Changes in corneal biomechanics and posterior corneal surface elevation after FS-LASlK
Zhong-Ji Li, Chen Yang, Su-Han Liu, Jiao Guo, Yu-Hui Duan
Department of Ophthalmology, Xi’an Gaoxin Hospital, Xi’an 710075, Shaanxi Province, China
Abstract
● KEYWORDS: femtosecond laser-assisted in situ keratomileusis; corneal biomechanics; posterior corneal surface elevation
INTRODUCTION
Femtosecond laser-assistedin situkeratomileusis (FSLASIK) is one of the safe and effective methods available for correcting refractive errors[1].In recent years,with the advancement of technology, the femtosecond laser has been used in laser corneal refractive surgery due to its extreme precision and safety, significantly reducing the risks associated with corneal flaps.FS-LΑSIK surgery results in a reduction in the thickness of the corneal stromal bed, causing a redistribution of corneal morphology in response to intraocular pressure (IOP), thereby altering the refractive power of the cornea.In recent years, changes in the posterior corneal surface morphology after laser corneal refractive surgery have received increasing attention, affecting the stability of the postoperative corneal refractive state and having significant clinical value for the long-term prediction and risk assessment of the procedure[2].The complications associated with the procedure itself remain a significant concern for surgeons, mainly referring to iatrogenic keratectasia, which is currently thought to be related to individual genetic susceptibility or altered corneal biomechanics due to excessive corneal stromal ablation,with an incidence of approximately 0.04% to 0.6% and 80%occurring within two years of the procedure[3-4].Seileret al[5]first reported secondary keratoconus after LΑSIK in 1998, and similar cases have been reported since then[6-7].Previous studies have suggested that the residual corneal stroma thickness/corneal thickness (RCST/CT) is a more accurate reflection of the effect of laser corneal refractive surgery on the cornea[8].Based on the difference between RCST/CT, we investigated the changes in corneal biomechanical parameters and posterior corneal surface elevation after FS-LASIK and their correlation by using the ocular response analyzer (ORA) and Pentacam to provide a reference for clinical application.
SUBJECTS AND METHODS
Ethical ApprovalThe study protocol was approved by Xi’an Gaoxin Hospital Medical Ethics Committee (approval No.GXYYEC-2021001) and adhered to the Declaration of Helsinki.Written informed consent was obtained from all patients before the surgery.
ParticipantsThis case-series study retrospectively enrolled 100 participants (197 eyes) with myopia or myopic astigmatism aged 18 to 39y (28.45±7.58y) who received FSLASIK surgery between April 2022 to November 2022 at the Department of Ophthalmology of Xi’an Gaoxin Hospital,including 46 males (92 eyes) and 54 females (105 eyes).Their preoperative spherical equivalent (SE) were from -5.75 to-9.63 D (-7.76±1.21 D).Visual acuity, manifest refraction, IOP,slit lamp microscopy, ORA and Pentacam were performed preoperatively and 1 and 3mo postoperatively.Inclusion criteria were: 1) preoperative thinnest corneal thickness more than 450 μm, postoperative remaining corneal stromal bed thickness more than 300 μm; 2) discontinuing soft contact lens wear for over 2wk, rigid contact lens wear for over 1mo or orthokeratology lens wear for over 3mo prior to the procedure; 3) the refractive error has been relatively stable for the past two years (myopia increasing by less than 0.50 D per year).Exclusion criteria were: 1) active ocular disease; 2)keratoconus or suspicious corneal topography; 3) history of ocular surgery or trauma; 4) pregnancy or lactation.
GroupsAll participants were divided into three groups according to the ratio of postoperative RCST/CT: Group I(50%≤RCST/CT<55%, 63 eyes of 32 patients), Group II(55%≤RCST/CT<60%, 67 eyes of 34 patients), and Group III(RCST/CT≥60%, 67 eyes of 34 patients).
Examination of Corneal Biomechanical Parameters and Posterior Corneal Surface ElevationORA is applied to measure Goldmann correlated IOP, corneal compensated IOP(IOPcc), corneal hysteresis (CH) and corneal resistance factor(CRF).Measurements were taken three times in each eye and averaged for statistical analysis.The difference between preoperative and postoperative values was recorded as ΔIOP,ΔIOPcc, ΔCH, and ΔCRF.Positive values indicated that IOP,IOPcc, CH, and CRF decreased after surgery compared to preoperative values.
Pentacam was used to measure the posterior corneal surface elevation under the darkroom preoperatively, 1 and 3mo postoperatively.The postoperative and preoperative posterior corneal surface elevation maps were overlapped and compared.The same posterior best-fit sphere (PBSF) was set.The corresponding point difference between postoperative and preoperative elevation was the posterior elevation difference(PED).Positive values indicate forward ectasia of the posterior corneal surface.The maximum PED value within 6 mm diameter of the corneal apex was used in the study.
Surgical Procedures and Postoperative ManagementBefore surgery, 4 g/L of oxybuprocaine hydrochloride eyedrops were used for surface anaesthesia.VisuMax femtosecond laser(Carl Zeiss, Germany) was used to create the corneal flap.The hinge of the flap was located at 90°, the thickness was 100 μm,the diameter was 8.1 mm, and the flap margin incision angle was 90°.Then, the patient was transferred to the excimer laser treatment area.The corneal stromal ablation was performed using the Amaris 1050RS excimer laser.The diameter of the optical zone was 6.0-7.0 mm.Reset the corneal flap after the laser scanning was completed and wash the corneal layers with balanced salt solution.Αfter flattening the corneal flap, a sterile eye mask was used to wrap the treated eye.To ensure consistent results, all surgeries were performed by the same experienced surgeon.
The postoperative regimen included administration of topical 0.5% levofloxacin eyedrops (Tarivid; Santen, Inc., Japan),0.25% tobramycin and dexamethasone eyedrops (Maxidex;Alcon Laboratories, Inc., Japan) four times per day for 1wk;and 0.1% fluorometholone eyedrops (Tarivid; Santen, Inc.,Japan) four times per day for 3wk.In addition, preservativefree lacrimal substitutes were used as needed.
Statistical AnalysisStatistical analysis was performed using SPSS (GLM UNIVARIATE, version 20, IBM, USA).Repeated measures ANOVA was used to compare IOP, IOPcc,CH, and CRF among and within groups, and SNK-qwas used to compare multiple measures between groups and at various time points.The PED value of each group at the same time after surgery was compared by one-way ANOVA analysis.Comparison of PED value at different time after surgery in each group was performed by paired samplet-test.Pearson correlation analysis was performed between ΔIOP, ΔIOPcc,ΔCH, ΔCRF, and PED, respectively.P<0.05 was regarded as significant.
RESULTS
Comparison of Preoperative Parameters, Postoperative SE and Visual AcuityThere were no statistically significant differences in gender, age, preoperative thinnest corneal thickness,preoperative best corrected visual acuity (BCVA), IOP, IOPcc,CH, CRF, and postoperative SE, uncorrected distance visual acuity (UDVA), and BCVA among three groups (Table 1).
Comparison of IOP, IOPcc, CH, and CRF Among Groups at Different TimesIOP, CH, and CRF were statisticallydifferent among different RCST/CT groups (F=12.99,34.148, 23.998, respectively, allP<0.001) and different times(F=699.635, 308.474, 640.145, respectively, allP<0.001), but the interaction of RCST/CT and times were not significant(F=1.832, 1.110, 2.776,P=0.163, 0.349, 0.065, respectively).The IOP, CH, and CRF of Group I were the lowest in three groups.There was no statistically significant difference of IOPcc among the three groups (F=0.603,P>0.05).IOPcc was statistically different at differents times (F=104.125,P<0.001),but the interaction of RCST/CT and times were not significant(F=0.854,P=0.427).
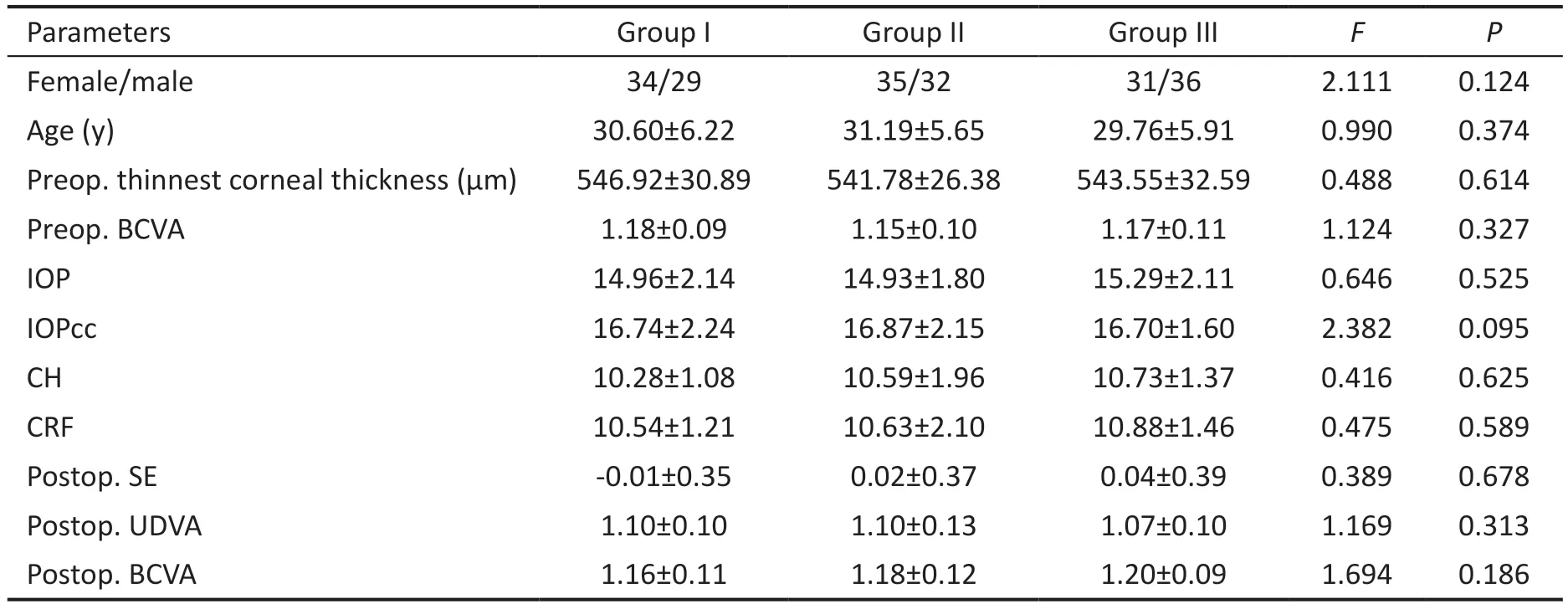
Table 1 Comparison of preoperative parameters, postoperative SE, and visual acuity mean±SD

Table 2 Comparison of IOP, IOPcc, CH, and CRF at different times mean±SD
Comparison of IOP, IOPcc, CH, CRF, and PED in Each Group at Different TimesIOP, IOPcc, CH, and CRF were statistically different at different times before and after surgery.
At 1 and 3mo after operation, the IOP, IOPcc, CH, and CRF decreased significantly compared with those before operation(Table 2).There were no statistically significant differences in IOP, IOPcc, CH, and CRF between 3 and 1mo after surgery(P>0.05).PED mong the three groups were statistically different at 1 and 3mo after surgery (F=223.22, 171.79,respectively, bothP<0.001).PED of Group I was the highest in three groups.The PED of 3mo after surgery decreased in each group compared with 1mo after surgery, but there was no statistical difference (Group I:t=0.82,P=0.41; Group II:t=0.17,P=0.87; Group III:t=1.35,P=0.18).
Correlation Analysis of ΔIOP, ΔIOPc, ΔCH, and ΔCRF with PEDCorrelations between corneal biomechanical parameters and PED were performed at 1 and 3mo postoperatively in threegroups respectively.There was no correlation between ΔIOP,ΔIOPcc, ΔCH, or ΔCRF and PED (allP>0.05; Tables 3 and 4).
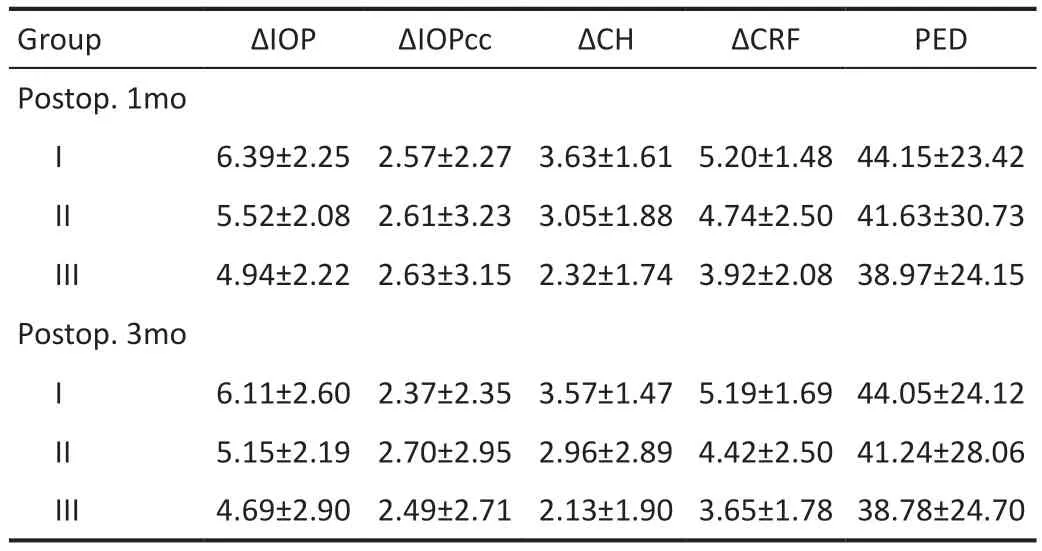
Table 3 ΔIOPg, ΔIOPcc, ΔCH, ΔCRF and PED at different postoperative times in three groups mean±SD

Table 4 Correlation analysis between ΔIOP, ΔIOPcc, ΔCH, or ΔCRF and PED
DISCUSSION
With the development of laser corneal refractive surgery, the femtosecond laser has replaced the microkeratome that has been used for nearly two decades and undertakes the critical task of making corneal flaps in LASIK surgery, significantly reducing the risks associated with corneal flaps and bringing corneal refractive surgery into the era of the pure laser.However, iatrogenic keratectasia after FS-LASIK surgery is still the most crucial focus of laser corneal refractive surgeons.The main reason for its occurrence is that excessive ablation of the corneal stroma leads to the change of corneal biomechanics, and then the change of corneal morphology.In this study, the changes in corneal biomechanical parameters and posterior corneal surface elevation after FS-LASIK and their correlation were analyzed to ensure the safety and stability of operation.By comparing corneal biomechanical parameters after FS-LASIK, we found that IOP, IOPcc, CH,and CRF all decreased in patients after surgery compared to the preoperative period, indicating that FS-LASIK surgery has an effect on corneal biomechanics and that excimer laser ablation of the corneal stroma leads to a decrease in corneal biomechanical properties.Then, the postoperative corneal posterior surface elevation was all increased compared to the preoperative period, indicating that the posterior corneal surface shifted forward after FS-LASIK, but not enough to cause keratectasia.The smaller the RCST/CT, the greater the effect on the corneal biomechanical properties and posterior corneal surface morphology.There was no correlation between changes in corneal biomechanics and changes in posterior surface elevation in the RCST/CT≥50% range.Over time,the changes in corneal biomechanics and posterior surface morphology gradually stabilized.
As a living biological tissue, a complete description of the corneal properties should include, in addition to morphological indicators such as corneal thickness and curvature, the biomechanical properties it exhibits when subjected to forces.It has non-linear, anisotropic and viscoelastic properties(including creep, stress relaxation and hysteresis).The anisotropy of the internal structure of the cornea is an essential determinant of corneal morphological changes following keratectasia disease and corneal refractive surgery.In addition,it can affect the postoperative corneal load-bearing capacity and morphological stability.The ORA is considered to be one of the most commonly used instruments in clinical practice to measure living corneal biomechanical parameters,providing both IOP and IOPcc, as well as it can measure corneal biomechanical parameters, including CH and CRF to quantify corneal viscoelasticity[9].CH mainly reflects the ability of the cornea to absorb and disperse energy.CRF reflects the cumulative effect of resistance, including viscous resistance and elastic resistance, when the cornea is deformed by airflow compression.By comparing corneal biomechanical parameters after FS-LASIK, we found that IOP, IOPcc, CH,and CRF all decreased in patients after surgery compared to the preoperative period, indicating that FS-LASIK surgery has an effect on corneal biomechanics and that excimer laser ablation of the corneal stroma leads to a decrease in corneal biomechanical properties, which is consistent with the findings of other scholars[10-11].The significantly lower IOP measurements in this study compared to the preoperative period suggest that there is an underestimation of IOPcc values after laser corneal refractive surgery, despite the systematic correction and compensation for thickness effects[12].Therefore,IOP values measured using ORA should be further corrected for postoperative follow-up patients to avoid missing patients with potential glaucoma after surgery.Our comparison of corneal biomechanical parameters at different times after FSLASIK revealed that IOP, IOPcc, CH, and CRF increased at 3mo postoperatively compared to the respective values at 1mo.However, none of them was statistically different, suggesting that the changes in corneal biomechanical properties have basically stabilized at 1mo postoperatively.
In the earliest clinical applications, the remaining corneal stromal thickness of 250 μm after LΑSIK surgery has been considered the golden standard for evaluating surgical safety.However, many physicians have reported cases of postoperative corneal ectasia in patients who meet this criterion[13-15], suggesting that an RCST of 250 μm is insufficient to maintain corneal biomechanical stability[16].Leeet al[17]advocated that the percentage of ablation depth to total corneal thickness was included as one of the safety conditions of surgery and found that the elevation change of the posterior corneal surface after surgery was less in patients with a ablation ratio <20%.We believe that RCST/CT was more accurately and intuitively reflected the impact of LΑSIK surgery on the cornea.In this study, the postoperative corneal biomechanical parameters of patients with different RCST/CT were analyzed.It was found that there were statistically significant differences in IOP, IOPcc, CH, and CRF.These above values in Group I were significantly lower than those in Group II, Group II was significantly lower than Group III.It showed that RCST/CT affected corneal biomechanics, which changed considerably in patients with small RCST/CT.
FS-LASIK surgery results in a reduction in the thickness of the corneal stromal bed, causing a redistribution of corneal morphology in response to IOP, thereby altering the refractive power of the cornea.In recent years, changes in the posterior corneal surface morphology after laser corneal refractive surgery have received increasing attention, affecting the stability of the postoperative corneal refractive state and having significant clinical value for the long-term prediction and risk assessment of the procedure[2-18].The posterior corneal surface elevation can objectively and accurately reflect the degree of corneal bulge and is, therefore, often used to evaluate changes in corneal morphology after surgery.Our study revealed that the postoperative corneal posterior surface elevation was all increased compared to the preoperative period, indicating that the posterior corneal surface shifted forward after FS-LASIK,but not enough to cause keratectasia, which is consistent with the findings of other scholars[19-20].We analyzed the postoperative PED of patients with different RCST/CT.We found that the PED in Group I were significantly greater than those in Group II, and Group II were significantly greater than those in Group III, but the PED values of postoperative 3mo in all three groups were reduced compared to 1mo.It indicates that the ratio of the postoperative RCST affects the posterior corneal surface elevation, with patients with a small RCST/CT having a more obvious amount of postoperative posterior corneal surface bulge.As time lengthens, the corneal stromal collagen fibers gradually repair, and their structural arrangement becomes more orderly than in the early stage.As a result, the posterior corneal surface morphology gradually shifts back towards the preoperative state, thus achieving stability.
The change in corneal biomechanics after laser corneal refractive surgery was closely related to the change of corneal morphology, in which the change of posterior surface morphology was significantly smaller than that of the anterior surface.Zhanget al[21]found that the biomechanical hardness of the cornea was negatively correlated with the corneal central anterior surface elevation and the average corneal curvature and positively correlated with the Q value of the corneal anterior surface.This study found no correlation between ΔIOP, ΔIOPcc, ΔCH, or ΔCRF, and PED, which is consistent with previous studies[22].The results showed that the posterior corneal surface morphology was not affected by the corneal biomechanical changes when RCST/CT≥50% after FS-LΑSIK.The change of posterior corneal surface morphology after FSLASIK may be related to factors such as early postoperative corneal edema, structural repair and reconstruction of corneal collagen fibers, and individual differences in patients[23].
The follow-up period of this study was short, and longerterm observation after surgery is still needed.In addition, we still need to study the effect of FS-LΑSIK surgery on corneal biomechanics and corneal morphology from various aspects,especially to summarize the cases of iatrogenic keratectasia after laser corneal refractive surgery, to provide a more objective basis for ensuring the safety of surgery.
ACKNOWLEDGEMENTS
Conflicts of Interest: Li ZJ,None;Yang C,None;Liu SH,None;Guo J,None;Duan YH,None.
 International Journal of Ophthalmology2023年11期
International Journal of Ophthalmology2023年11期
- International Journal of Ophthalmology的其它文章
- Quantitative analysis of optic disc changes in school-age children with ametropia based on artificial intelligence
- Association analysis of Bcll with benign lymphoepithelial lesions of the lacrimal gland and glucocorticoids resistance
- In vitro protective effect of recombinant prominin-1 combined with microRNA-29b on N-methyl-D-aspartateinduced excitotoxicity in retinal ganglion cells
- Bioinformatics and in vitro study reveal the roles of microRNA-346 in high glucose-induced human retinal pigment epithelial cell damage
- Therapeutic effect of folic acid combined with decitabine on diabetic mice
- Comparison of visual performance with iTrace analyzer following femtosecond laser-assisted cataract surgery with bilateral implantation of two different trifocal intraocular lenses
