Clinical and pathological characteristics and expression of related molecules in patients with airway disseminated lung adenocarcinoma
Wei Lun ,Shui Liu ,Ki Zhng ,Yin-Zi He
Abstract Objective: Lung adenocarcinoma exhibits diverse genetic and morphological backgrounds,in addition to considerable differences in clinical pathology and molecular biological characteristics.Among these,the phenomenon of spread through air space(STAS),a distinct mode of lung cancer infiltration,has rarely been reported.Therefore,this study aimed to explore the relationship between STAS tumor cells and the clinical and molecular characteristics of patients with lung adenocarcinoma,as well as their impact on prognosis.Methods:This study included 147 patients who were diagnosed with lung adenocarcinoma at the Inner Mongolia Autonomous Region Cancer Institute between January 2014 and December 2017.Surgical resection specimens were retrospectively analyzed.Using univariate and multivariate Cox analyses,we assessed the association between STAS and the clinicopathological features and molecular characteristics of patients with lung adenocarcinoma.Furthermore,we investigated the effects on patient prognosis.In addition,we developed a column-line plot prediction model and performed internal validation.Results:Patients with positive STAS had a significantly higher proportion of tumors with a diameter ≥2 cm,with infiltration around the pleura,blood vessels,and nerves,and a pathological stage >IIB than in STAS-negative patients(P <0.05).Cox multivariate survival analysis revealed that clinical stage,STAS status,tumor size,and visceral pleural invasion were independent prognostic factors influencing the 5-year progression-free survival in patients with lung adenocarcinoma.The predictive values and P values from the Hosmer-Lemeshow test were 0.8 and 0.2,respectively,indicating no statistical difference.Receiver operating characteristic curve analysis demonstrated areas under the curve of 0.884 and 0.872 for the training and validation groups,respectively.The nomogram model exhibited the best fit with a value of 192.09.Conclusions:Clinical stage,pleural invasion,vascular invasion,peripheral nerve invasion,tumor size,and necrosis are independent prognostic factors for patients with STAS-positive lung adenocarcinoma.The nomogram based on the clinical stage,pleural invasion,vascular invasion,peripheral nerve invasion,tumor size,and necrosis showed good accuracy,differentiation,and clinical practicality.
Keywords: Airway dissemination of tumor cells;Lung adenocarcinoma;Clinicopathological characteristics;Nomogram;Prognosis prediction model
1.Introduction
Lung cancer is one of the most common malignant tumors,and non–small cell lung cancer accounts for approximately 85%to 90%of cases.Non–small cell lung cancer can be categorized into squamous cell carcinoma,adenocarcinoma,and large cell carcinoma based on its pathological features.Among these,the incidence of lung adenocarcinoma has shown a gradual increase and has gained considerable attention in current research and treatment exploration.[1–3]Adenocarcinomas of the lung exhibit various genetic and morphological backgrounds,and considerable differences exist in their clinical pathology and molecular biological characteristics,resulting in substantial prognostic differences.[4–6]Spread through air space(STAS),a unique mode of lung cancer infiltration,is closely associated with pleural invasion,lymph node involvement,and vascular invasion.[7–10]However,studies analyzing the correlation between STAS and clinicopathological features,such as histological type and molecular subtyping,are currently lacking in China.This study aimed to explore the relationship between STAS and the clinicopathological and molecular features in patients with lung adenocarcinoma and their impact on prognosis,to provide novel evidence for precise treatment and adjustment of follow-up strategies for lung adenocarcinoma.
2.Materials and methods
2.1.General information
This study retrospectively reviewed surgical resection specimens of patients who had been diagnosed with lung adenocarcinoma at the Inner Mongolia Cancer Research Institute between January 2014 and December 2017.A total of 147 patients(83 men and 64 women)with complete clinical and follow-up data were included in this study.Patient data,including sex,age,smoking history,tumor location,clinical stage,surgical approach,pathological stage,and postoperative survival,were extracted and analyzed.The follow-up period was calculated from the date of surgery.Two experienced pathologists reevaluated the hematoxylin-eosin–stained tissue slides.The 2015 World Health Organization classification for lung adenocarcinoma was used as the morphologicalevaluation standard to reassess the histological subtypesof tumors.Based on the presence or absence of STAS,the patients were divided into STAS-positive and STAS-negative groups.
2.2.STAS diagnostic criteria
STAS positivity refers to the appearance of tumor cells as a microstructure of the nipple,small solid nests,or individual cells within the lung tissue distant from the main tumor focus.The collection and analysis of all data required approval from the institutional review board,and informed consent was obtained.
2.3.Molecular biology detection
Mutations in exons 18,19,20,and 21 of the epidermal growth factor receptor(EGFR)gene and exons 12 and 13 of the Kirsten rat sarcoma viral oncogene(KRAS)gene were detected using a mutation amplification blockade system.Anaplastic lymphoma kinase(ALK)gene fusion was detected using fluorescence in situ hybridization.Tissue DNA extraction for paraffin embedding and mutation detection of genes,such as EGFR and KRAS,was performed on a fluorescence quantification instrument according to the manufacturers’instructions(Xinnuo Meidi Gene Testing Technology Co,Ltd,Beijing,China).
2.4.Follow-up
Patients were followed up through telephone interviews,and information regarding postoperative treatments,follow-up examinations (including specific tests and intervals),and patient outcomes were recorded.
2.5.Statistical analysis
All data were analyzed using SPSS 22.0 software(IBM Corp,Armonk,NY).Categorical data are presented as counts(percentages).Rate comparisons were performed using the χ2test or Fisher exact probability test,and a P value <0.05 was considered statistically significant for intergroup differences.A multivariate Cox regression analysis was performed to investigate prognostic factors for lung adenocarcinoma.Independent hazard factors that had been identified through survival analysis were included in the construction of a nomogram model that assessed the impact on prognosis.The nomogram model is visualized using the“rms”package version 6.3-0 in R version 4.2.2.The discrimination of the model was assessed by evaluating the concordance index and the area under the receiver operating characteristic curve(AUC).A calibration curve was used to assess the goodness of fit of the model.
3.Results
3.1.General data
Our study included 147 patients with adenocarcinoma of the lung.Among them,45 were confirmed to be STAS positive by pathological evaluation.Of the 45 STAS-positive patients,44.4% were women,and 42.2%(19 of 45)were older than 65 years.The remaining 102 patients were identified as STAS negative,and among them,43.1%(44 of 102)were women and 49.0%(50 of 102)were older than 65 years.No significant differences in sex,age,or smoking history were observed between the 2 groups.However,within the STAS-positive group,the proportion of tumor diameter ≥2 cm,pleural invasion,vascular infiltration,and neural infiltration,as well as pathological staging above stage IIB,was significantly higher than in the STAS-negative group(P <0.05).Table 1 presents the results of the study.
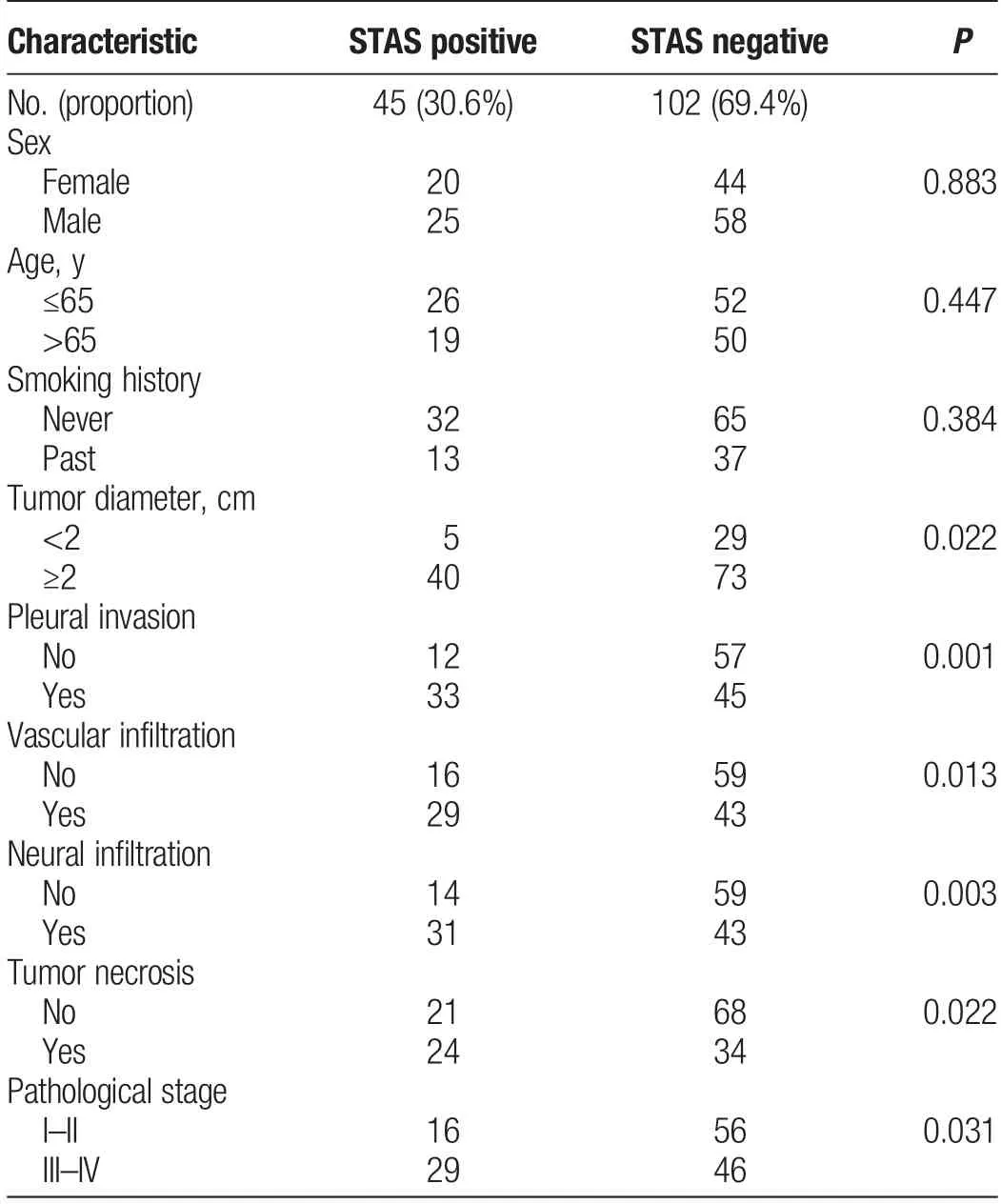
Table 1Association between STAS and clinical characteristics of patients with lung adenocarcinoma
3.2.Relationship between STAS and histological subtypes and molecular alterations in lung adenocarcinoma
STAS is closely associated with the histological subtypes and molecular alterations of lung adenocarcinoma.Further analysis revealed no significant differences(P >0.05)in the composition ratio of different histological types between the STAS-positive and STAS-negative groups.However,the positive mutation rates of EGFR and KRAS were significantly higher in the STAS-positive group than in the STAS-negative group(P <0.05),whereas no statistically significant differences in the positive rate of ALK gene rearrangements were observed(P >0.05).The results are summarized in Table 2.
3.3.Relationship between STAS and prognosis of adenocarcinoma of the lung
Univariate analysis indicated that progression-free survival (PFS) and overall survival(OS)of patients with lung adenocarcinoma differed significantly(P <0.05)based on STAS status,histological subtype,tumor size,pleural infiltration,vascular infiltration,neural infiltration,and clinical staging.Cox multivariate survival analysis revealed that clinical staging,STAS status,tumor size,and visceral pleural infiltration were independent prognostic factors influencing 5-year PFS in patients with lung adenocarcinoma.Clinical stage and tumor necrosis were independent prognostic factors that influenced the 5-year OS of patients with lung adenocarcinoma(Table 3).
3.4.Line graph of predicted median PFS in patients with STAS-positive lung adenocarcinoma
To gain a more intuitive understanding of the relationship between prognostic factors and survival time in patients with STAS-positivelung adenocarcinoma after radical surgery,a Cox proportional hazards model was used.Tumor diameter(in centimeters),TNM staging,visceral pleural invasion,and genetic mutations were considered indicators of the model.A prognostic nomogram was established using R4.2.2,which can be used to estimate the 1-,3-,and 5-year PFS rates of patients(Figure 1).The uppermost axis of the chart represents the scoring standards used to quantify factors within the nomogram.Scores ranged between 0 and 100,with higher scores indicating a poorer prognosis.Four potential prognostic risk factors that lie below this axis were included in this study.The lower axis of the nomogram corresponds to the sum of scores obtained for these variables.The total score ranged from 0 to 400,and as the total score increased,the PFS rate of patients showed a decreasing trend.The 1-,3-,and 5-year PFS rates were determined on the basis of the final total score for each patient.
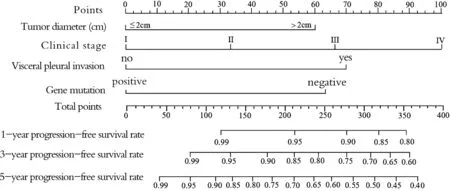
Figure 1.Nomogram for progression-free survival rates at 1,3,and 5 years after surgery.

Table 2Relationship between STAS and histological subtypes and molecular alterations in lung adenocarcinoma
3.5.Evaluation of the performance of the predictive model using line graphs
The predictive value of the nomogram in predicting the STAS status was evaluated using the Hosmer-Lemeshow test,which revealed no significant differences between the predicted and actual values (P values of 0.8 and 0.2,respectively).The discriminative ability of the predictive model was assessed using receiver operating characteristic curves,yielding an AUC of 0.884,sensitivity of 84.3%,and specificity of 80.7% in the training group and an AUC value of 0.872,sensitivity of 86.5%,and specificity of 90.1%in the validation group.The optimal fit for the nomogram model was 192.09,showing favorable predictive and diagnostic efficacy for prognosis among STAS-positive patients.
4.Discussion
STAS,a novel invasive growth pattern of lung adenocarcinoma,was officially described by the World Health Organization in 2015.[11,12]Its primary features include the formation of pathological microvascular clusters,individual tumor cells,and solid nests at the periphery of the primary lesion and within the pulmonary parenchymal airways.[13,14]However,STAS status can only be obtained through postoperative pathology,and guiding preoperative treatment planning is challenging.Recent studies have shown a significant correlation between STAS-positive status and the prognosis of patients with lung cancer.Specifically,patients with STAS-positive adenocarcinoma of the lung exhibit significantly decreased OS and PFS rates.Therefore,the preoperative assessment and prediction of STAS are crucial for determining patient outcomes.However,studies exploring the correlation between STAS and clinicopathological characteristics,including histological and molecular subtyping,in domestic settings are currently lacking.Analyzing the association between STAS status and postoperative molecular and clinicopathological characteristics will aid in formulating more rational diagnostic and treatment plans.Therefore,this study aimed to further analyze and investigate STAS status in patients with lung adenocarcinoma and its correlation with clinical factors.Consistent with previous findings,the results demonstrated that STAS positivity was present in 30.6%of patients with lung adenocarcinoma.STAS positivity rates ranging from 30.3%to 72%at different stages of lung adenocarcinoma have been reported.[15–17]Analysis of the correlations between STAS and clinical and pathological parameters revealed no significant associations with patient age,sex,or smoking history.However,a close relationship exists between STAS and factors indicating tumor invasion and metastasis,such as tumor diameter ≥2 cm,pleural,vascular,and neural invasion,and pathological stage >IIB.Notably,the rate of STAS positivity significantly increased in patients with clinical stage >IIB disease,indirectly suggesting the need for appropriate margin enlargement during surgery to reduce the risk of postoperative recurrence in patients with stage IIB and higher.
Genetic mutations are crucial factors that contribute to tumorigenesis and play vital roles in cellular signal transduction.They have significant regulatory effects on cell cycle processes such as growth,proliferation,differentiation,and apoptosis of tumor cells[18,19].Recently,molecular events such as EGFR and KRAS gene mutations and ALK gene rearrangements have emerged as the most important focus in lung cancer treatment and prognosis research[20,21].Therefore,this study aimed to analyze the relationship between histological subtypes,molecular mutations,and STAS positivity.The results demonstrated that the rates of EGFR and KRAS mutations in STAS-positive patients were significantly higher than those in STAS-negative patients,whereas no statistical difference was observed in ALK rearrangement positivity.The lack of statistical significance in the ALK rearrangement positivity may be attributed to the low incidence of ALK gene rearrangements in lung adenocarcinoma and the relatively limitedclinical samples used in this study[22,23].Moreover,the findings provide a new strategy for studying mechanisms underlying resistance to targeted therapies.Survival analysis revealed that STAS-positive patients had significantly shorter PFS and OS than STAS-negative patients,indicating that STAS can serve as an independent predictive factor for prognosis in patients with lung adenocarcinoma.

Table 3Cox multivariate survival analysis
A nomogram prediction model can represent complex computational formulae graphically in a fast,intuitive,and precise manner and has gained widespread attention and applications in medical research and clinical practice[24,25].By constructing a multiple regression model,the nomogram consisted of several parallel lines,including an integration line,hazard factor line,total score line,and percentage line segments.Each hazard factor corresponded to a specific score on the integration line,and the scores were added to obtain the total score.Finally,the event’s predictive probability is determined based on the total score[26,27].However,studies and predictive models focusing on the prognosis of patients with STAS-positive lung adenocarcinoma are currently scarce globally.Therefore,this study integrated four independent prognostic factors (clinical stage,tumor diameter,tumor infiltration,and genetic mutations)in STAS-positive patients to construct a nomogram for prognostic assessment.This nomogram can accurately predict an individual patient’s survival outcome and offers a more accurate and intuitive prediction than traditional single indicators,such as clinical stage alone.
In conclusion,this study identified the prognostic factors for STAS-positive patients and visualized the risk factors and predictive outcomes using a nomogram chart.This study provides a reference for the survival assessment,adjuvant therapy,and long-term postoperative management of patients with lung adenocarcinoma associated with airway spread.
Acknowledgments
Not applicable.
Financial support and sponsorship
Funded by the Health Science and Technology Program of Inner Mongolia Autonomous Region (no.202201061).Supported by the Joint Project of the Million Science and Technology Initiatives of Inner Mongolia Medical University(no.YKD2020KJBW(LH)057).
Conflicts of interest statement
The authors declare that they have no conflict of interest with regard to the content of this report.
Author contributions
W.L.is responsible for data collection and article writing.S.L.and K.Z.are responsible for data analysis and article revision.Y.-Z.H.is responsible for reviewing and submitting articles.
Data availability statement
The data in this article are obtained from clinical research and are true and reliable.
Ethical approval
This study and publication have received ethical approval.
 Oncology and Translational Medicine2024年1期
Oncology and Translational Medicine2024年1期
- Oncology and Translational Medicine的其它文章
- Wan-Yee Joseph Lau:the promoter of modernization and internationalization of Chinese surgery
- In vivo study of the effect of anlotinib on the stemness of the lenvatinib-resistant hepatocellular carcinoma cells and the underlying mechanisms
- Utilizing bioinformatics for integrated analysis of multiple genes in the diagnosis and pathogenesis of metastatic pheochromocytoma and paraganglioma
- Role of tumor necrosis factor alpha-induced protein 6(TNFAIP6)in tumors:a pan-cancer analysis
- Three novel rare TP53 fusion mutations in a patient with multiple primary cancers:a case report
