Analysis of independent risk factors for acute acquired comitant esotropia
Jie Cai, Wei-Xia Lai, Xia Li, Qin Li, Ying Cai, Jin-Mao Chen
1Department of Ophthalmology, the First Affiliated Hospital of Guangxi Medical University, Nanning 530021, Guangxi Zhuang Autonomous Region, China
2Department of Ophthalmology, the First Affiliated Hospital of Guangxi University of Chinese Medicine, Nanning 530022,Guangxi Zhuang Autonomous Region, China
3Nanning Aier Eye Hospital, Nanning 530001, Guangxi Zhuang Autonomous Region, China
Abstract
● KEYWORDS: acute acquired comitant esotropia;strabismus; risk factors
INTRODUCTION
Acute acquired comitant esotropia (AACE) is a rare type of esotropia that can occur in children and adults.It is characterized by sudden onset of concomitant esotropia with minimal accommodative effect and potential for good binocular vision[1].AACE was previously considered as a rare disease, but in recent years, with the widespread use of video terminals, increasing prevalence of myopia, and high intensity near work, the number of patients with AACE has shown a significant increase.Especially since the outbreak of the COVID-19 at the end of 2019, there has been a significant increase in AACE patients who seek medical treatment for diplopia and esotropia[2].However, the etiology of AACE is still not clear.Previous literature reports have suggested that uncorrected myopia, prolonged near work, increased medial rectus muscle tension, and factors such as compensatory heterophoria, disruption of fusion function, and anatomical structure of the extraocular muscles may contribute to the development of AACE[1,3-7].In addition, inappropriate use of electronic devices appears to have contributed to an increase in the prevalence of this type of strabismus over the past few years, especially during the COVID-19 pandemic[8-11].Therefore, the aim of this study is to evaluate the risk factors for AACE, in order to provide insights for the prevention of AACE.
SUBJECTS AND METHODS
Ethical ApprovalThis study followed the principles of the Helsinki Declaration and was approved by the Ethics Committee of the First Αffiliated Hospital of Guangxi Medical University (Ethics approval number: 2022-E467-01).All patients in this study signed informed consent.
General InformationThis retrospective study included a case group consisting of 83 patients diagnosed with AACE who underwent horizontal rectus muscle surgery at the First Affiliated Hospital of Guangxi Medical University between January 1, 2021, and June 30, 2022.The study aimed to assess the characteristics and risk factors associated with AACE.Inclusion criteria for the case group were as follows:1) onset age of 5y or older, presenting with acute acquired non-accommodative esotropia and initial distance diplopia; 2)normal eye movement function, with a difference of less than 5 prism degree (PD) of esotropia across all diagnostic gaze positions; 3) disease duration of at least 6mo at the time of surgery; 4) confirmation of absence of neurological or systemic diseasesviahead and eye socket computed tomography(CT) or magnetic resonance imaging (MRI) examination; 5)best-corrected visual acuity (BCVA) of 0.5 or higher in each eye.During the same study period, a total of 73 outpatient volunteers were recruited as the normal control group.The inclusion criteria for the control group were as follows: 1)BCVA of 0.5 or higher in each eye; 2) presence of orthophoria and normal eye movement in both eyes; 3) no symptoms of diplopia or visual fatigue; 4) no history of eye or systemic diseases, except refractive errors; 5) age between 5 and 50y.Exclusion criteria for both the case and control groups included amblyopia, history of eye surgery, cranial injury, neurological deficits, infantile esotropia, and history of systemic diseases such as hyperthyroidism or myasthenia gravis.
Examination MethodsAge, gender, glasses prescription, and age of onset of diplopia were collected for all patients in the case group.All patients underwent routine eye examinations and cycloplegic refraction assessment using retinoscopy.Patients aged 12y or younger received atropine eye ointment 3 times per day for 3 consecutive days, while those older than 12y received compound tropicamide eye drops 3 times with a 5-minute interval, followed by retinoscopy examination 30min later.Patients in the case group with hyperopia of ≥1.0 D were provided with corrective glasses.Binocular vision was assessed using the four-hole lamp at distances of 6m and 33 cm, and the synoptophore was used to evaluate the degree of esotropia in different gaze positions.Stereopsis was evaluated using the Titmus stereo test.BCVA was recorded using the decimal notation and then converted to the logarithm of the minimum angle of resolution (logMAR).The case group underwent examination of distant and near esotropia degree at 6 m and 33 cm using corneal reflex combined with prism,alternating prism cover test and Maldox rod methods.Based on the degree of esotropia, conventional unilateral/bilateral medial rectus resection and lateral rectus recession surgeries were performed.A questionnaire survey on eye usage was conducted for all participants in the case and control groups,which included daily near-work time (working time on video display terminals such as mobile phones, computers,tablets, and non-video display terminals), adequacy of glasses prescription, whether glasses were worn for near work, and whether near work was often performed in a supine position(working time on video display terminals such as mobile phones, computers, tablets, and non-video display terminals).The questionnaire is open-ended and is administered by the doctors after questioning patients.
Statistical AnalysisStatistical analysis was performed using SPSS 26.0 software.Continuous variables were presented as means and standard deviations.Independent samplest-test was utilized for analysis when the data followed a normal distribution.For data that did not follow a normal distribution,non-parametric tests were employed for intergroup comparisons.Categorical data were analyzed using the Chisquare test.Univariate and multivariate logistic regression analyses were conducted to assess the risk factors for AACE.P<0.05 was considered statistically significant.
RESULTS
Basic InformationThe case group consisted of 83 individuals, including 50 males and 33 females, while the control group included 73 individuals, with 40 males and 33 females.The mean age in the case group was 22.52±10.72y(range: 5-52y), and in the control group, it was 21.30±1.00y(range: 6-50y).Among the case group, 61 individuals had myopia, with a mean spherical equivalent (SE) of -3.35±3.31 D(range: +2.75 to -10.62 D) of the right eye and -2.87±3.35 D(range: +2.75 to -11.12 D) of the left eye.In the control group,65 individuals had myopia, with a mean SE of -4.17±2.69 D(range: 0 to -14.75 D) of the right eye and -3.69±2.52 D (range:0.25 to -9.82 D) of the left eye.There were no significant differences in terms of gender, age, BCVA, SE, or myopia between the case and control groups (P>0.05).The daily close-up work time for the case group was 5.47±2.41h (range:2-12h), which was significantly higher than 4.55±1.35h (range:2-8h) of the control group.The proportion of individuals with uncorrected refractive errors, those working at near distance without glasses, and those working in a supine position at near distance was significantly higher in the case group compared to the control group.Detailed clinical characteristics of both groups are presented in Table 1.The mean duration of diplopiain the case group was 29.83±35.72mo (range: 0.5-240mo),and 80 patients (96.39%) had distance diplopia.Preoperative four-hole lamp examination (distance and near) revealed varying degrees of binocular visual function destruction in 75 cases (90.36%) and preoperative stereopsis dysfunction in 59 cases (71.08%).The postoperative prism deviation at near and distance was 52.36±20.95 PD (range: 10-140 PD) and 56.71±19.54 PD (range: 14-140 PD), respectively, with no statistically significant difference (t=1.38,P=0.169).

Table 2 Univariate logistic regression analysis of risk factors for AACE
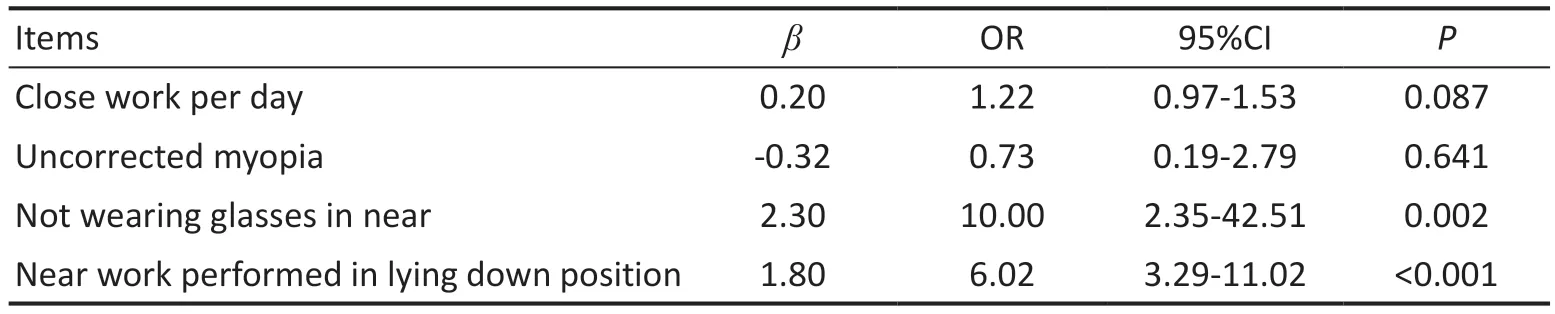
Table 3 Multivariate logistic regression analysis of risk factors for AACE
Analysis of Acute Acquired Comitant Esotropia Risk FactorsSingle-factor logistic regression analysis showed that daily close work duration, wearing uncorrected glasses,near work without glasses, and working at a close distance while lying down were all associated with an increased risk of AACE (P<0.05; Table 2).Multivariate logistic regression analysis showed that not wearing glasses for near work (β=2.30,P=0.002) and near work in supine position (β=1.80,P<0.001)were independent risk factors for AACE (Table 3).
DISCUSSION
In 1958, Burian and Miller[12]classified ΑΑCE into three types(Swan type, Burian-Franceschetti type, and Bielschowsky type).Among them, Bielschowsky type occurs in adults with uncorrected myopia less than 5.00 D[13].The disease onset is characterized by esotropia and ipsilateral diplopia when looking at a distance, while maintaining binocular single vision when looking at close objects.However, the exact cause of AACE is still unknown.In this study, myopia was the main refractive error in both the case and control groups, with a high degree of variability in the case group.Alongside the typical myopia patients with a degree greater than 5.00 D, there were also patients with highly myopic eyes exhibiting anisometropia or bilateral high myopia, which may be attributed to the increasing prevalence of myopia in recent years.The age range of the case group was 5 to 52y, with 5 patients over 40 years old, indicating that elderly patients with a decline in physiological regulation (the decrease in accomodative amplitude with age, with symptoms of eyestrain during sustained near effort) can also develop ΑΑCE, similar to the study by Zhenget al[14].Furthermore, elderly patients with a need for close vision rely more on accommodative reserves,leading to more pronounced diplopia and discomfort with near vision.This finding aligns with the research conducted by Ruatta and Schiavi[4], which indicated that patients with reduced accommodative function, such as those with artificial crystalline lenses or presbyopia, can also develop AACE.The accommodative parameters of AACE patients, such as the accommodative near point and accommodation convergence/accommodation (AC/A) ratio, were found to be within the normal range, suggesting that accommodative factors are not the cause of AACE[4].However, the possibility that excessive accommodation induced by high-intensity near work contributes to convergence excess cannot be ruled out.The characteristic diplopia in AACE patients in this study initially presented with distance vision, often manifesting as diplopia and visual fatigue when looking at traffic signs, roads,blackboards, or distant targets.Although the diplopia can be alleviated at first, it also occurs during close-range visual tasks as the disease progresses, but farsightedness predominates.There was no significant difference in the degree of esotropia between near and far distances in the patients.Ruatta and Schiavi[4]believe that the divergent fusional amplitude at close distances is greater than that at far distances and is sufficient to compensate for the esodeviation at near fixation, which is why patients mainly complain of diplopia during distance vision.Additionally, we observed a significant difference between the esotropia degree measured by corneal reflex and the actual esotropia degree in AACE patients.In clinical practice,it is often observed that the esotropia degree measured by corneal reflex is small or even not apparent, but with thorough alternating cover testing, a larger degree of deviation is often detected.It suggests that the deviation is intermittent and the patient possesses the ability to actively control the ocular misalignment.However alternating cover testing dissociates the eye and breaks the fusion leading to manifestation of the deviation.Furthermore, the observed increase in deviation during accommodative effort when presented with an actual accommodative target instead of light further supports the possibility that deviation is influenced by the accommodative response.In addition to alternating cover testing, we also employed the prism combined with the Maddox rod method to fully separate binocular images and avoid underestimating the preoperative esotropia degree.The phenomenon of a small corneal reflex deviation and a large prism testing deviation in AACE may be associated with abnormal accommodative function, which requires further investigation.
Through the questionnaire survey, we observed that the incidence of poor vision correction, such as wearing glasses with an incorrect prescription (73.49%) and not wearing glasses for near vision (61.45%), as well as poor eye habits,such as working at a close distance while lying down (60.24%)and the duration of near vision work (5.47±2.41h), were significantly higher in the case group when compared to the control group (P<0.05).This suggests a close relationship between refractive correction, eye habits, and the occurrence of AACE.Generally, a healthy binocular visual system with strong binocular fusion function can compensate for diplopia caused by binocular position deviation.However, if there are risk factors that lead to a decrease in binocular fusion function,diplopia may occur[14].In our study, not wearing glasses for near vision and working at a close distance while lying down were identified as independent risk factors for AACE.Since myopia is linearly associated with the duration of near vision work, the multiple regression model did not include myopia as a risk factor.
Previous studies have suggested that uncorrected myopia is a risk factor for AACE[12,14-16].However, in our study, wearing glasses with an incorrect prescription was not found to be a risk factor, while not wearing glasses for near vision was associated with an increased risk of AACE, which aligns with the findings by Zhenget al[14].Nonetheless, the causeand-effect relationship between myopia and AACE is still controversial.Caiet al[1]discovered that out of 41 myopia patients, 23 had fully corrected myopia and regularly wore glasses but still developed AACE.Spierer[17]referred to this type of AACE as “adult-onset acute concomitant esotropia”,a distinct subgroup of AACE.Ruatta and Schiavi[4]examined 26 patients with AACE, all of whom had myopia and wore fully corrective glasses throughout the day, with normal fusional function.Therefore, they concluded that uncorrected myopia was not a causative factor in AACE.However, their study included patients with small deviations in the angle of squint (average 23.7 PD), whereas in our study, the angle of squint was generally larger, which may explain the disparity in results.Typically, myopic patients do not wear glasses for near work, leading to reduced accommodative ability and convergence, making them susceptible to exotropia.
However, Burian and Miller[12]proposed that in uncorrected myopia patients, the distance between the target and the eye is shortened during near vision.The closer the distance, the weaker the compensatory force exerted by the nerve fibers responsible for relaxing the eye muscles, resulting in increased tension of the medial rectus muscle.When compensatory fusional divergence fails to counteract the increased tension of the medial rectus muscle, esotropia occurs.This theory is supported by pathological examinations of the medial rectus muscle in ΑΑCE patients, which have shown a deficiency of muscle fibers and an abundance of collagen fibers, impairing the muscle’s ability to relax effectively, particularly during distant vision[5].Aliet al[6]suggested that patients with AACE had latent heterotropia prior to the onset of diplopia.It is known that the ability of the eyes to fuse images is crucial for overcoming heterotropia.It is demonstrated that adult myopic patients with AACE exhibit impaired fusion divergence function, characterized by decreased fusion convergence and increased fusion divergence, serving as an adaptive mechanism to maintain fusion in the presence of heterotropia[18].With increasing myopia, the adaptive capacity of fusion convergence diminishes.Wearing glasses for near vision in myopic patients stimulates accommodative convergence, thereby exercising fusion divergence.Not wearing glasses for near vision may lead to decreased accommodative convergence and reduced fusion divergence, which can result in the failure to compensate for latent heterotropia and the onset of diplopia[14].Similarly, working at a close distance in a supine position also reduces the distance between the target and the eyes.In our study, patients in the case group often failed to wear glasses when working at a close distance in a supine position.Under unfavorable conditions of excessive close-range work,the previously existing balance between convergence and divergence is disrupted, with the strength of the medial rectus muscle surpassing the average level while the lateral rectus muscle weakens due to constant stretching.
Previous studies have suggested that prolonged near work,especially with the use of smartphones, may be a risk factor for AACE[19-20].Zhenget al[14]revealed through a matched casecontrol study that prolonged near work is an independent risk factor for AACE.They believe that prolonged near work itself leads to an increase in the tension of the medial rectus muscle,and that long-term work on video terminals disrupts regulation and balance, leading to AACE.However, our results are inconsistent with these findings.Αlthough the daily near work time of the case group (5.47±2.41h) is longer than that of the control group (4.55±1.35h), the multivariate logistic regression analysis showed that prolonged near work is not a risk factor for ΑΑCE.This may be related to differences in the selection of the control group and a lack of a sufficiently large sample size.At the same time, the pervasive integration of smart video terminal products into various aspect of individual’s lives is evident, as these devices have become essential not only for daily work and study but also for leisure and entertainment purposes.Whether prolonged near work is an independent risk factor for AACE still requires multicenter large-sample clinical research.
In summary, AACE patients exhibit mainly far vision double vision, and there is high variability in the nearsightedness diopters.AACE can occur in patients aged 5 to 52 years old,and not wearing glasses for near work and working at a close distance while lying down are independent risk factors for AACE.
ACKNOWLEDGEMENTS
Foundations:Supported by the Guangxi Health Appropriate Technology Development and Application Project (No.S2021093); the Education and Teaching Reform Project of Guangxi Medical University (No.2021XJGA18).
Conflicts of Interest:Cai J,None;Lai WX,None;Li X,None;Li Q,None;Cai Y,None;Chen JM,None.
 International Journal of Ophthalmology2023年11期
International Journal of Ophthalmology2023年11期
- International Journal of Ophthalmology的其它文章
- Quantitative analysis of optic disc changes in school-age children with ametropia based on artificial intelligence
- Association analysis of Bcll with benign lymphoepithelial lesions of the lacrimal gland and glucocorticoids resistance
- In vitro protective effect of recombinant prominin-1 combined with microRNA-29b on N-methyl-D-aspartateinduced excitotoxicity in retinal ganglion cells
- Bioinformatics and in vitro study reveal the roles of microRNA-346 in high glucose-induced human retinal pigment epithelial cell damage
- Therapeutic effect of folic acid combined with decitabine on diabetic mice
- Comparison of visual performance with iTrace analyzer following femtosecond laser-assisted cataract surgery with bilateral implantation of two different trifocal intraocular lenses
