identify the underlying causes of the observed fundus phenotypes in congenital cataracts,thereby enhancing our understanding and potentially informing treatment strategies.Clinicians should pay more attention to fundus abnormalities in patients with congenital cataracts and their influence on long-term visual outcomes.
This study has several limitations.First, our data were derived from a single-center pediatric population in China; thus, the findings may not be broadly generalizable to other populations.Second, despite the study’s large sample size, its retrospective design entailed data omission, potentially affecting the accuracy of patient clustering.Third, genetic information on the patients, which could have provided more insights into phenotypic variations, was not available.
In summary, this study suggests the existence of two clusters of congenital cataracts according to multidimensional phenotypes.A greater axial length, posterior cataracts, macular abnormalities, and retinal abnormalities characterize a group of congenital cataracts with poorer visual prognoses.The other cluster, in contrast, generally exhibits more favorable visual outcomes.This categorization of congenital cataracts may help identify individuals with different visual prognoses and support clinicians in optimal treatment choices for better visual outcomes.Moreover, our findings pave the way for broader research, particularly foundational studies using new genomic technologies, to identify the potential prognostic factors of each phenotype, which can guide ophthalmologists in future treatment practices.
ACKNOWLEDGEMENTS
Foundations:Supported by the Municipal Government and School (Hospital) Joint Funding Programme of Guangzhou(No.2023A03J0174; No.2023A03J0188); the State Key Laboratories’ Youth Program of China (No.83000-32030003).
Conflicts of Interest:Tan Y,None;Zou YS,None;Yu YL,None;Hu LY,None;Zhang T,None;Chen H,None;Jin L,None;Lin DR,None;Liu YZ,None;Lin HT,None;Liu ZZ,None.
 International Journal of Ophthalmology2024年3期
International Journal of Ophthalmology2024年3期
- International Journal of Ophthalmology的其它文章
- Meibomian glands segmentation in infrared images with limited annotation
- Artificial intelligence for the detection of glaucoma with SD-OCT images: a systematic review and Meta-analysis
- Overexpression of TRPV1 activates autophagy in human lens epithelial cells under hyperosmotic stress through Ca2+-dependent AMPK/mTOR pathway
- Dry environment on the expression of lacrimal gland S100A9, Anxa1, and Clu in rats via proteomics
- Semaphorin 7A impairs barrier function in cultured human corneal epithelial cells in a manner dependent on nuclear factor-kappa B
- Novel MIP gene mutation causes autosomal-dominant congenital cataract
