Biomaterial types, properties, medical applications, and other factors: a recent review
Reeya AGRAWAL, Anjan KUMAR, Mustafa K. A. MOHAMMED, Sangeeta SINGH
Review
Biomaterial types, properties, medical applications, and other factors: a recent review

1VLSI Research Centre, GLA University, 281406 Mathura, India2Radiological Techniques Department, Al-Mustaqbal University College, 51001 Hillah, Babylon, Iraq3Microelectronics & VLSI Lab, National Institute of Technology, Patna 800005, India
Biomaterial research has been going on for several years, and many companies are heavily investing in new product development. However, it is a contentious field of science. Biomaterial science is a field that combines materials science and medicine. The replacement or restoration of damaged tissues or organs enhances the patient’s quality of life. The deciding aspect is whether or not the body will accept a biomaterial. A biomaterial used for an implant must possess certain qualities to survive a long time. When a biomaterial is used for an implant, it must have specific properties to be long-lasting. A variety of materials are used in biomedical applications. They are widely used today and can be used individually or in combination. This review will aid researchers in the selection and assessment of biomaterials. Before using a biomaterial, its mechanical and physical properties should be considered. Recent biomaterials have a structure that closely resembles that of tissue. Anti-infective biomaterials and surfaces are being developed using advanced antifouling, bactericidal, and antibiofilm technologies. This review tries to cover critical features of biomaterials needed for tissue engineering, such as bioactivity, self-assembly, structural hierarchy, applications, heart valves, skin repair, bio-design, essential ideas in biomaterials, bioactive biomaterials, bioresorbable biomaterials, biomaterials in medical practice, biomedical function for design, biomaterial properties such as biocompatibility, heat response, non-toxicity, mechanical properties, physical properties, wear, and corrosion, as well as biomaterial properties such surfaces that are antibacterial, nanostructured materials, and biofilm disrupting compounds, are all being investigated. It is technically possible to stop the spread of implant infection.
Surface severe plastic deformation (SSPD); Hyaluronan (HA); Extracellular matrix (ECM); Polyvinylchloride (PVC); Tissue engineering (TE)
1 Introduction
A biomaterial is any matter surface or construct that interacts with biological systems. They can be derived from nature or synthesized in the lab using metallic components, polymers, ceramics, or composite materials. The study of biomaterials just like baby and biomechanics is a multi-disciplinary field that has established disciplines in medicine, chemistry, chemical engineering, mechanical engineering, biome dical engineering, and materials science (Mohammed et al., 2019, 2020; Ahmed et al., 2020; Al Rugaie et al., 2022; Alhujaily et al., 2022). Biomaterials are used in many ways in medical practice in medical implant methods to promote the healing of human tissues, regenerated human tissues, molecular probes, nanoparticle biosensors, and drug delivery systems. Examples of medical implants include but are not limited to heart valves, stent grafts, artificial joints, ligaments, tendons, hearing loss implants, and dental implants. Examples of regenerated human tissues include scaffold cells and bioactive molecules. Because biomaterials restore function while speeding recovery, today patients suffering from accidents or illnesses benefit significantly from using biomaterials (Saadatmand et al., 2021; Jasim et al., 2022; Vakil et al., 2022). Using bioengineered materials to repair wounded tissue or restore a compromised biological function in medical applications is expected. Historically, ancient Egyptians first employed biomaterials, which used sutures made of animal sinew to repair wounds. Among other medical, biological, physical, and chemical domains, tissue engineering and materials science have had a more significant recent impact on the contemporary field of biomaterials than any of these disciplines combined until recently (Mohammed et al., 2020; Mahmood et al., 2022; Noori et al., 2022). The use of non-living materials and living cells in biomaterials can be combined. Engineers can create molded or machined parts, coatings, and fabrics for biomedical devices and other consumer goods and industrial applications using these materials. Depending on the category, many medical devices may be included. They typically decay fast in the body after completing their intended function; some are even bioabsorbable (Ahmed and Mohammed, 2020; Ahmed et al., 2020; Govindan et al., 2022). Biomaterials can be divided into two categories: therapeutic materials and diagnostic materials. Fig. 1 shows different types of biomaterials.
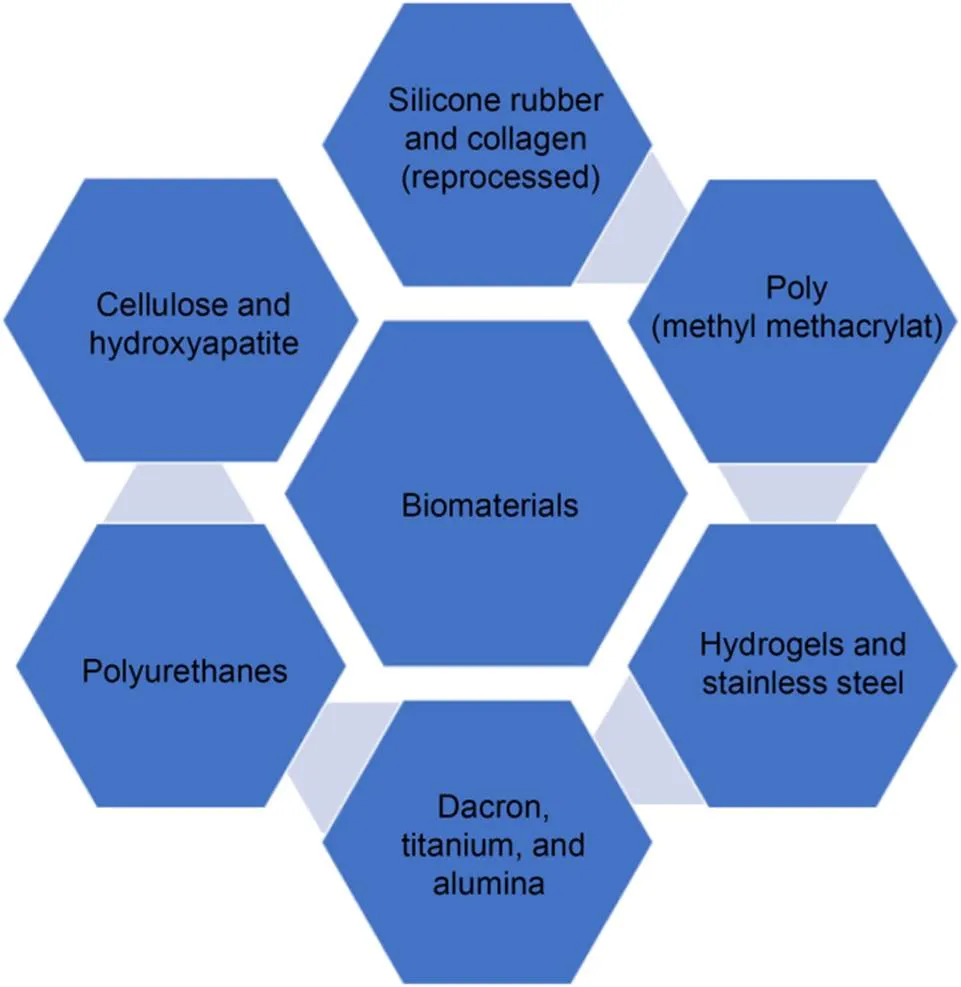
Fig. 1 Types of biomaterials
Therapeutic biomaterials are used in medical devices to treat or improve the function of tissues in the body. Biomaterials used in tissue repair or replacement replace lost or damaged tissue because of injury or disease. Biomaterials can be looked at with terms that are both biological and engineering. Trauma, disease, and degeneration can lead to surgery to fix things, which can happen if needed. People with broken bones usually need to have them replaced (Yilmaz et al., 2019; Motameni et al., 2021; Alshemary et al., 2022b). Everything that can be used instead of living things is called biomaterial. There are many different biomaterials, which are natural and artificial materials. The biological material is made by a living thing, like skin or an artery. Fig. 2 shows biomaterials required for tissue engineering of salient features.
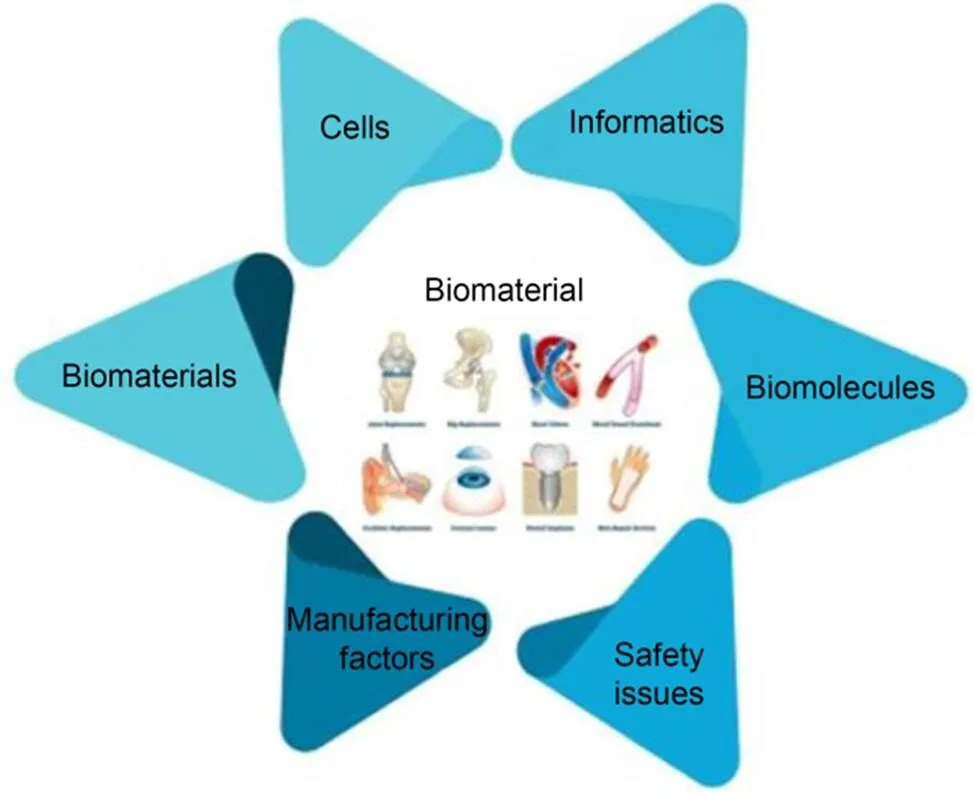
Fig. 2 Salient features of biomaterials required for tissue engineering
1.1 Bioactivity
Bioactivity is the ability of a biomaterial to make a person's body do something good for the material's job and efficiency (Alshemary et al., 2022a, 2022c). When materials are implanted in the body, the term osseoconductive conductor refers to materials that work as osseoconductive conductors. It can be found in bioactive glasses and ceramics. Most importantly, the materials used in implanted bone stimulate bone growth while also breaking down the body's fluids. When hydroxyapatite forms on the surface of biomaterials, it is common to find out how good they are for humans (Qin et al., 2021). Fig. 3 shows the different impacts of biomaterials.
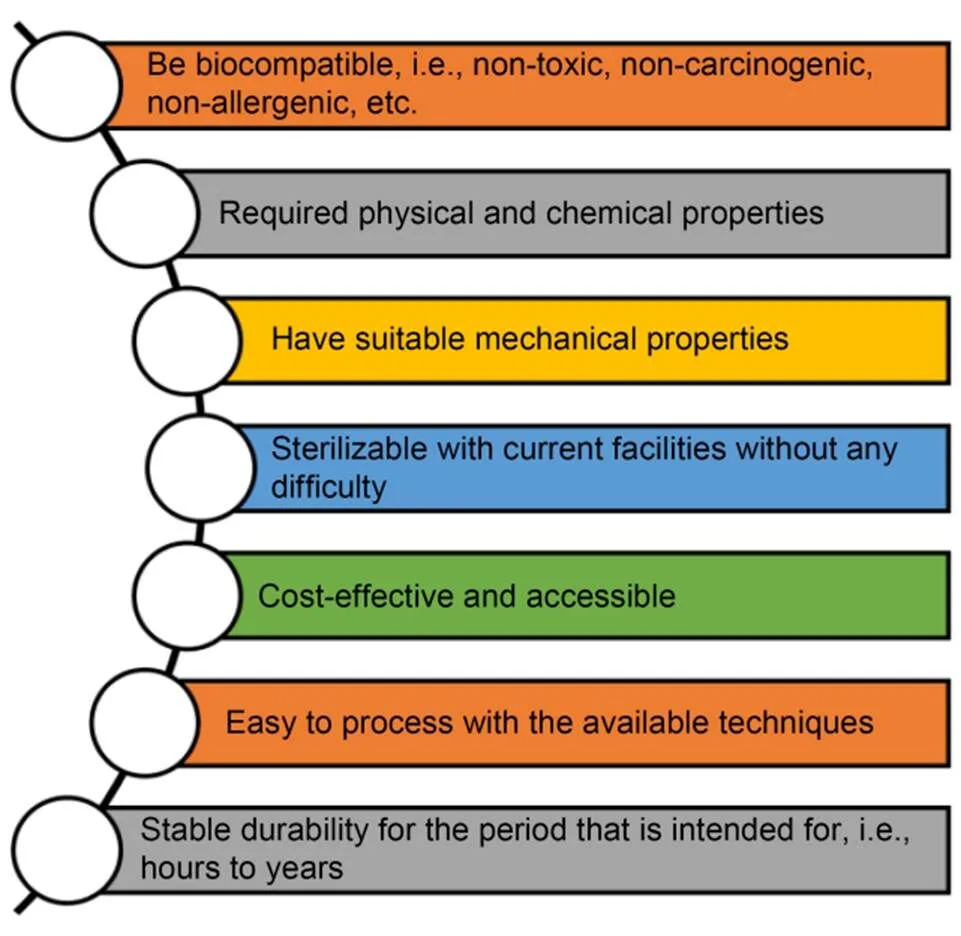
Fig. 3 Different impacts of biomaterials
1.2 Self assembly
In the scientific community, the phrase "self-assembly" is frequently used to describe the phenomenon in which particles spontaneously assemble without the assistance of an external force (Jin M et al., 2021). Massive clusters of these particles can combine to create one of seven crystal systems that are thermodynamically stable and structurally well-defined in metallurgy and mineralogy. A well-known fact is that molecular self-assembly is used to develop many biological structures, including the human body. Using natural microstructural features and designs to produce mechanically superior biomaterials has become increasingly popular (Książek, 2021). The use of self-assembly is becoming increasingly prevalent in chemical synthesis and nanotechnology. Applying these strategies can result in a diverse range of well-ordered structures. Molecular and liquid crystals are only a few instances of cutting-edge technology to realize the same. These approaches are distinct because they rely on self-organization to achieve their goals.
1.3 Applications
Before they may be used in therapeutic settings, biomaterials must demonstrate that they are biocompatible with the human body (Castro et al., 2021). Any biocompatibility difficulties must be resolved before the product is commercialized. As a result, novel pharmacological treatments are subjected to the same stringent standards as biomaterials. Therefore, all manufacturing organizations must ensure that all of their products are traceable to discover any more inappropriate materials that may have been added to the batch. Various biomaterials are employed in the following fields, as shown in Fig. 4.
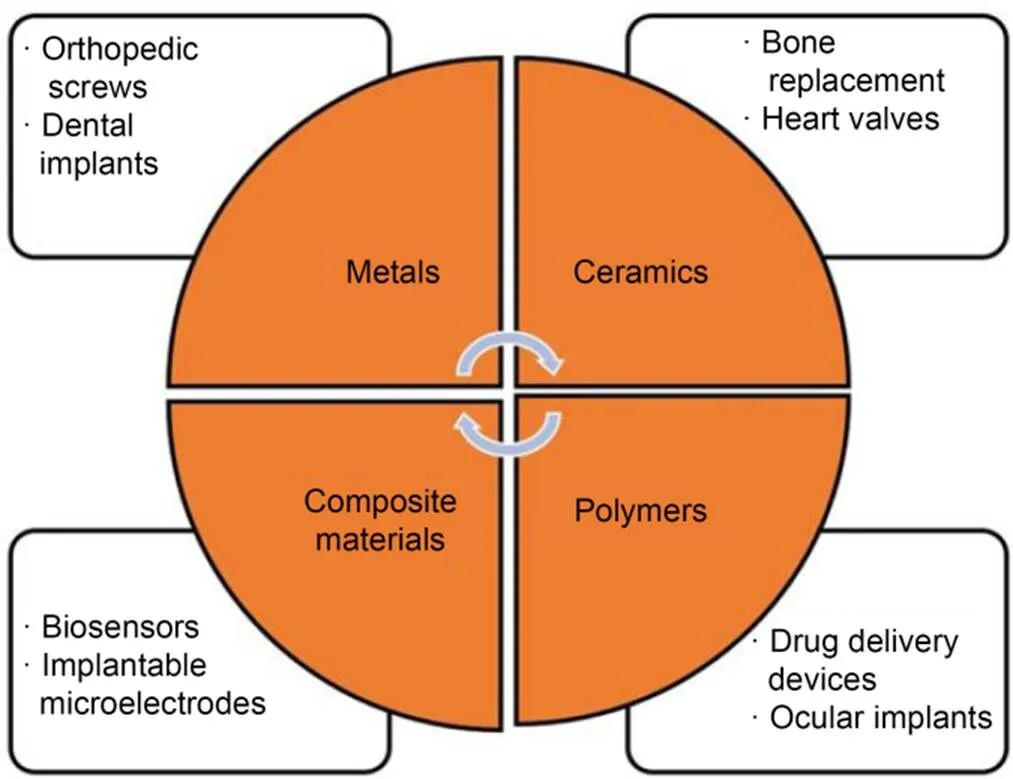
Fig. 4 Biomaterials' applications
1.3.1Heart valves
During a back-and-forth motion between two semi-circular discs, blood flow occurs while the other disc forms a seal to prevent blood from returning. DuPont used polyethylene terephthalate in the valve's manufacture because it was a commercial material for their pyrolytic carbon coating (Indurkar et al., 2021). The company employed a woven fabric called Dacron to hold the coating against the surrounding tissue. The valve can be absorbed into the body while allowing tissue growth around it using a mesh.
1.3.2Skin repair
It is possible to employ artificial tissue cells in extreme conditions where using a patient's cells might cause irreversible damage to the patient's body (Chen et al., 2021). Developing a structure on which cells can create and organize themselves is challenging. The scaffold must meet several characteristics, including biocompatibility, cell adhesion, mechanical strength, and biodegradability. Copolymers of lactic acid and glycolic acid are helpful as scaffolds.
1.3.3Bio-robots and 4D bio-printing
Bio-robots are an emerging field at the intersection of biomedical engineering, cybernetics, and robotics, to create innovative tools for merging the biological and mechanical worlds to improve communication, modify genetic information, and create machines that mimic biological processes. 4D bio-printing is a next-generation additive manufacturing-based fabrication process that has applications in creating both soft and stiff tissue structures and biomedical devices (Yu et al., 2021). Incorporating their biomedical expertise, the 4D bio-printing community has made remarkable achievements in producing innovative stimuli-responsive polymeric materials in recent years. Cartilage, bone, heart, and neurological tissue are all part of this category, as are the expensive biomedical equipment used to administer drugs. When external magnetic or electric fields are applied, a particular class of stimuli-responsive materials known as magneto/electro-responsive polymers (MERPs) is activated. Regulation of MERPs (multifunctional, dynamic, and fast reversible characteristics) is achieved at various length scales (Wu et al., 2020).
1.4 Bio-design
Unmet clinical requirements can only be addressed via innovation. Worldwide, medical devices and implants are in great demand, with India being the most prominent market. Medical technology innovation is needed today, more than ever, to address local problems and bring about lasting solutions (Yu et al., 2021). The recognition of the need to encourage and promote indigenous affordable medical innovations has taken steps to establish med-tech innovation bio-design initiatives and capacity for creative medical technology research prototyping, validation, and testing. The main goal is to develop innovative, low-cost medical implants and technology for the benefit of the whole nation. The bio-design goals are shown in Fig. 5.
Fig. 5 Bio-design objectives
1.5 Magnetorheological
Innovative materials include magnetorheological (MR) substances, which change their rheological and mechanical properties in reaction to an external magnetic field. Gels, liquids, and elastomers with solid consistency are viable for MR materials. Magnetorheological fluids (MRFs) and magnetorheological elastomers (MREs) are the most popular MR materials. At MREs, the magnetic particles are immobilized in a precisely controlled location within a polymeric matrix, whereas in MRFs, the particles float in a carrier fluid like silicone oil (Moreno et al., 2021). In an external magnetic field, their rheological and mechanical properties alter. MRFs are well-known for their severe stress amplification in a magnetic field, while MREs well-known for their modulus alterations (Bastola et al., 2020). However, MREs have a relatively short history as a counterpoint to MRFs. After initial studies on MREs were conducted, a novel class of MR materials called MR plastomers (MRPs) has the potential to create intelligent materials and structures distinct from MREs and MRFs. The highly mobile magnetic particles give MRPs plastic properties even at room temperature and have more substantial MR effects than MREs. MRPs are unsuitable for vibration isolators and absorbers due to their meager beginning moduli. But MRPs have the potential as a package for elastic, flexible, and conductive sensors and actuators like on/off switches. MREs experience dynamic changes in stiffness, natural frequency, and damping capacity in response to an applied magnetic field. Supplies classified as multi-role equipment (ME) can be used in various situations and are highly versatile. Changes in behavior, such as a shift in modulus or stiffness, are less prevalent (Dargahi et al., 2019).
Consequently, there has been an explosion of research investigating MRE behavior concerning attribute changes in the past few years. MEs alter their behavior by changing stiffness, natural frequency, damping capacity, storage/loss modulus, and complicated viscosity. Sandwich beams and vibration absorbers/isolators are only two examples of technical applications that benefit from ME's malleable stiffness and modulus.
1.6 Improved 3D-printed biomaterials for tissue engineering
Additive manufacturing (AM), often known as 3D printing, has made it possible to create patient-specific scaffolds, medical devices, and multiscale biomimetic structures with intricate cytoarchitecture and a hierarchy of function and structure (Arif MM et al., 2021; Arif ZU et al., 2022). The demand for 3D-printed replacement organs is rising with the number of people needing transplants. Many researchers in tissue engineering (TE) are currently focusing on 3D printing because of its potential to revolutionize the field. Both polylactide and polycaprolactone have attracted considerable interest as potential biomaterials for tissue regeneration due to their superior physicochemical and biocompatibility. Biodegradable polymers' interactions with in-vivo and in-vitro testing methodologies for future evaluation of degradation and biological properties are also highlighted (Mondal et al., 2016). Biomedical engineers will be of greater use to the clinical community if they bear the above in mind.
2 Biomaterial classifications, biomaterials in medical practice, and biomaterials designed for function
Artificial implants can produce a range of reactions in the tissue once implanted. Tissue reacts to the implant's surface and determines how the implant interacts with the surrounding tissues. The majority of the time, a biomaterial can be defined or classed in three ways based on the tissues' responses (Bhattacharyya et al., 2021; Momin et al., 2021; Saydé et al., 2021; Wang F et al., 2021; Hayajneh and Al-Oqla, 2022).
2.1 Biomaterial classifications
2.1.1Bioinert biomaterials
The materials that are not harmful to the body after they are put inside the body are stainless steel, titanium, alumina, zirconia, and ultra-high molecular weight polyethylene, among other things. Bioinert materials have minimal contact with the body's surrounding tissue after being transplanted into the body. A bioinert implant's biological usefulness depends on how well it can work with its tissue. A fibrous capsule can form around non-bioinert implants.
2.1.2Bioactive biomaterials
Bioactive implants and the body fluids surrounding them undergo an ion-exchange process, which creates an implant-surface layer composed of carbonate apatite (CHAp), which is physiologically active and has a mineral-equivalent carbonate composition. In terms of chemical composition and crystallographic structure, this layer is analogous to the mineral phase of bone in the human body.
2.1.3Bioresorbable biomaterials
As soon as they enter the body, bioresorbable materials dissolve (resorb) and are eventually replaced by new tissue, a process known as resorption (such as bone). Other bioresorbable compounds include polylactic–polyglycolic acid copolymers, tricalcium phosphate [Ca3(PO4)2], and polylactic–polyglycolic acid copolymers. Other typical materials employed in recent decades include calcium oxide, calcium carbonate, and gypsum.
2.2 Biomaterials in medical practice
Several applications for biomaterials in medicine, research, and bioengineering, including the following, are shown in Fig. 6. It is one of the main reasons biomaterials are used. They replace hard or soft tissues damaged or destroyed by the disease. Most people's tissues and structures last for a long time, but they can be damaged by fractures, infections, and cancer (Jin S et al., 2021).
Orthopedics: Biomaterials are used in many ways, but orthopedic implant devices are the most common. Osteoarthritis and rheumatoid arthritis change the structure of joints that can move freely, like the hip, knee, shoulder, ankle, and elbow.
Cardiovascular applications: Heart valves and arteries can have cardiovascular circulatory problems. Implants can be used to fix these problems.
Ophthalmics: The tissues in the eye can get sick from many different things, making it hard to see and eventually leading to blindness. Cataracts, for example, cause the lens to become cloudy. If users do not want this, users can get a synthetic (polymer) intraocular lens instead.
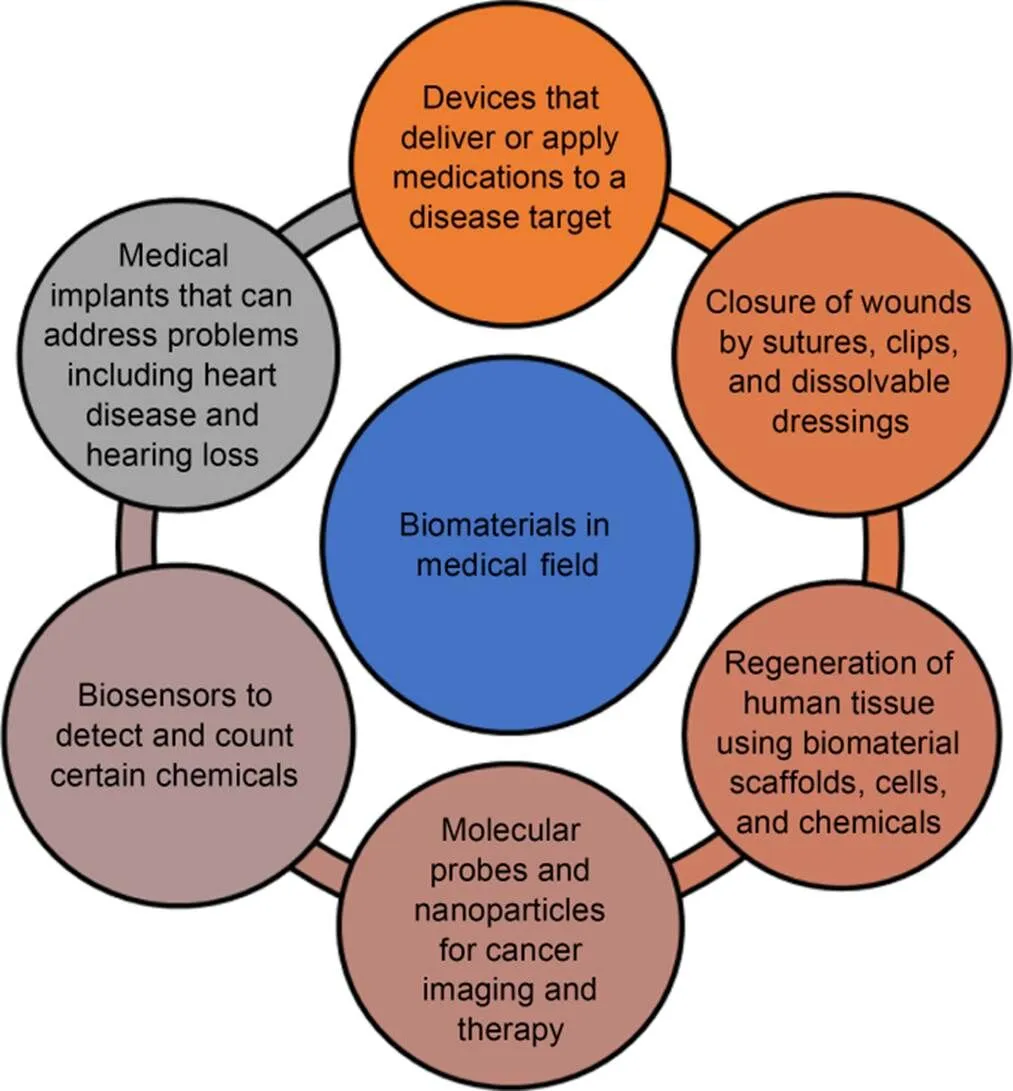
Fig. 6 Biomaterials in the medicine fields
Dental applications: People with bacteria in their mouths can quickly kill their teeth and the gums that hold them in place. People with dental caries, which are holes in their teeth caused by plaque's metabolic activity, can lose a lot of teeth.
Wound healing: There were first sutures, and they were used to close wounds. Implantable biomaterials can be traced back to this time. It is common for synthetic sutures to make polymers, but some metals can also make stitches.
2.3 Biomaterials designed for function
Bioengineers evaluate the performance of a biomaterial's properties, depending on how well it performs a particular activity and how it will be used (Bonferoni et al., 2021; Janarthanan and Noh, 2021; Liu et al., 2021; Yeung and Kelly, 2021). New skin and blood vessel growth are essential for wound healing to function correctly and quickly.
Intriguing fibrous protein systems: Stem cells are unspecialized; they can differentiate into any cell. Biomaterials can influence the behavior and fate of stem cells (Holmes et al., 2022). These materials must regulate biological activity, including stem cell production, by simulating the flexibility of different tissues.
Protecting the lungs with a chest bandage: Applying biomaterial sealants and patches to injured tissue makes it possible to rejuvenate and restore it. Brown algae-derived alginate could be utilized as a lung leak sealant and therapeutic patch to treat pneumonia and cystic fibrosis (Nace et al., 2021). According to the manufacturer, alginate is administered to the wound after freeze-dried and rehydrated with bodily fluids. Preliminary data reveal that this patch effectively treats lung leakage and repairs lung tissue in mice. A clever wound dressing can effectively treat diabetic ulcers in the long run. Many people wear wrist bandages with embedded sensors and actuators that come into direct contact with their flesh (Morita et al., 2021). It is anticipated to improve healing while simultaneously lowering the number of hospital visits and dressing changes patients require. Laser technology is used in laser-aided tissue healing and laser welding. Approximately one-quarter of persons who have had their colon segments re-joined experience wound site leaking in the weeks and months following surgery (Roach et al., 2021). The procedure uses laser-heated nanoscale materials, gold rods inserted in a matrix, and photothermal nanocomposites.
A burn bandage dissolves in the mouth: Burn sufferers experience excruciating pain when removing the application. The current clinically authorized dressings cause stress to newly produced tissue, making a recovery more difficult to achieve (Tao et al., 2022). Because of the controlled decomposition of the hydrogel into safe by-products, on-demand dressing removal and re-exposure of the wound will be achievable without mechanical debridement or cutting, making therapy more straightforward and less unpleasant.
Zinc alloy stents that disintegrate in body acid-metal stents are routinely utilized to maintain the patency of blood arteries. Long-term complications associated with metal stents include vessel re-narrowing, blood clots, and bleeding, among other complications (Kumar et al., 2022). A bioabsorbable zinc stent that gradually dissolves can reduce the hazards associated with long-term stent use. Early research on zinc stents that dissolve in the body has shown their potential.
3 SEM/TEM materials used for bio-applications
Three cutting-edge technologies, biomaterials, may have a bright future shortly (Hasan et al., 2021; Wang YM et al., 2021; Nickkholgh et al., 2022). Biomaterials injected into the body deliver medicines, genetic information, and proteins. Fig. 7 shows scanning electron microscope (SEM) images, transmission electron microscope (TEM) images, and modes of four nanocrystals.

Fig. 7 SEM images, TEM images, and modes of four nanocrystals (Li et al., 2018): (a) SEM images; (b) TEM images; (c) selected area electron diffraction (SAED) patterns for the four micro/nanocrystal structures product models derived from SAED and crystal parameters. Reprinted from (Li et al., 2018), Copyright 2018, with permission from American Chemical Society
Researchers are developing injectable biomaterials containing synthetic and naturally occurring components to treat cancer and heart disease. Biomaterials based on supramolecular chemistry have several benefits over conventional molecular ones when treating injury and illness (Ackun-Farmmer et al., 2021). Surrounding the development of supramolecular biomaterials that may imitate natural biological signaling or respond to physiological stimuli, scientists are examining how to make them. SEM can be used to demonstrate that the polymer blend is monophasic. The surface got more abrasive, and the number of holes produced increased (Fig. 8, NaOH).
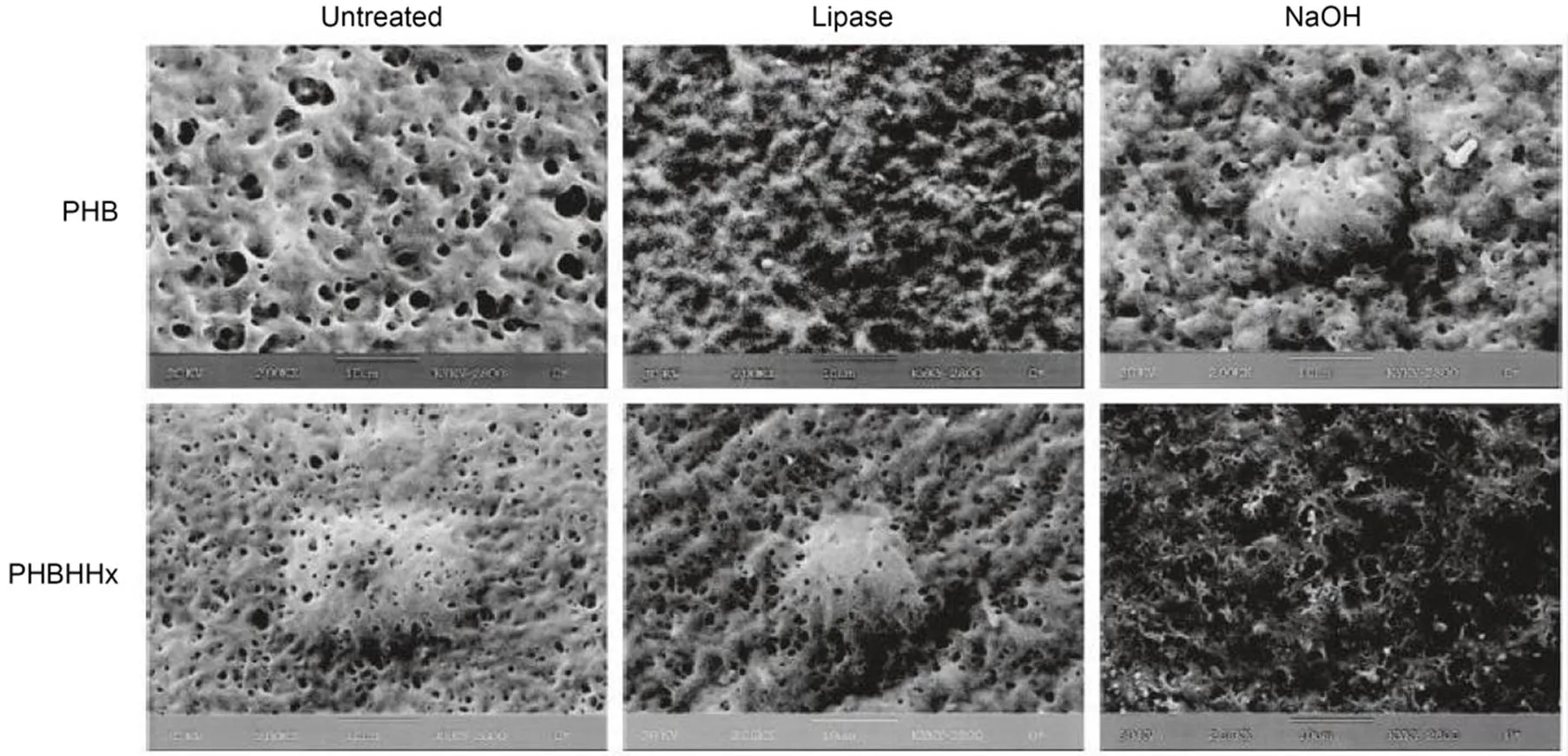
Fig. 8 SEM images of polyhydroxybutyrate (PHB) and poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) (PHBHHx) films before and after lipase and NaOH hydrolysis. Reprinted from (Zhao et al., 2002), Copyright 2002, with permission from Springer Nature
Numerous bacteria produce enzymes released outside their cell walls, such as extracellular polyhydroxybutyrate (PHB) depolymerase. The enzymes initially adhere to the surface of polymer materials via their C-terminal substrate-binding domains. They then use their N-terminal catalytic regions to degrade polymer chains (Adorinni et al., 2021; Sivasankarapillai et al., 2021). Enzymes can cleave specific segments of a polymer chain on its surface. The material disintegrates layer by layer (surface erosion, not inside the polymer matrix). SEM pictures of PLA and its composites after 14 d in compost and mud are shown in Fig. 9.
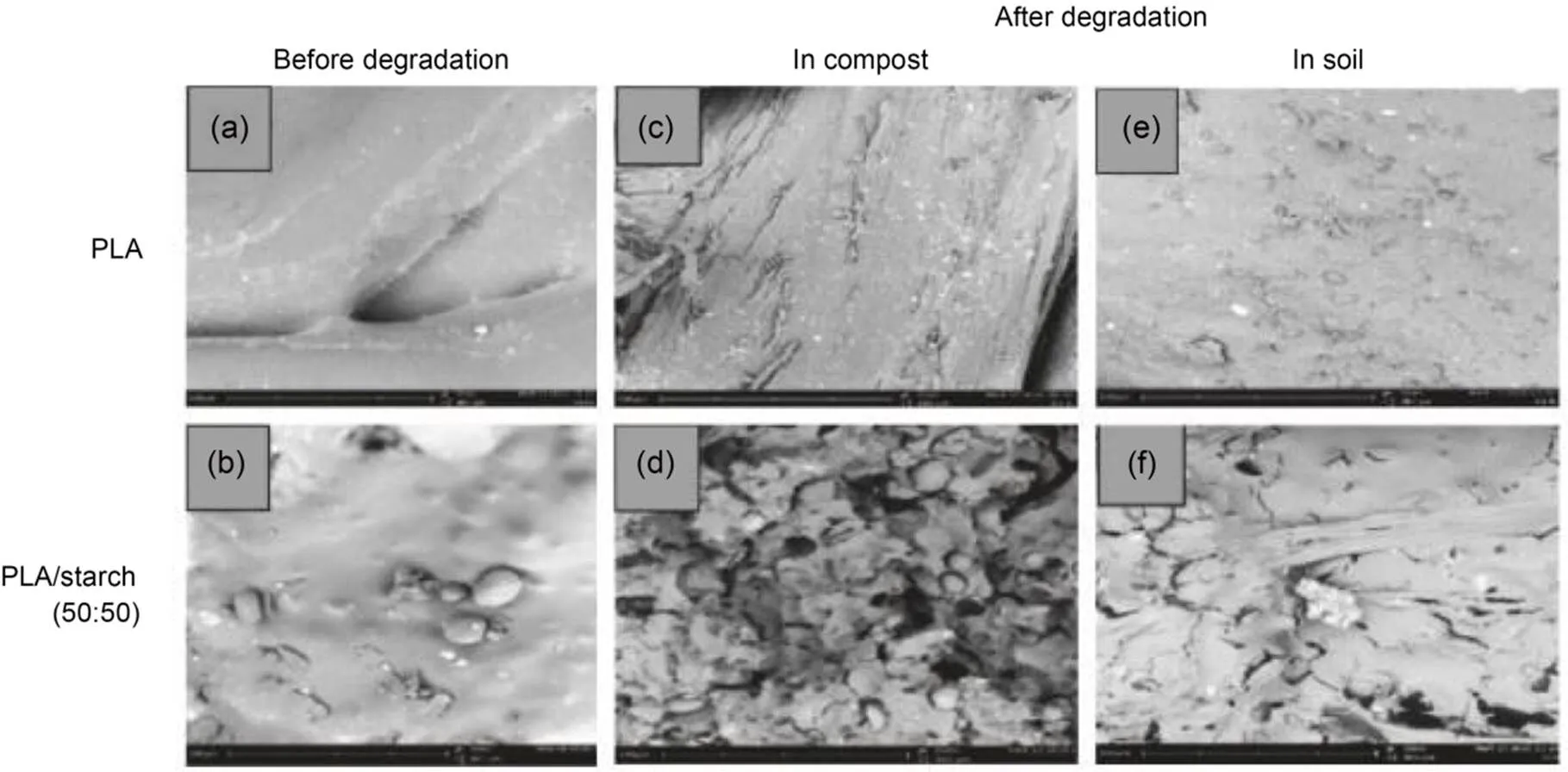
Fig. 9 PLA and PLA/starch samples before they were broken down (a and b), after they were broken down in compost (c and d), and in soil for 14 d (e and f). Reprinted from (Wilfred et al., 2018), Copyright 2018, with permission from Innovation Info
Polylactic acid (PLA) and its composites' surface morphology changed. All of the polymer materials examined exhibited biodegradation. Composites of PLA and starch (50:50) exhibited more alterations than pure PLA samples (Ma et al., 2021). While starch was removed from the surface of the PLA mixes, chemical hydrolysis was selected for the breakdown of pure PLA. Things degraded more rapidly in compost than in soil. Energy-dispersive X-ray spectroscopy (EDS) detector can ascertain whether any additives have a detrimental effect on the deterioration process. Different PLA/polybutylene adipate terephthalate (PBAT) blends containing the same PLA may degrade at varying speeds due to thickness variances and commercial additives added during production (Xiang et al., 2021).
The results indicate that the talc components may not behave as expected when water exposure, altering their degradation rate.
EDS analysis of some PLA/PBAT blend components revealed the presence of white inclusions (Mg and Si) in the polymer matrix, which was derived from a commercial addition known as hydrated magnesium silicate (talc), illustrated in Fig. 10. Phase separation occurs in low-miscibility mixes, whereas high-miscibility blends have a smooth surface. The molar mass and crystallinity of PLA and polyhydroxyalkanoates (PHAs) in polyester blends such as PHB and poly(hydroxybutyrate-valerate) (PHBV) affect their ability to operate well together (González et al., 2021). When the component molar masses are large, the combinations are not correct. In this case, one of the blend components has a lower molar mass, reducing the likelihood of phase separation.
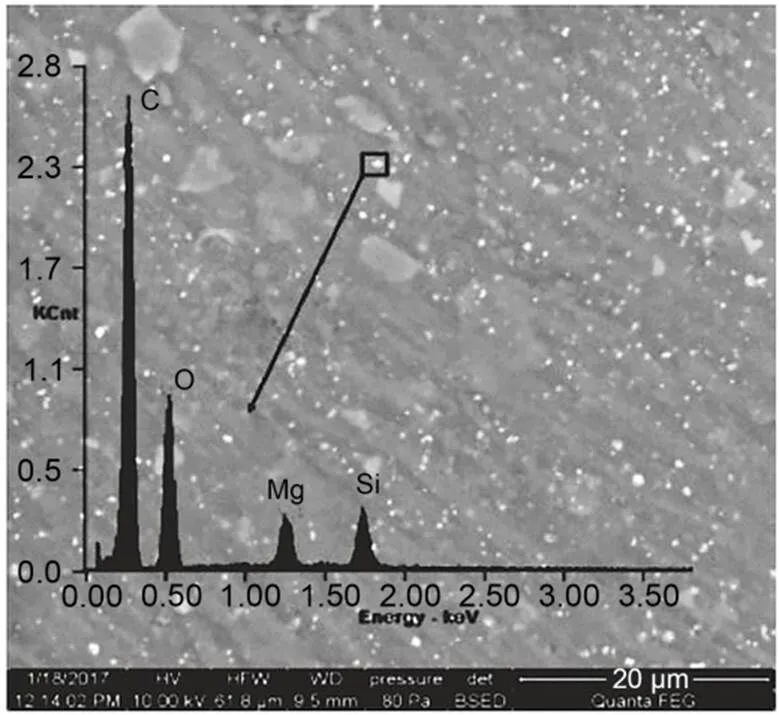
Fig. 10 SEM-EDS micrograph of PLA/PBAT. Reprinted from (Musioł et al., 2018), Copyright 2018, with permission from Elsevier
4 Biomaterials’ limitations and uses
Biomaterials look promising new treatment options in the early phases of research, but their full potential has not yet been realized. Biomaterials have various restrictions on interacting with the patient's bodily fluids (Crist et al., 2021; Dziadek et al., 2021; Zhang et al., 2021). Despite this, there are significant differences between synthetic materials and biological tissues, which suggests that biomaterials may not be as effective in healing wounded tissue as they could otherwise be. Biomaterials used in the heart must contract in sync with the heartbeat to avoid cardiac problems. Another biomaterial problem that influences heart health is insufficient oxygen reaching the heart. Because biomaterials have only been able to restore a fifth of the heart's original size, a significant heart attack causes more damage to the organ than it can heal with them. Researchers will develop novel biomaterials for treating additional illnesses after understanding the underlying reasons. It is necessary to create better methods to ensure new medicines repair damaged organs and tissues while not hurting patients during development. More details can be found in the electronic supplementary materials (ESM).
5 In vitro cytotoxicity concept in biomaterials
Biomaterials that work well with cells and tissues need to be designed and used in a way that works for them. One way to see how cells and tissues respond is to measure how toxic a substance is to a cell in the lab or how harmful it is to a cell in the real world (Nouri et al., 2021; Salihu et al., 2021). Cell toxicity is measured by how many cells die or cannot grow. It has been shown to meet these needs. There are two ester groups on each side of the carbon-carbon double bond in polypropylene fumarate (PPF), so there are two on each side. The unsubstituted carbon bond on the fumarate functional group makes PPF cross-link (Chu et al., 2021). Fumaric acid and propylene glycol are the products of hydrolysis, which breaks down an ester bond. Fig. 11 shows how the two methods of extracts were used. They were either added to a cell monolayer still growing 24 h after seeding or to cells floating in water (2nd mode).
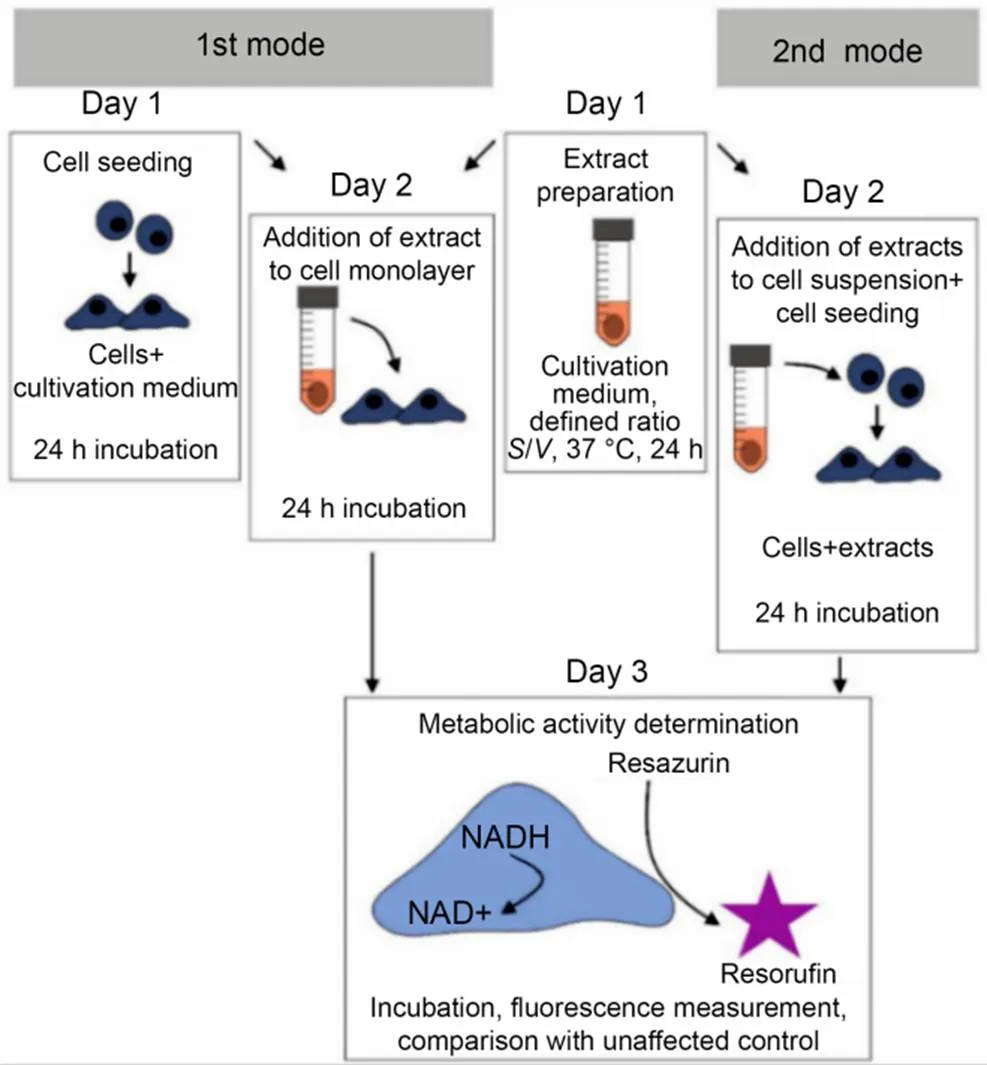
Fig. 11 Twenty-four hours after seeding, extracts were either added to a cell monolayer that was not yet fully grown (the first mode) or added to cells that had just been thrown around (2nd mode). Reprinted from (Jablonská et al., 2021), Copyright 2021, with permission from Nature Publishing Group
5.1 Evaluation of bioceramic toxicity
Different kinds of artificial implants made of metals, ceramics, polymers, and composites are safe for people to have in other body parts, depending on where they are put. Ceramics are the most common material used to repair hard tissue that has been damaged (Kumari and Chatterjee, 2021; Sadowska et al., 2021). Because different tests must be done depending on how long the material is in contact with the body to ensure it is biocompatible. Fig. 12 shows how bioceramic materials are tested in vitro and how they can be harmful.

Fig. 12 Toxicity of bioceramic materials in vitro and vivo. Reprinted from (Thrivikraman et al., 2014), Copyright 2014, with permission from The Royal Society of Chemistry. RBC: red blood cell
Biocompatibility is very important for any material used in the body, so regulatory bodies have set up tests to ensure that materials are safe for people. In the long run, if a biomaterial that has not been adequately tested is implanted, it may cause a long-term biological reaction (Ma et al., 2022). The biomaterials used in an implant must be checked for risks to last a long time in the body. Table 1 describes the classification of biocompatible polymer optical fiber.
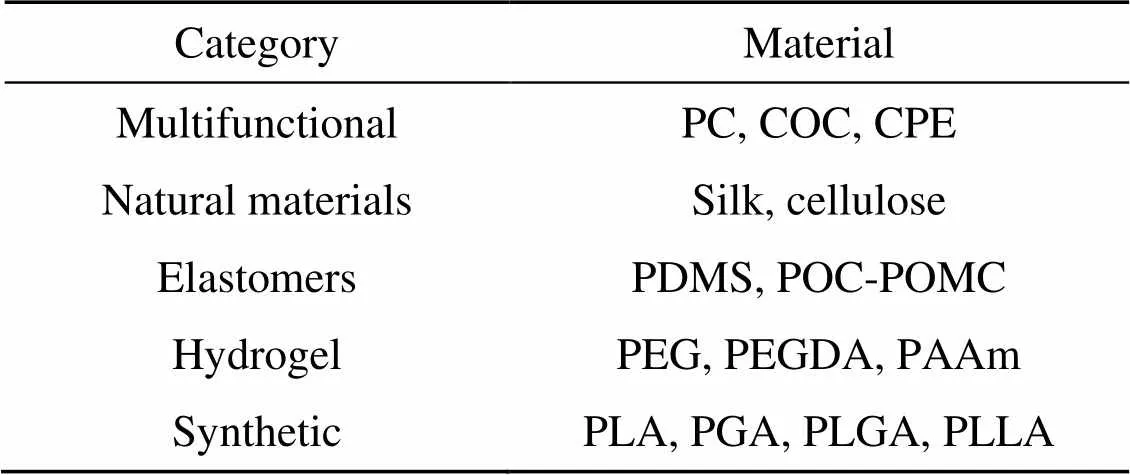
Table 1 Classification of biocompatible polymer optical fiber
PC: polycarbonate; COC: cyclic olefin copolymer; CPE: conductive polyethylene; PDMS: polydimethylsiloxane; POC-POMC: poly (octamethylene citrate)-poly (octamethylene maleate citrate); PEG: poly (ethylene glycol); PEGDA: poly (ethylene glycol) diacrylate; PAAm: polyacrylamide; PGA: poly (glycolic acid); PLGA: poly (lactic-co-glycolic acid); PLLA: poly (L-lactic acid)
5.1.1Cytotoxicity
Plant a cell or put the cell in a solution from extracting the material to determine how a specific cell type reacts to a particular material. Choosing the right cell lines, controls, biochemical assay type, and culture time all play a significant role in whether a material can be used with other things. On cell lines from mice, humans (and other animals), the toxic residues from three polymeric biomaterials did not make any difference in how sensitive the cells were to them. More evaluation methods and specific cell lines should be used (Park SY et al., 2022; Suvindran et al., 2022; Szczuka et al., 2022). Tissue osteoblast and keratinocyte cell lines can also be used to check the cell compatibility of orthopedic implant materials. Wound dressing materials can also be tested for their cytotoxicity, which can be done with different types of cells. For a new biomaterial to move from the lab to the clinic, it must undergo rigorous tests, as shown in Fig. 13.
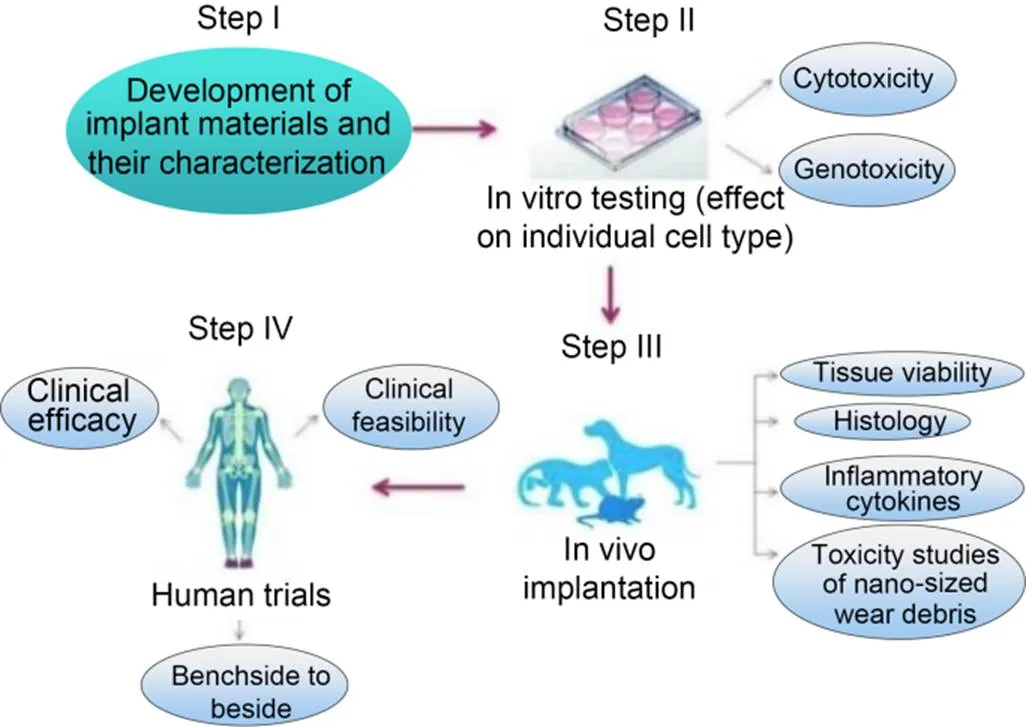
Fig. 13 Formation steps of biomaterials from bench side to bedside. Reprinted from (Thrivikraman et al., 2014), Copyright 2014, with permission from The Royal Society of Chemistry
5.1.2Genotoxicity
Implant materials and particles that come with them are a big part of figuring out how safe they are for people to have in their bodies for a long time. They can get into the cytoplasm of a eukaryotic cell because they are tiny (Park KM et al., 2022). In one case, zirconium oxide particles that came out of bone cement when worn down are an exception to this rule. It has been said that when these nanoparticles get inside the body, they can make reactive oxygen species (ROS) and make the body more oxidatively stressed, but this is not true. It can also cause other signaling pathways to be activated, leading to the aberration or double-strand breaks of chromosomes in the nucleus, affecting cell division and growth. Different gene regulatory proteins are turned on in other cells when a virus damages a cell. It can happen when oncogenes are turned on or tumor suppressor genes do not work (Abreu et al., 2022). A tumor can start when these things happen. If biomaterials can cause cancer, relevant in vitro methods should be used to see if this is the case. Tiny particles of cadmium, cobalt, cobalt-chromium alloy, and nickel have been found to cause cancer in people who use orthopedic implants. These metals are used in many types of orthopedic implants. Biomaterial implants' toxicity and long-term stability can be tested more effectively and in biologically relevant ways. Even though comparing the biocompatibility results of new material in vitro and in vivo can show its safety, its true fate will only be known when used in people (Liu et al., 2022). Fig. 14 shows possible ways that nano particles and micron particles enter the body and cause genotoxicity.

Fig. 14 Genotoxicity representation. Reprinted from (do Nascimento et al., 2017), Copyright 2017, with permission from Springer Nature
6 Conclusions and future directions
Biotechnology could improve people's health and quality of life if used correctly. This procedure could provide compounds of extensive utility. Utilization possibilities are vast due to the molecular and atomic combinations. Biomaterials with this technique may be used in various fields, including medicine, dentistry, veterinary care, and even mechanical engineering. Fabricating biosensors, drug delivery systems, and scaffolds are a few of this technique's possible uses. The ability to accurately adjust stoichiometry and particle size during production is possible. From their early days, when they were used by surgeons performing amazing surgeries with the aid of engineers, the areas of biology and bioengineering have come a long way. Just as a wide range of materials can be utilized to make biomaterials, so can their medical applications. Biomaterials can be used to create replacement heart valves and other organs for patients needing repair. Use it on items that can move, like the hydroxyapatite-coated hip implant from 20 years ago. The medical device industry heavily uses biomaterials because of their pivotal role in the healthcare system. Products for hard and soft tissues, biomedical devices, pharmaceuticals, test kits, and more can all be found in the medical sector. However, there is still a long way to go. Biomaterials used in modern medical therapies, such as those for preventing and treating major hereditary diseases, may vary in response to new medical needs. We can expect a surge in the popularity of metal, ceramic, and polymer implants for medical use. Researchers in molecular biology, biochemistry, genetics, and physics are merging their efforts to develop more effective biomaterials for specific applications.
Biocompatibility, bioactivity or surface reactivity, biodegradability, stabilizability, good mechanical and physical features, manufacturability, low weight, affordability, and accessibility are all traits to look for in a material. Molecular and genetic approaches to disease research have led to exciting new developments in diagnosis, treatment, and prevention. A biomaterial is any synthetic material that could be used in medicine. For instance, a biomaterial heart valve replacement could be passive or active.
6.1 Drug encapsulation and release gels and hydrogels
Much interdisciplinary research has been conducted on biomaterials used in the administration of drugs. The chemical and biological characteristics restricting medicine delivery are still a mystery, so kinetically controlling the release of medicines remains a challenging problem (Xu et al., 2021). Over 50 years of encapsulation and release materials have been developed to release bioactive pharmaceuticals over a long period and (in the best case scenario) begin interactions with the host to control how much medication is taken from the capsule. While conventional chemicals like silver nanoparticles or silver nitrate have demonstrated biocidal activity against human pathogens (both gram-negative and positive) and bacteria resistant to quaternary amine, lignin-derived nanoparticles have shown biocidal activity at significantly lower silver concentrations, resulting in an inactive biodegradable particle after release, which has less of an effect on the environment (Kalirajan et al., 2021). An immobilized (or "spatially restricted") catalyst is contained in lignin colloidal particles. The research will emphasize the design, characterization, and potential uses of nanostructured lignin hydrogels. No investigations into drug release or biocompatibility have been carried out despite the idea that carriers play a role in medication delivery. During the precipitation step, the researchers added the hydrophobic insecticide Avermectine to the particles and examined the microparticles for drug release and ultraviolet (UV) protection, among other properties (Wan et al., 2021).
6.2 Tissue engineering scaffolds
An interdisciplinary approach is taken while looking into the various biomaterials utilized in tissue engineering and regenerative medicine. Scaffolds can be used for multiple purposes, some of which are at odds with one another (Rashid et al., 2021). If harmful degradation products are to be avoided, scaffolds for bone regeneration must be disintegrated and replaced with natural bone. Allogeneic bone transplants are the second most common source of replacement bones, behind the chin, retro-molar area, iliac crest, and trabecular bone (available from bone banks). In addition to allogeneic and xenogeneic transplants, there are also xenogeneic and alloplastic transplants (which use materials like hydroxyapatite or tricalcium phosphate). Patients can now receive treatments specifically suited to their needs because of advancements in stem cell technology. A variety of factors influence biocompatibility (Khalid et al., 2021). These include long-term stability against physiological media, mechanical strength depending on the application's mechanical strength, corrosion resistance, residual-free metabolism, and adequate technical capability for a given application. Comprehending the adhesion mechanisms on cell–biomaterial surfaces and interfaces is the first step in understanding cell–biomaterial interactions. Different surface polarities, surface roughness, and topography influence how hydrophilic and hydrophobic surfaces interact. In this method, polymers are made with well-defined porosity structures, allowing cells to grow into them as they are built (Bello et al., 2020). It is essential to tailor the properties of polymers for each specific application. Surface polarity and topography must be adapted to the shape of cells to promote cell adhesion, proliferation, and growth. Polyurethane (PU) has also been the topic of numerous studies regarding its applications in tissue engineering (Hussain et al., 2021). Because of the extensive range of polyol and isocyanate components for PU synthesis available, it is feasible to modify the internal structure and morphology of PU materials to appear and feel like actual bone while also encouraging tissue ingrowth stiff or flexible osteogenic differentiation in bone tissue stimulated by the addition of iron oxide nanoparticles having super magnetic characteristics (Chao et al., 2021). They implant human bone marrow stem cells (hBMSCs) into PU scaffolds with better osteogenesis than the control PU scaffolds. Lignin-based polyurethanes (lignin-PU) are projected to rise in importance as preferred study materials because of their potential as biodegradable tissue engineering scaffolds and drug encapsulation materials. The mechanical stability of agarose/lignin composites has been improved by partially using lignin to replace polysaccharide components (Rahmati et al., 2020).
Author contributions
Reeya AGRAWAL: conceptualization, methodology, data curation, writing-original draft; Anjan KUMAR: conceptualization, review, and editing; Sangeeta SINGH: supervision and validation; Mustafa K. A. MOHAMMED: supervision.
Conflict of interest
Reeya AGRAWAL, Anjan KUMAR, Mustafa K. A. MOHAMMED, and Sangeeta SINGH declare that they have no conflict of interest.
Abreu H, Canciani E, Raineri D, et al., 2022. Extracellular vesicles in musculoskeletal regeneration: modulating the therapy of the future., 11(1):43. https://doi.org/10.3390/cells11010043
Ackun-Farmmer MA, Overby CT, Haws BE, et al., 2021. Biomaterials for orthopedic diagnostics and theranostics., 19:100308. https://doi.org/10.1016/j.cobme.2021.100308
Adorinni S, Cringoli MC, Perathoner S, et al., 2021. Green approaches to carbon nanostructure-based biomaterials., 11(6):2490. https://doi.org/10.3390/APP11062490
Ahmed DS, Mohammed MKA, 2020. Studying the bactericidal ability and biocompatibility of gold and gold oxide nano particles decorating on multi-wall carbon nanotubes., 74(11):4033-4046. https://doi.org/10.1007/s11696-020-01223-0
Ahmed DS, Mohammed MKA, Mohammad MR, 2020. Sol–gel synthesis of Ag-doped titania-coated carbon nanotubes and study their biomedical applications., 74(1):197-208. https://doi.org/10.1007/s11696-019-00869-9
Al Rugaie O, Jabir MS, Mohammed MKA, et al., 2022. Modification of SWCNTs with hybrid materials ZnO–Ag and ZnO–Au for enhancing bactericidal activity of phagocytic cells againstthrough NOX2pathway., 12(1):17203. https://doi.org/10.1038/S41598-022-22193-1
Alhujaily M, Albukhaty S, Yusuf M, et al., 2022. Recent advances in plant-mediated zinc oxide nanoparticles with their significant biomedical properties., 9(10):541. https://doi.org/10.3390/bioengineering9100541
Alshemary AZ, Hussain R, Dalgic AD, et al., 2022a. Bactericidal and in vitro osteogenic activity of nano sized cobalt-doped silicate hydroxyapatite., 48(19):28231-28239. https://doi.org/10.1016/j.ceramint.2022.06.128
Alshemary AZ, Motameni A, Evis Z, 2022b. Biomedical applications of metal oxide–carbon composites.: Chaudhry MA, Hussain R, Butt FK (Eds.), Metal Oxide-Carbon Hybrid Materials. Elsevier, Amsterdam, the Netherlands, p.371-405. https://doi.org/10.1016/B978-0-12-822694-0.00004-1
Alshemary AZ, Muhammed Y, Salman NA, et al., 2022c. In vitro degradation and bioactivity of antibacterial chromium doped β-tricalcium phosphate bioceramics., 66(3):347-353.
Arif MM, Khan SM, Gull N, et al., 2021. Polymer-based biomaterials for chronic wound management: promises and challenges., 598:120270. https://doi.org/10.1016/j.ijpharm.2021.120270
Arif ZU, Khalid MY, Zolfagharian A, et al., 2022. 4D bioprinting of smart polymers for biomedical applications: recent progress, challenges, and future perspectives., 179:105374. https://doi.org/10.1016/j.reactfunctpolym.2022.105374
Bastola AK, Paudel M, Li L, et al., 2020. Recent progress of magnetorheological elastomers: a review., 29(12):123002. https://doi.org/10.1088/1361-665X/abbc77
Bello AB, Kim D, Kim D, et al., 2020. Engineering and functionalization of gelatin biomaterials: from cell culture to medical applications., 26(2):164-180. https://doi.org/10.1089/ten.teb.2019.0256
Bhattacharyya A, Janarthanan G, Noh I, 2021. Nano-biomaterials for designing functional bioinks towards complex tissue and organ regeneration in 3D bioprinting., 37:101639. https://doi.org/10.1016/j.addma.2020.101639
Bonferoni MC, Caramella C, Catenacci L, et al., 2021. Biomaterials for soft tissue repair and regeneration: a focus on Italian research in the field., 13(9):1341. https://doi.org/10.3390/pharmaceutics13091341
Castro D, Jaeger P, Baptista AC, et al., 2021. An overview of high-entropy alloys as biomaterials., 11(4):648. https://doi.org/10.3390/MET11040648
Chao WX, Li YD, Sun XH, et al., 2021. Enhanced wood-derived photothermal evaporation system by in-situ incorporated lignin carbon quantum dots., 405:126703. https://doi.org/10.1016/j.cej.2020.126703
Chen L, Cheng LY, Wang Z, et al., 2021. Conditioned medium-electrospun fiber biomaterials for skin regeneration., 6(2):361-374. https://doi.org/10.1016/j.bioactmat.2020.08.022
Chu S, Wang AL, Bhattacharya A, et al., 2021. Protein based biomaterials for therapeutic and diagnostic applications., 4(1):012003. https://doi.org/10.1088/2516-1091/AC2841
Crist TE, Mathew PJ, Plotsker EL, et al., 2021. Biomaterials in craniomaxillofacial reconstruction: past, present, and future., 32(2):535-540. https://doi.org/10.1097/SCS.0000000000007079
Dargahi A, Sedaghati R, Rakheja S, 2019On the properties of magnetorheological elastomers in shear mode: design, fabrication and characterization, 159:269-283. https://doi.org/10.1016/j.compositesb.2018.09.080
do Nascimento MHM, Ferreira M, Malmonge SM, et al., 2017. Evaluation of cell interaction with polymeric biomaterials based on hyaluronic acid and chitosan., 28(5):68. https://doi.org/10.1007/s10856-017-5875-x
Dziadek M, Dziadek K, Checinska K, et al., 2021. PCL and PCL/bioactive glass biomaterials as carriers for biologically active polyphenolic compounds: comprehensive physicochemical and biological evaluation., 6(6):1811-1826. https://doi.org/10.1016/j.bioactmat.2020.11.025
González OM, García A, Guachambala M, et al., 2021. Innovative sandwich-like composite biopanels–towards a new building biomaterials concept for structural applications in nonconventional building systems., 16(2):132-148. https://doi.org/10.1080/17480272.2020.1819871
Govindan N, Mohammed MKA, Tamilarasu S, 2022. Nano-sized plant particles for next generation green-medicine., 309:131301. https://doi.org/10.1016/j.matlet.2021.131301
Hasan F, Al Mahmud KAH, Khan MI, et al., 2021. Cavitation induced damage in soft biomaterials., 3(1):67-87. https://doi.org/10.1007/S42493-021-00060-X
Hayajneh M, Al-Oqla FM, 2022. Physical and mechanical inherent characteristic investigations of various Jordanian natural fiber species to reveal their potential for green biomaterials., 19(13):7199-7212. https://doi.org/10.1080/15440478.2021.1944432
Holmes DW, Singh D, Lamont R, et al., 2022. Mechanical behaviour of flexible 3D printed gyroid structures as a tuneable replacement for soft padding foam., 50:102555. https://doi.org/10.1016/j.addma.2021.102555
Hussain S, Li SX, Mumtaz M, et al., 2021. Foliar application of silicon improves stem strength under low light stress by regulating lignin biosynthesis genes in soybean ((L.) Merr.)., 401:123256. https://doi.org/10.1016/j.jhazmat.2020.123256
Indurkar A, Pandit A, Jain R, et al., 2021. Plant-based biomaterials in tissue engineering., 21:e00127. https://doi.org/10.1016/j.bprint.2020.e00127
Jablonská E, Kubásek J, Vojtěch D, et al., 2021. Test conditions can significantly affect the results of in vitro cytotoxicity testing of degradable metallic biomaterials., 11(1):6628. https://doi.org/10.1038/s41598-021-85019-6
Janarthanan G, Noh I, 2021. Recent trends in metal ion based hydrogel biomaterials for tissue engineering and other biomedical applications., 63:35-53. https://doi.org/10.1016/j.jmst.2020.02.052
Jasim SA, Opulencia MJC, Ramírez-Coronel AA, et al., 2022. The emerging role of microbiota-derived short-chain fatty acids in immunometabolism., 110:108983. https://doi.org/10.1016/j.intimp.2022.108983
Jin M, Shi JL, Zhu WZ, et al., 2021. Polysaccharide-based biomaterials in tissue engineering: a review., 27(6):604-626. https://doi.org/10.1089/ten.teb.2020.0208
Jin S, Xia X, Huang JH, et al., 2021. Recent advances in PLGA-based biomaterials for bone tissue regeneration., 127:56-79. https://doi.org/10.1016/j.actbio.2021.03.067
Kalirajan C, Dukle A, Nathanael AJ, et al., 2021. A critical review on polymeric biomaterials for biomedical applications., 13(17):3015. https://doi.org/10.3390/polym13173015
Khalid MY, Al Rashid A, Arif ZU, et al., 2021. Recent advances in nanocellulose-based different biomaterials: types, properties, and emerging applications., 14:2601-2623. https://doi.org/10.1016/j.jmrt.2021.07.128
Książek M, 2021. Retracted: application of sulfur waste in biomaterials., 217:108848. https://doi.org/10.1016/j.compositesb.2021.108848
Kumar A, Collini L, Ursini C, et al., 2022. Energy absorption and stiffness of thin and thick-walled closed-cell 3D-printed structures fabricated from a hyperelastic soft polymer., 15(7):2441. https://doi.org/10.3390/ma15072441
Kumari S, Chatterjee K, 2021. Biomaterials-based formulations and surfaces to combat viral infectious diseases., 5(1):011503. https://doi.org/10.1063/5.0029486
Li YX, Wang SS, Jin LZ, et al., 2018. Self-assembly rules of dumbbell-shaped molecules and their effect on morphology and photophysical behaviors of micro/nanocrystals., 18(9):4822-4828. https://doi.org/10.1021/acs.cgd.8b00652
Liu YY, Jiang HM, Zhang LT, et al., 2022. Diluted acetic acid softened intermuscular bones from silver carp () by dissolving hydroxyapatite and collagen., 11(1):1. https://doi.org/10.3390/foods11010001
Liu ZQ, Liu XL, Ramakrishna S, 2021. Surface engineering of biomaterials in orthopedic and dental implants: strategies to improve osteointegration, bacteriostatic and bactericidal activities., 16(7):2000116. https://doi.org/10.1002/biot.202000116
Ma CL, Nikiforov A, de Geyter N, et al., 2022. Plasma for biomedical decontamination: from plasma-engineered to plasma-active antimicrobial surfaces., 36:100764. https://doi.org/10.1016/j.coche.2021.100764
Ma YM, Gao L, Tian YQ, et al., 2021. Advanced biomaterials in cell preservation: hypothermic preservation and cryopreservation., 131:97-116. https://doi.org/10.1016/j.actbio.2021.07.001
Mahmood RI, Kadhim AA, Ibraheem S, et al., 2022. Biosynthesis of copper oxide nanoparticles mediatedas cytotoxic and apoptosis inducer factor in breast cancer cell lines., 12(1):16165. https://doi.org/10.1038/S41598-022-20360-Y
Mohammed MKA, Ahmed DS, Mohammad MR, 2019. Studying antimicrobial activity of carbon nanotubes decorated with metal-doped ZnO hybrid materials., 6(5):055404. https://doi.org/10.1088/2053-1591/ab0687
Mohammed MKA, Mohammad MR, Jabir MS, et al., 2020. Functionalization, characterization, and antibacterial activity of single wall and multi wall carbon nanotubes., 757:012028. https://doi.org/10.1088/1757-899X/757/1/012028
Momin M, Mishra V, Gharat S, et al., 2021. Recent advancements in cellulose-based biomaterials for management of infected wounds., 18(11):1741-1760. https://doi.org/10.1080/17425247.2021.1989407
Mondal D, Griffith M, Venkatraman SS, 2016. Polycaprolactone-based biomaterials for tissue engineering and drug delivery: current scenario and challenges., 65(5):255-265. https://doi.org/10.1080/00914037.2015.1103241
Moreno MA, Gonzalez-Rico J, Lopez-Donaire ML, et al., 2021. New experimental insights into magneto-mechanical rate dependences of magnetorheological elastomers., 224:109148. https://doi.org/10.1016/j.compositesb.2021.109148
Morita J, Ando Y, Komatsu S, et al., 2021. Mechanical properties and reliability of parametrically designed architected materials using urethane elastomers., 13(5):842. https://doi.org/10.3390/polym13050842
Motameni A, Alshemary AZ, Evis Z, 2021. A review of synthesis methods, properties and use of monetite cements as filler for bone defects., 47(10):13245-13256. https://doi.org/10.1016/j.ceramint.2021.01.240
Musioł M, Sikorska W, Janeczek H, et al., 2018. (Bio)degradable polymeric materials for a sustainable future–part 1. Organic recycling of PLA/PBAT blends in the form of prototype packages with long shelf-life., 77:447-454. https://doi.org/10.1016/j.wasman.2018.04.030
Nace SE, Tiernan J, Holland D, et al., 2021. A comparative analysis of the compression characteristics of a thermoplastic polyurethane 3D printed in four infill patterns for comfort applications., 27(11):24-36. https://doi.org/10.1108/RPJ-07-2020-0155
Nickkholgh B, Hickerson DHM, Wilkins C, et al., 2022. Regenerative medicine: the newest cellular therapy.: Gee AP (Ed.), Cell Therapy. Springer, Cham, Germany, p.517-537. https://doi.org/10.1007/978-3-030-75537-9_33
Noori AS, Mageed NF, Abdalameer NK, et al., 2022. The histological effect of activated Aloe Vera extract by microwave plasma on wound healing., 807:140112. https://doi.org/10.1016/j.cplett.2022.140112
Nouri A, Shirvan AR, Li YC, et al., 2021. Additive manufacturing of metallic and polymeric load-bearing biomaterials using laser powder bed fusion: a review., 94:196-215. https://doi.org/10.1016/j.jmst.2021.03.058
Park KM, Min KS, Roh YS, 2022. Design optimization of lattice structures under compression: study of unit cell types and cell arrangements., 15(1):97. https://doi.org/10.3390/ma15010097
Park SY, Yun YH, Park BJ, et al., 2022. Fabrication and biological activities of plasmid DNA gene carrier nanoparticles based on biodegradable L-tyrosine polyurethane., 15(1):17. https://doi.org/10.3390/ph15010017
Qin LD, Yao S, Zhao JX, et al., 2021. Review on development and dental applications of polyetheretherketone-based biomaterials and restorations., 14(2):408. https://doi.org/10.3390/ma14020408
Rahmati M, Silva EA, Reseland JE, et al., 2020. Biological responses to physicochemical properties of biomaterial surface., 49(15):5178-5224. https://doi.org/10.1039/D0CS00103A
Rashid T, Sher F, Khan AS, et al., 2021. Effect of protic ionic liquid treatment on the pyrolysis products of lignin extracted from oil palm biomass., 291:120133. https://doi.org/10.1016/j.fuel.2021.120133
Roach DJ, Rohskopf A, Hamel CM, et al., 2021. Utilizing computer vision and artificial intelligence algorithms to predict and design the mechanical compression response of direct ink write 3D printed foam replacement structures., 41:101950. https://doi.org/10.1016/j.addma.2021.101950
Saadatmand M, Al-Awsi GRL, Alanazi AD, et al., 2021. Green synthesis of zinc nanoparticles usingVera. Extract by microwave method and its prophylactic effects oninfection., 28(11):6454-6460. https://doi.org/10.1016/j.sjbs.2021.07.007
Sadowska JM, Genoud KJ, Kelly DJ, et al., 2021. Bone biomaterials for overcoming antimicrobial resistance: advances in non-antibiotic antimicrobial approaches for regeneration of infected osseous tissue., 46:136-154. https://doi.org/10.1016/J.MATTOD.2020.12.018
Salihu R, Abd Razak SI, Zawawi NA, et al., 2021. Citric acid: a green cross-linker of biomaterials for biomedical applications., 146:110271. https://doi.org/10.1016/j.eurpolymj.2021.110271
Saydé T, El Hamoui O, Alies B, et al., 2021. Biomaterials for three-dimensional cell culture: from applications in oncology to nanotechnology., 11(2):481. https://doi.org/10.3390/nano11020481
Sivasankarapillai VS, Das SS, Sabir F, et al., 2021. Progress in natural polymer engineered biomaterials for transdermal drug delivery systems., 19:100382. https://doi.org/10.1016/j.mtchem.2020.100382
Suvindran N, Servati A, Servati P, 2022. Emerging biomedical and industrial applications of nanoporous materials.: Uthaman A, Thomas S, Li TD (Eds.), Advanced Functional Porous Materials. Springer, Cham, Germany, p.353-390. https://doi.org/10.1007/978-3-030-85397-6_11
Szczuka J, Sandomierski M, Buchwald T, 2022. Formation of the octadecylphosphonic acid layer on the surface of Ti6Al4V ELI titanium alloy and analysis using Raman spectroscopy., 265:120368. https://doi.org/10.1016/j.saa.2021.120368
Tao YB, Li P, Zhang HW, et al., 2022. Compression and flexural properties of rigid polyurethane foam composites reinforced with 3D-printed polylactic acid lattice structures., 279:114866. https://doi.org/10.1016/j.compstruct.2021.114866
Thrivikraman G, Madras G, Basu B, 2014. In vitro/in vivo assessment and mechanisms of toxicity of bioceramic materials and its wear particulates., 4(25):12763-12781. https://doi.org/10.1039/C3RA44483J
Vakil MK, Mansoori Y, Al-Awsi GRL, et al., 2022. Individual genetic variability mainly of proinflammatory cytokines, cytokine receptors, and toll-like receptors dictates pathophysiology of COVID-19 disease., 94(9):4088-4096. https://doi.org/10.1002/jmv.27849
Wan MC, Qin W, Lei C, et al., 2021. Biomaterials from the sea: future building blocks for biomedical applications., 6(12):4255-4285. https://doi.org/10.1016/j.bioactmat.2021.04.028
Wang F, Guo CC, Yang QQ, et al., 2021. Protein composites from silkworm cocoons as versatile biomaterials., 121:180-192. https://doi.org/10.1016/j.actbio.2020.11.037
Wang Y, Huang Y, Bai HY, et al., 2021. Biocompatible and biodegradable polymer optical fiber for biomedical application: a review., 11(12):472. https://doi.org/10.3390/bios11120472
Wang YM, Liu P, Zhang GF, et al., 2021. Cascading of engineered bioenergy plants and fungi sustainable for low-cost bioethanol and high-value biomaterials under green-like biomass processing., 137:110586. https://doi.org/10.1016/j.rser.2020.110586
Wilfred O, Tai HY, Marriott R, et al., 2018. Biodegradation of polyactic acid and starch composites in compost and soil., 1(2):1-11.
Wu S, Hu WQ, Ze QJ, et al., 2020. Multifunctional magnetic soft composites: a review., 3(4):042003. https://doi.org/10.1088/2399-7532/abcb0c
Xiang Y, Jin RR, Zhang Y, et al., 2021. Foldable glistening-free acrylic intraocular lens biomaterials with dual-side heterogeneous surface modification for postoperative endophthalmitis and posterior capsule opacification prophylaxis., 22(8):3510-3521. https://doi.org/10.1021/acs.biomac.1c00582
Xu C, Wang DY, Zhang SW, et al., 2021. Effect of lignin modifier on engineering performance of bituminous binder and mixture., 13(7):1083. https://doi.org/10.3390/POLYM13071083
Yeung DA, Kelly NH, 2021. The role of collagen-based biomaterials in chronic wound healing and sports medicine applications., 8(1):8. https://doi.org/10.3390/bioengineering8010008
Yilmaz B, Alshemary AZ, Evis Z, 2019. Co-doped hydroxyapatites as potential materials for biomedical applications., 144:443-453. https://doi.org/10.1016/j.microc.2018.10.007
Yu W, Maynard E, Chiaradia V, et al., 2021. Aliphatic polycarbonates from cyclic carbonate monomers and their application as biomaterials., 121(18):10865-10907. https://doi.org/10.1021/acs.chemrev.0c00883
Zhang L, Qu Y, Gu J, et al., 2021. Photoswitchable solvent-free DNA thermotropic liquid crystals toward self-erasable shape information recording biomaterials., 12:100140. https://doi.org/10.1016/j.mtbio.2021.100140
Zhao K, Yang X, Chen GQ, et al., 2002. Effect of lipase treatment on the biocompatibility of microbial polyhydroxyalkanoates., 13(9):849-854. https://doi.org/10.1023/A:1016596228316
Electronic supplementary materials
Data S1
题目:最新综述:生物材料类型、性能、医疗应用及其他因素
作者:Reeya AGRAWAL1,3, Anjan KUMAR1, Mustafa K. A. MOHAMMED2, Sangeeta SINGH3
机构:VLSI Research Centre, GLA University, 281406 Mathura, India; Radiological Techniques Department, Al-Mustaqbal University College, 51001 Hillah, Babylon, Iraq; Microelectronics & VLSI Lab, National Institute of Technology, Patna 800005, India
概要:当患者体内的受损器官/组织被修复/替代后,患者的生活质量将会得到大幅改善。用于人体植入性治疗的生物材料必须具备特定的性能。人体对生物材料的接受程度是决定器官修复/移植成败的关键因素。最新的生物材料的结构应与组织内的结构相似。当前,基于先进的抗污、杀菌及抗生物膜技术,研究者正在研发抗感染的生物材料;它在现代医疗中预防和治疗重大传染性疾病是不可或缺的。这些对生物材料提出了新的要求。将来的研究热点之一是制备人体植入物的材料,并添加金属、陶瓷及聚合物。这篇综述涵盖了组织工程所需的生物材料的概念、关键特征以及生物材料(包括生物活性材料和生物可吸收材料)在医疗实践中的应用,并将会帮助研究者更好地选取生物材料。
关键词:生物材料;医疗应用;受损器官或组织;修复;移植
https://doi.org/10.1631/jzus.A2200403
https://doi.org/10.1631/jzus.A2200403
Jan. 5, 2023;
Mar. 2, 2023
© Zhejiang University Press 2023
Aug. 19, 2022;
Nov. 2, 2022;
 Journal of Zhejiang University-Science A(Applied Physics & Engineering)2023年11期
Journal of Zhejiang University-Science A(Applied Physics & Engineering)2023年11期
- Journal of Zhejiang University-Science A(Applied Physics & Engineering)的其它文章
- Experimental and theoretical analysis of a hybrid vibration energy harvester with integrated piezoelectric and electromagnetic interaction
- Advances in micro-nano biosensing platforms for intracellular electrophysiology
- Correlation between travel experiences and post-COVID outbound tourism intention: a case study from China
- Experimental investigation on cenosphere-aluminum syntactic foam-filled tubes under axial impact loading
- Short-term tunnel-settlement prediction based on Bayesian wavelet: a probability analysis method
- Effect of carbon dioxide concentration on the combustion characteristics of boron agglomerates in oxygen-containing atmospheres
