Prolonging dual antiplatelet therapy improves the long-term prognosis in patients with diabetes mellitus undergoing complex percutaneous coronary intervention
Jing-Jing XU ,Si-Da JIA ,Pei ZHU ,Ying SONG ,De-Shan YUAN ,Xue-Yan ZHAO ,Yi YAO,Lin JIANG,Jian-Xin LI,Yin ZHANG,Lei SONG,Run-Lin GAO,Ya-Ling HAN,Jin-Qing YUAN,✉
1.Department of Cardiology,National Clinical Research Center for Cardiovascular Diseases,National Center for Cardiovascular Diseases,State Key Laboratory of Cardiovascular Disease,Fuwai Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing,China;2.Department of Cardiology,General Hospital of Northern Theater Command,Shenyang,China
ABSTRACT OBJECTIVE To investigate the optimal duration of dual antiplatelet therapy (DAPT) in patients with diabetes mellitus (DM)requiring complex percutaneous coronary intervention (PCI).METHODS A total of 2403 patients with DM who underwent complex PCI from January to December 2013 were consecutively enrolled in this observational cohort study and divided according to DAPT duration into a standard group (11-13 months,n=689)and two prolonged groups (13-24 months,n=1133;> 24 months,n=581).RESULTS Baseline characteristics,angiographic findings,and complexity of PCI were comparable regardless of DAPT duration.The incidence of major adverse cardiac and cerebrovascular event was lower when DAPT was 13-24 months than when it was 11-13 months or > 24 months (4.6% vs.8.1% vs.6.0%,P=0.008),as was the incidence of all-cause death (1.9% vs.4.6% vs.2.2%,P=0.002) and cardiac death (1.0% vs.3.0% vs.1.2%,P=0.002).After adjustment for confounders,DAPT for 13-24 months was associated with a lower risk of major adverse cardiac and cerebrovascular event [hazard ratio (HR)=0.544,95% CI: 0.373-0.795] and all-cause death (HR=0.605,95% CI: 0.387-0.944).DAPT for > 24 months was associated with a lower risk of all-cause death (HR=0.681,95% CI: 0.493-0.942) and cardiac death (HR=0.620,95% CI: 0.403-0.952).The risk of major bleeding was not increased by prolonging DAPT to 13-24 months (HR=1.356,95% CI: 0.766-2.401) or > 24 months (HR=0.967,95% CI: 0.682-1.371).CONCLUSIONS For patients with DM undergoing complex PCI,prolonging DAPT might improve the long-term prognosis by reducing the risk of adverse ischemic events without increasing the bleeding risk.
Although dual antiplatelet therapy (DAPT)is already used routinely as secondary prevention for patients undergoing percutaneous coronary intervention (PCI),the optimal duration of DAPT continues to be debated.[1]Diabetes mellitus(DM) has long been considered a strong risk factor for ischemic events,and patients with coronary artery disease (CAD) complicated by DM have been shown to have a poor prognosis.[2]Patients with complex CAD,such as those with multi-vessel disease,chronic total occlusions,or multi-stent implantation,are deemed to be at high thrombotic risk.Given that prolonging DAPT has been confirmed to reduce the incidence of ischemic events,[3]it is possible that a longer period of DAPT might be of particular benefit in patients with DM undergoing complex PCI.However,this benefit may be offset by an increased risk of bleeding.Therefore,the current guidelines suggest that the duration of DAPT should be tailored to the risks of ischemia and bleeding.[4-6]
In a previous study,we found that prolonging DAPT from the standard duration of one year to more than one year reduced the incidences of all-cause death,cardiac death,and stent thrombosis during two years of followup in patients who underwent drug-eluting stents (DES)implantation without increasing the risk of bleeding.[7]However,for patients with DM who undergoing complex PCI,it is not clear whether prolonging DAPT will continue to be beneficial beyond two years.
METHODS
Study Population
A total of 10,724 patients underwent PCI at Fuwai Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing,China from January to December 2013.Patients with a confirmed diagnosis of DM and at least one high thrombotic risk technical aspects were selected for this study (the specific standards were shown in the part of definition).
The following exclusion criteria were applied: (1) bare metal stent implantation (n=64);(2) balloon angioplasty alone (n=237);(3) adverse cardiovascular,cerebrovascular,or bleeding events within one year after PCI(n=612);(4) duration of DAPT less than one year (n=157);and (5) single antiplatelet therapy (n=120).Finally,2403 patients were enrolled and according to DAPT duration divided into a standard group (11-13 months,n=689) and two prolonged groups (13-24 months,n=1133;>24 months,n=581) (Figure 1).
The study protocol was approved by the Institutional Review Board of Fuwai Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College (No.2021-1501) in Beijing,China and in accordance to the principles outlined in the Declaration of Helsinki.All patients provided written informed consent before starting the intervention.
Procedures and Medications
The PCI strategy and type of stent were selected at the discretion of the treating physician.Before the procedure,patients who were not on long-term aspirin and clopidogrel received an oral loading dose of aspirin 300 mg and clopidogrel 300 mg or 600 mg.During the procedure,all patients received unfractionated heparin (100 U/kg) with administration of glycoprotein IIb/IIIa inhibitors in accordance with the operator’s judgment.Other P2Y12inhibitors (e.g.,prasugrel and ticagrelor) were not routinely used in our center in 2013;during that time,only 16 patients (0.16%) received ticagrelor (at a loading dose of 180 mg).
Follow-up
All patients were evaluated during clinic visits or by telephone at one,three,and six months and one,two,and five years after the procedure.Patients were advised to return for coronary angiography if clinically indicated by symptoms or if showing signs of myocardial ischemia.
Definitions
DM was diagnosed in accordance with the criteria in the 2020 guideline for prevention and treatment of type 2 DM in China,[8]namely,a definite history of DM or symptoms of DM accompanied by a fasting blood glucose level ≥ 7.0 mmol/L or the glycated hemoglobin A1c ≥6.5%.
The high thrombotic risk technical aspects refers to the risk criteria for extended treatment with a second antithrombotic agent in the 2020 European Society of Cardiology guidelines for the management of acute coronary syndrome (ACS) in patients presenting without persistent ST-segment elevation.[9]These criteria are as follows: at least three stents implanted,at least three lesions treated,total stent length > 60 mm,and a history of complex revascularization (left main,bifurcation stenting with more than two stents implanted,or chronic total occlusion).
The duration of DAPT was defined as the interval between the date of PCI and cessation of DAPT.Patients were divided into two groups according to whether they received a standard duration of DAPT (11-13 months,n=689) or a prolonged duration of DAPT (> 13 months,n=1714).The prolonged DAPT group was divided further into two subgroups according to whether DAPT was administered for 13-24 months (n=1133) or > 24 months (n=581) (Figure 1).Myocardial infarction (MI) was defined according to the third universal definition[10]and bleeding according to the definition of the Bleeding Academic Research Consortium.[11]A new-generation DES was defined as a second-generation DES or a biodegradable polymer DES.
Endpoints
The primary endpoint was major adverse cardiac and cerebrovascular event (MACCE),which is a composite of all-cause death,MI,and stroke,at the five-year followup.The secondary endpoints were the individual components of MACCE and bleeding.All endpoint events were adjudicated by two independent cardiologists,and disagreement was resolved by consensus.
Statistical Analysis
Continuous variables were compared by the one-way analysis of variance as appropriate.Categorical variables were compared using the Bonferroni method in aZ-test between columns,and the overallP-value was calculated by the Pearson’s chi-squared test.Continuous variables are shown as mean ± SD and categorical variables as counts (percentages).Survival curves were calculated using the Kaplan-Meier estimates and compared using the log-rank test.We took the standard DAPT as the reference with adjustment for age,sex,body mass index,hypertension,hyperlipidemia,previous PCI,and SYNTAX score before PCI for the multivariable Cox regression models.The results of Cox regression analysis are expressed as hazard ratio (HR) with 95% CI.Subgroup analyses were performed using factors associated with a high risk of ischemia and a high risk of bleeding (i.e.,age,sex,history of smoking,previous PCI,previous MI,ACS,cardiac function,and renal function).Interactions between duration of DAPT and the selected factors were analyzed according to outcomes.
All statistical analyses were conducted with SPSS 20.0(SPSS Inc.,IBM,Armonk,NY,USA).Two-tailedP-value< 0.05 were considered statistically significant.
RESULTS
Baseline Characteristics
In total,689/2403 patients (28.7%) received standard DAPT and 1714/2403 patients (71.3%) received prolonged DAPT.The patient characteristics at baseline are shown in Table 1.The background and angiographic characteristics were similar among the three groups,except for a lower incidence of previous coronary artery bypass grafting in the group that received DAPT for 13-24 months,a higher fasting blood glucose level in the group that received DAPT for > 24 months,and a higher incidence of unstable angina in the group that received DAPT for 11-13 months.
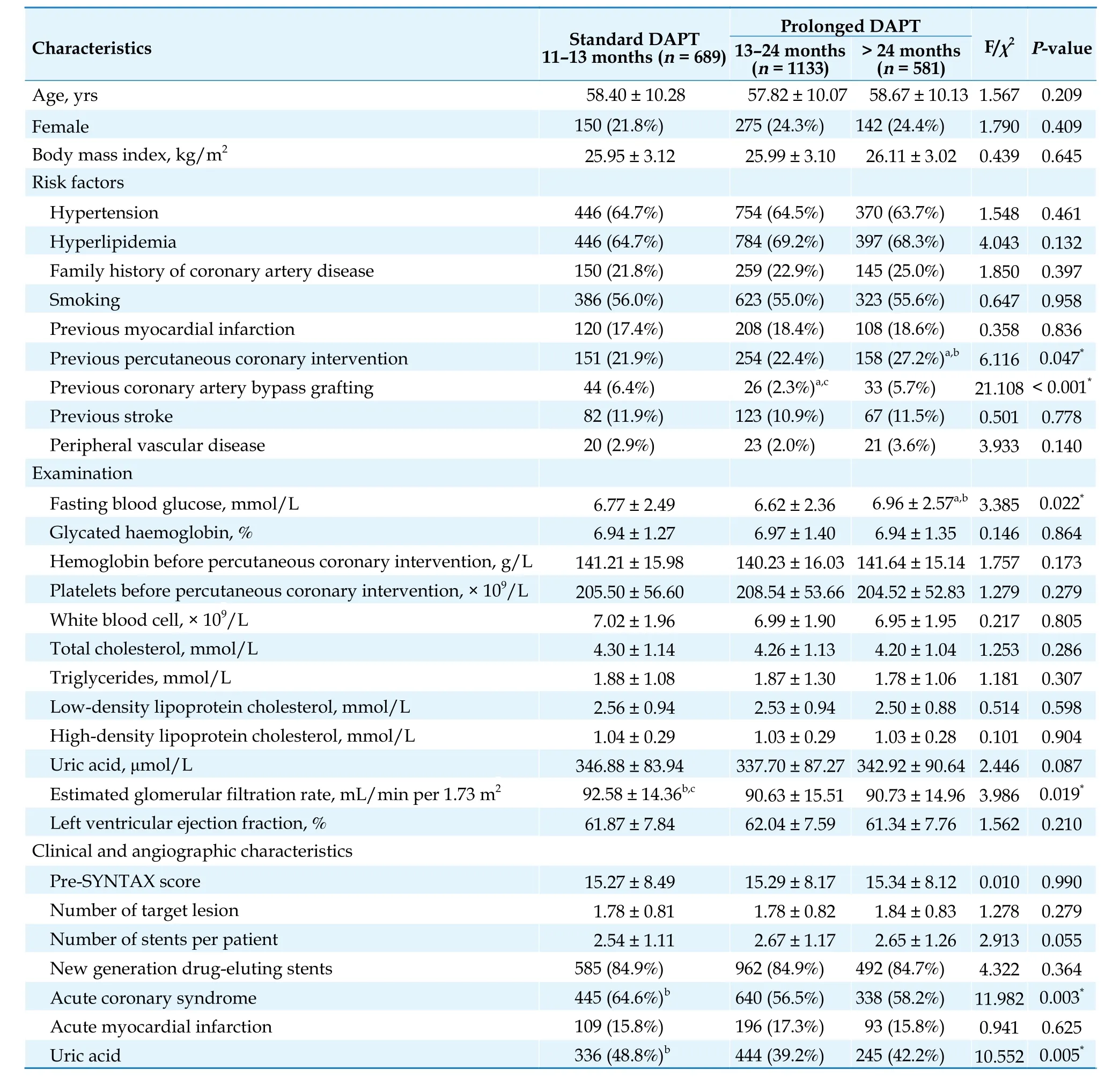
Table 1 Baseline characteristics in the three DAPT duration groups.
High Thrombotic Risk Technical Aspects
The high thrombotic risk technical aspects are shown according to duration of DAPT in Figure 2.There was no significant difference in the type of complex PCI technique used between the three DAPT groups.
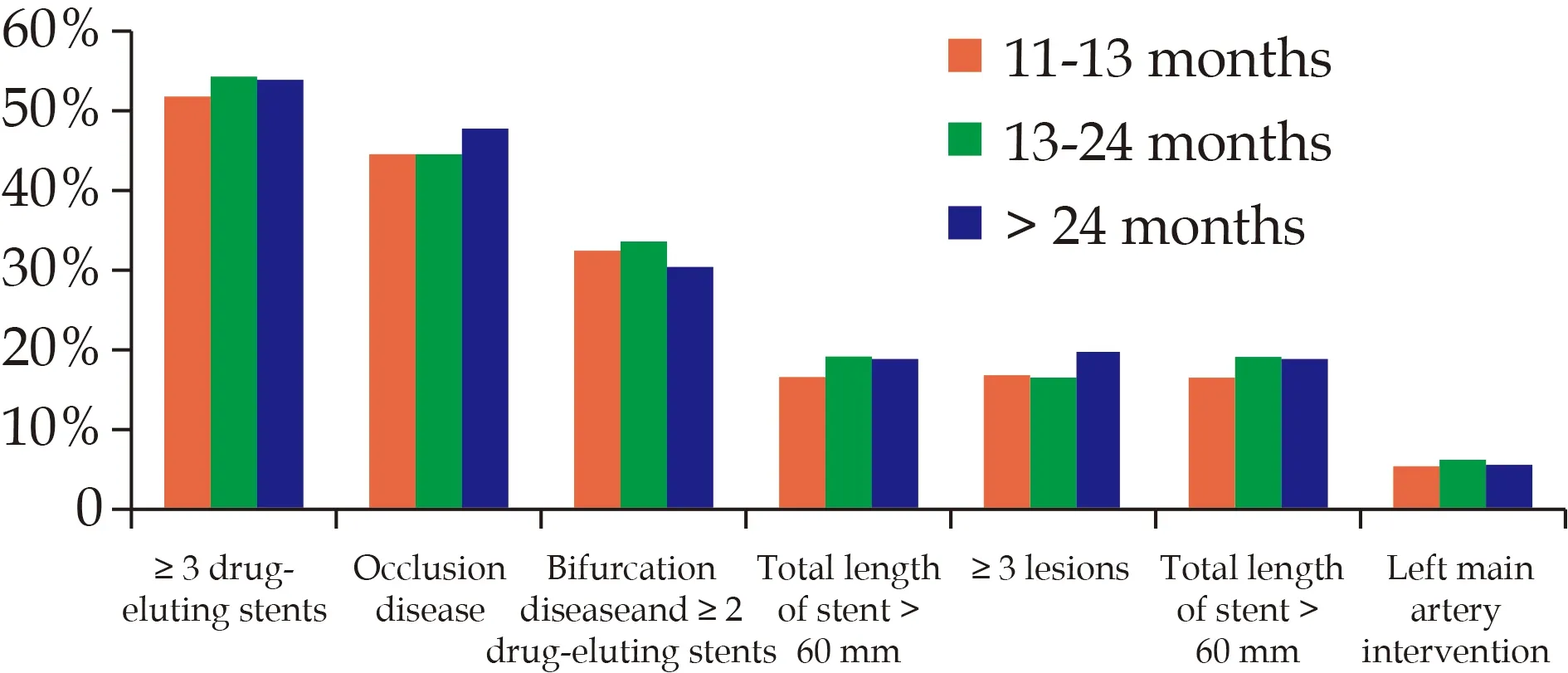
Figure 2 High thrombotic risk in technical aspects according to duration of DAPT.The proportions of different coronary intervention technical aspects with high thrombotic risk are shown for the three DAPT durations.DAPT: dual antiplatelet therapy.
Five-year Outcomes
During five years of follow-up,the incidences of MACCE,all-cause death,and cardiac death were significantly lower in the groups with prolonged DAPT than in the group with standard DAPT.The incidence of MACCE was significantly lower when DAPT was 13-24 months than when it was 11-13 months or > 24 months (4.6%vs.8.1%vs.6.0%,P=0.008),as was the incidence of allcause death (1.9%vs.4.6%vs.2.2%,P=0.002) and cardiac death (1.0%vs.3.0%vs.1.2%,P=0.002).There were no between-group differences in the incidence of stroke or bleeding (Table 2).Kaplan-Meier estimates showed a similar trend (Figure 3).

Table 2 Five-year outcomes according to DAPT duration.
Multivariable Analysis
Cox multivariable regression analysis confirmed that DAPT for 13-24 months was associated with a lower risk of MACCE (HR=0.544,95% CI: 0.373-0.795) and all-cause death (HR=0.605,95% CI: 0.387-0.944).DAPT for > 24 months was associated with a lower risk of all-cause death (HR=0.681,95% CI: 0.493-0.942) and a lower risk of cardiac death (HR=0.620,95% CI: 0.403-0.952) (Table 3).
根据各自意愿,在特定领域就某个项目开展合作。实习有优势的偏重实习方面合作,场地有优势的利用场地办学。这种合作一事一议,方式灵活,双方优势互补,互利互惠,就某个项目签订合作协议,展开长期或短期合作,合作任务完成后根据情况确定今后合作意向。

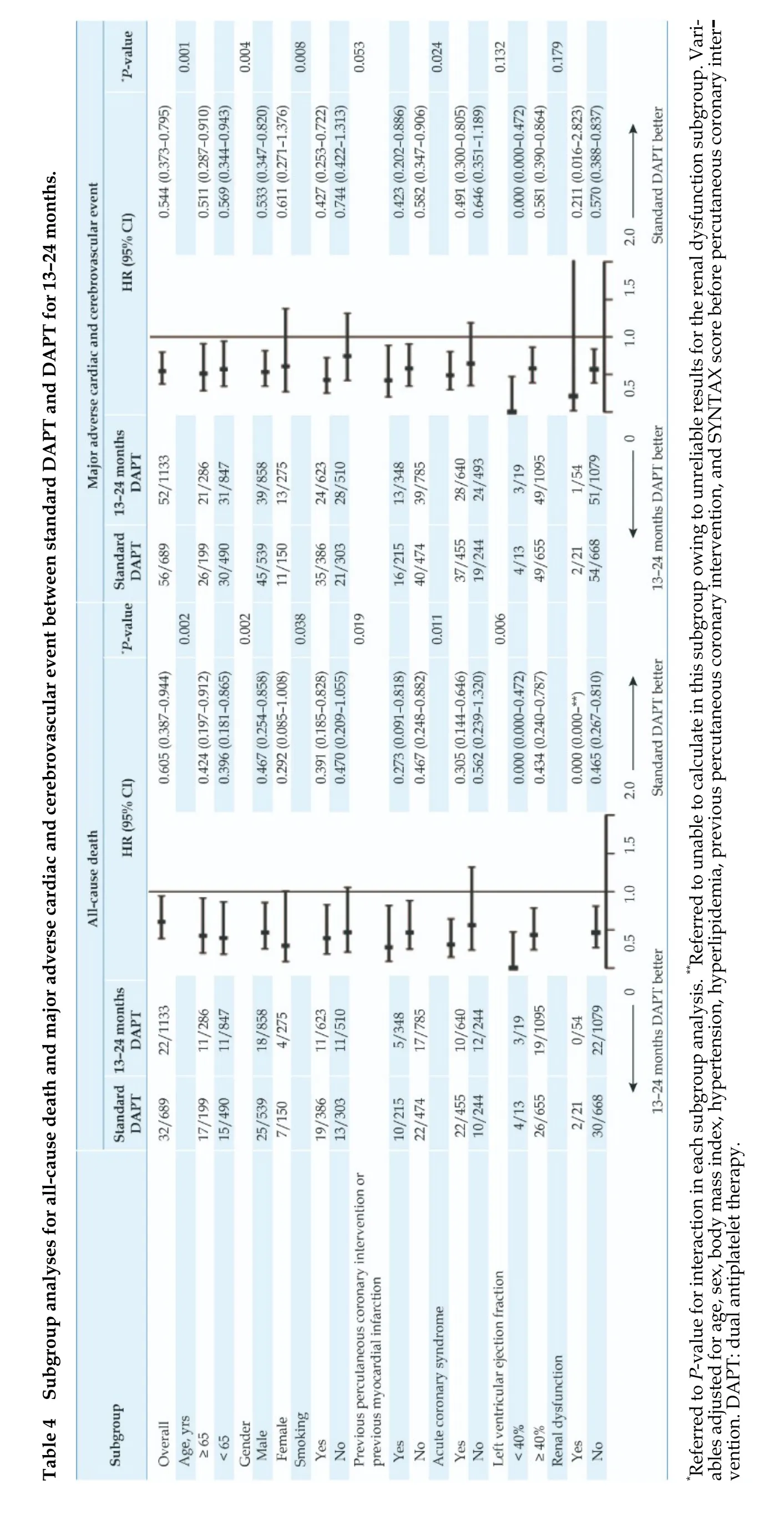
Subgroup Analysis
We performed a subgroup analysis for all-cause death and MACCE between a standard duration of DAPT and DAPT for 13-24 months to evaluate patients with risk factors for ischemia or bleeding.Variables in this subgroup analysis included age,sex,smoking history,previous PCI,history of MI,ACS,cardiac dysfunction(left ventricular ejection fraction < 40%),and renal dysfunction (estimated glomerular filtration rate < 60 mL/min per 1.73 m2).DAPT for 13-24 months reduced the risks of all-cause death and MACCE in patients aged ≥65 years and < 65 years,in men,in patients with a smoking history,and in patients with ACS.Furthermore,DAPT for 13-24 months reduced the risk of all-cause death regardless of whether there was a history of PCI or MI and whether or not cardiac dysfunction was present(Table 4).
DISCUSSION
The objective of this study was to determine the appropriate duration of DAPT for patients at high risk of ischemic events,specifically patients with DM undergoing complex PCI.The study had four major findings.Firstly,a prolonged duration of DAPT is common in patients at high ischemic risk undergoing PCI with DES in China.Secondly,a prolonged duration of DAPT can reduce the incidence of adverse cardiovascular events in patients at high ischemic risk,such as those with DM and those undergoing complex coronary interventions.Thirdly,prolonged DAPT does not increase the risk of bleeding.Fourthly,patients at high ischemic risk benefit even more when combined with risk enhancers for ischemic events.
DM and Complex Coronary Intervention Increase Ischemic Risk
DM is a major risk factor for coronary heart disease,which makes patients vulnerable to atherosclerosis because of damage to the vascular endothelium and vascular dysfunction caused by metabolic abnormalities in blood glucose.Furthermore,high platelet reactivity and hypercoagulability in patients with DM cause a significant increase in the risk of thrombosis and ischemic events.[12]Complex coronary interventions could also increase the risk of thrombosis.Although advances in equipment and techniques have enabled interventional cardiologists to revascularize extremely difficult coronary lesions,[13]there is a need for increased awareness of the ischemic risk in these patients.
Selection of DAPT Duration and Recommendations in the Guidelines
DAPT benefits patients undergoing PCI by reducing the incidence of stent thrombosis and strengthening secondary prevention of coronary heart disease.[14]The United States and European guidelines recommend 12 months of DAPT for patients after DES implantation with adjustment of the duration according to the risk of ischemic events and bleeding.[15,16]The guidelines recommend appropriate prolongation of DAPT if patients have complex CAD combined with risk factors for ischemia.[4,17]
In the present study,28.7% of patients received standard DAPT and 71.3% of patients received prolonged DAPT.The high proportion of patients on prolonged DAPT reflects cardiologists’ preference for extending this therapy in patients with a high ischemic risk.
Benefits of Prolonging DAPT
The benefits of prolonging DAPT continue to be controversial.The TIMI 38 Coronary Stent Registry found a similar rate of recurrence of ischemic events between patients who continued DAPT and those who discontinued it (P=0.74 for cardiovascular death/MI/stroke,P=0.72 for definite or probable stent thrombosis).[18]Moreover,the DAPT Study indicated that continued treatment with thienopyridine could reduce the rates of stent thrombosis (0.4%vs.1.4%;HR=0.29,95% CI: 0.17-0.48,P< 0.001) and MACCE (4.3%vs.5.9%;HR=0.71,95% CI:0.59-0.85,P< 0.001).[3]However,these studies did not strictly define the risk of ischemia.
Prolonging DAPT Does Not Increase the Bleeding Risk
The biggest concern when considering prolongation of DAPT is the increased bleeding risk,especially in Chinese patients,who are considered to be at a relatively higher risk of bleeding.[19]In the present study,we found no significant difference in the risk of bleeding among the three DAPT groups.This result is in line with our previous finding that prolonging the duration of DAPT in patients undergoing PCI and patients with ACS did not significantly increase their risk of bleeding,including all bleeding events and major bleeding events,[7,20]and confirms the safety of prolonging DAPT.
More Benefits for Patients Combined with Risk Enhancers
Subgroup analysis that included risk enhancers for ischemia or bleeding showed that prolonging DAPT to 13-24 months can reduce the risk of all-cause death and MACCE in patients aged ≥ 65 years and < 65 years,in men,in patients with a smoking history,and in patients with ACS.DAPT for 13-24 months can also reduce the risk of all-cause death irrespective of whether there is a history of PCI or MI and whether or not cardiac dysfunction is present.These results indicate that appropriately prolonging the duration of DAPT would bring more benefits if combined with risk enhancers in patients with a high ischemic risk.The more risk factors for ischemia that are combined,the more likely patients are to benefit from prolongation of DAPT.
LIMITATIONS
There are several limitations that must be noted.Firstly,being an observational study,evaluation of medication efficacy was limited.Furthermore,the study had a non-randomized design and may have included unrecognized confounders that would preclude definitive conclusions.Secondly,only patients who could tolerate prolonged DAPT were enrolled,which may have introduced selection bias.Last but not least,information on how DAPT was discontinued was not available.
CONCLUSIONS
Appropriate prolongation of DAPT could improve the long-term prognosis in patients with DM undergoing complex PCI by reducing the risk of adverse cardiovascular ischemic events without increasing the risk of bleeding.
ACKNOWLEDGMENTS
This study was supported by the National High Level Hospital Clinical Research Fund (2022-GSP-QN-1),the Young Talent Program of the Academician Fund (YS-20 22-002),the National Key Research and Development Program of China (2016YFC130130 &2016YFC1301301),and the National Clinical Research Center for Cardiovascular Diseases,Fuwai Hospital,Chinese Academy of Medical Sciences (NCRC2020013).All authors had no conflicts of interest to disclose.The authors are grateful to the staff in the Department of Cardiology and Catheterization Laboratory,Fuwai Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing,China for their research contributions.
 Journal of Geriatric Cardiology2023年8期
Journal of Geriatric Cardiology2023年8期
- Journal of Geriatric Cardiology的其它文章
- Prognostic value of hematological parameters in older adult patients with acute coronary syndrome undergoing coronary intervention: a single centre prospective study
- Age-related outcomes in patients with cardiogenic shock stratified by etiology
- Development and validation of a score predicting mortality for older patients with mitral regurgitation
- Current and recent cigarette smoking in relation to cardiovascular and non-cardiovascular mortality in an elderly male Chinese population
- Feasibility of emergent transcatheter aortic valve replacement sequentially followed by cardiac computed tomography angiography: experience from the procedure
- The first experience of multi-gripper robot assisted percutaneous coronary intervention in complex coronary lesions
