Development and validation of a score predicting mortality for older patients with mitral regurgitation
De-Jing FENG,Yun-Qing YE,Zhe LI,Bin ZHANG,Qing-Rong LIU,Wei-Wei WANG,Zhen-Yan ZHAO,Zheng ZHOU,Qing-Hao ZHAO,Zi-Kai YU,Hai-Tong ZHANG,Zhen-Ya DUAN,Bin-Cheng WANG,Jun-Xing LV,Shuai GUO,Run-Lin GAO,Hai-Yan XU,Yong-Jian WU,on behalf of the China-DVD and China-VHD study investigators
Department of Cardiology,Fuwai Hospital,National Center for Cardiovascular Disease,Chinese Academy of Medical Science and Peking Union Medical College,Beijing,China
ABSTRACT OBJECTIVE To develop and validate a user-friendly risk score for older mitral regurgitation (MR) patients,referred to as the Elder-MR score.METHODS The China Senile Valvular Heart Disease (China-DVD) Cohort Study functioned as the development cohort,while the China Valvular Heart Disease (China-VHD) Study was employed for external validation.We included patients aged 60 years and above receiving medical treatment for moderate or severe MR (2274 patients in the development cohort and 1929 patients in the validation cohort).Candidate predictors were chosen using Cox’s proportional hazards model and stepwise selection with Akaike’s information criterion.RESULTS Eight predictors were identified: age ≥ 75 years,body mass index < 20 kg/m2,NYHA class III/IV,secondary MR,anemia,estimated glomerular filtration rate < 60 mL/min per 1.73 m2,albumin < 35 g/L,and left ventricular ejection fraction < 60%.The model displayed satisfactory performance in predicting one-year mortality in both the development cohort (C-statistic=0.73,95%CI: 0.69-0.77,Brier score=0.06) and the validation cohort (C-statistic=0.73,95% CI: 0.68-0.78,Brier score=0.06).The Elder-MR score ranges from 0 to 15 points.At a one-year follow-up,each point increase in the Elder-MR score represents a 1.27-fold risk of death(HR=1.27,95% CI: 1.21-1.34,P < 0.001) in the development cohort and a 1.24-fold risk of death (HR=1.24,95% CI: 1.17-1.30,P <0.001) in the validation cohort.Compared to EuroSCORE II,the Elder-MR score demonstrated superior predictive accuracy for oneyear mortality in the validation cohort (C-statistic=0.71 vs.0.70,net reclassification improvement=0.320,P < 0.01;integrated discrimination improvement=0.029,P < 0.01).CONCLUSIONS The Elder-MR score may serve as an effective risk stratification tool to assist clinical decision-making in older MR patients.
Mitral regurgitation (MR) is one of the most common valve diseases,with a prevalence of 6.5% in populations aged 65 years and above,imposing a considerable global burden on healthcare systems.[1,2]In recent years,transcatheter treatments such as transcatheter edge-to-edge repair (TEER)and transcatheter mitral valve replacement have emerged as alternative approaches to surgery for older MR patients and those with high surgical risk.Consequently,an increasing number of older MR patients are expected to receive these treatments in the near future.[3,4]Risk stratification is essential for optimizing treatment strategies and avoiding futile interventions,although it is more challenging for older patients who require multiple evaluations,such as frailty and nutritional status assessments.[5-7]Predicting outcomes in MR patients is difficult due to the heterogeneity in pathophysiology across various etiologies,such as primary MR (PMR) and secondary MR (SMR).While several attempts have been made recently to identify high-risk MR patients,their applications have been limited to specific subgroups,such as patients with MR due to flail leaflet or those who received TEER therapy.[8,9]To date,no dedicated score exists for risk-stratifying older MR patients across different etiologies.This study aimed to derive and validate a userfriendly risk score for predicting mortality in older MR patients based on two large cohorts,thereby facilitating clinical decision-making.
METHODS
Development Cohort
Patients were recruited from the China Senile Valvular Heart Disease (China-DVD) Cohort Study (Clinical-Trials.gov Identifier: NCT02865798),a nationwide,multicenter,prospective cohort study that included older patients (≥ 60 years) diagnosed with significant valvular heart disease (VHD) through echocardiography according to the 2014 American Heart Association/American Colege of Cardiology guidelines.[10]Between September and December 2018,a total of 8929 patients aged ≥60 years with VHD were consecutively enrolled from 69 large academic hospitals across 28 provinces in China.All patients were followed for one year.Follow-up data were collected from patient visits,medical records,and telephone interviews.The China-DVD study’s detailed information regarding patient selection,study organization,and follow-up has been previously described.[11]The study protocol adhered to the ethical guidelines of the 1975 Declaration of Helsinki,as reflected in the prior approval by the National Center for Cardiovascular Diseases of China’s Human Research Committee (No.2016-7 77).Written informed consent was obtained from all eligible participants.This study followed the TRIPOD (Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis) statement for reporting.
This study included patients diagnosed with significant MR (moderate or severe).The following patients were excluded: (1) patients with combined more than mild stenosis of any valves;(2) patients with more than mild aortic regurgitation or pulmonary regurgitation;(3) patients with more than mild primary tricuspid regurgitation;(4) patients with a diagnosis of endocarditis or cancer;(5)patients who received surgery at enrollment;and (6) patients with incomplete data.Patients with concomitant moderate or severe secondary tricuspid regurgitation were not excluded since it is often secondary to MR and thus is an essential indicator for the progression of MR.
Validation Cohort
Data from the China Valvular Heart Disease (China-VHD) Study (ClinicalTrials.gov Identifier: NCT034848 06) were utilized to externally validate the risk model.The China-VHD study was a nationwide,multicenter,prospective cohort study involving adult patients (≥ 18 years) diagnosed with significant VHD through echocardiography.Between April and June 2018,13,917 consecutive adult patients were enrolled across 46 large academic hospitals in China.Patients in the China-VHD study were followed for two years.In this study,we applied the same inclusion and exclusion criteria as those used in the China-DVD study,focusing on patients aged 60 years and older.
Data Collection and Variables
The China-DVD and China-VHD studies collected comprehensive data with standard definitions,encompassing patient demographics,comorbidities,presentations,investigations,etiology,interventions,complications,and outcomes.A standardized echocardiography protocol was provided to operators and reporters at participating sites.Patient echocardiography videos were randomly sampled and blindly reviewed at the core echocardiography lab to ensure quality.VHD etiologies were adjudicated based on clinical context,echocardiography,computed tomography,and surgical findings (when available) at each participating site.
The China-DVD Executive Committee selected 23 variables as candidate predictors,based on their availability,potential prognostic significance,and clinical relevance,as displayed in Table 1.To generate a user-friendly risk score for clinical practice,we dichotomized continuous variables according to clinically relevant cut-off points,such as body mass index (BMI) < 20 kg/m2,anemia (defined as hemoglobin < 120 g/L in males and < 110 g/L in females,respectively),albumin < 35 g/L,and estimated glomerular filtration rate < 60 mL/min per 1.73 m2(calculated using the Modification of Diet in Renal Disease equations).[12]The cut-off values of echocardiographic variables were identified based on their associations with PMR patients reported in previous studies,such as left atrial size ≥ 55 mm,pulmonary artery systolic pressure ≥ 50 mmHg,and left ventricular ejection fraction(LVEF) < 60%.[8]
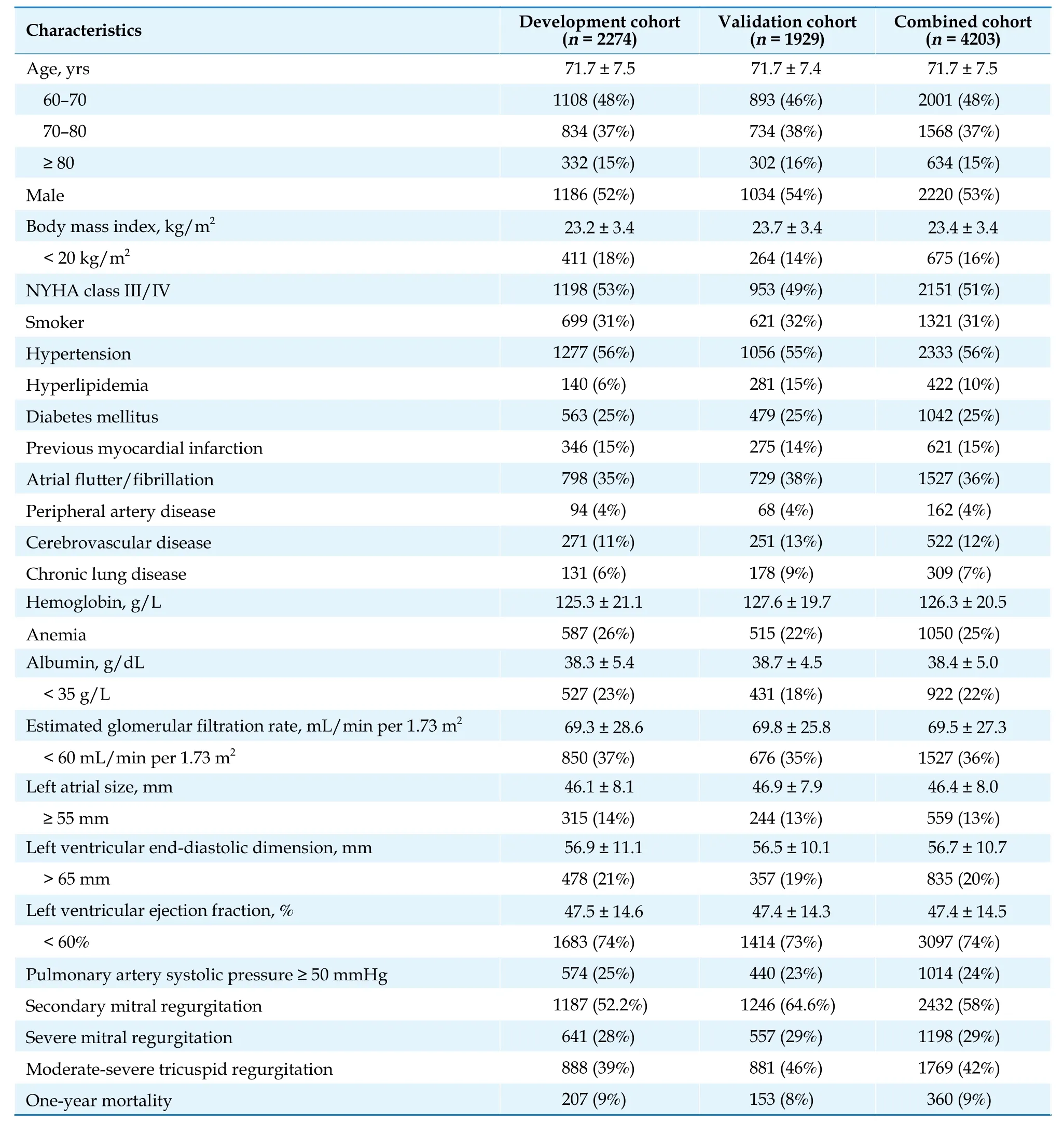
Table 1 Baseline characteristics of the development cohort and the validation cohort.
Study Endpoints
The primary endpoint was one-year all-cause mortality.
Statistical Analysis
Cox’s proportional hazards models were employed to investigate the association between potential predictors and one-year survival.Competing risk analysis was not applied due to the relatively small number of patients under medical management who underwent surgery during follow-up (development cohort: 42 patients at one year,validation cohort: 135 patients at two years).Variables in the final model were selected through a combination of forward and backward steps using Akaike’s information criterion.Proportional hazard assumptions were evaluated with scaled Schoenfeld residuals.The weights of each variable in the final model were calculated based on their regression coefficients,generating the final Elder-MR score system.The Elder-MR score was derived as the sum of these weights for individuals.Patients were then classified into three risk groups by tertiles:low-risk (≤ 25thpercentile),moderate-risk (25th-75thpercentile),and high-risk (≥ 75thpercentile).Score discrimination was assessed using Harrell’s C-statistic,ranging from 0.5,representing no discrimination,to 1 for perfect discrimination.Calibration was visually evaluated by a calibration plot,which depicted the predicted risk versus the observed risk of events by quantiles.The Brier score assessed the model’s overall performance,ranging from 0 for a perfect model to 0.25 for a noninformative model with a 50% outcome incidence.AP-value < 0.05 was considered statistically significant.All analyses were performed using R statistical software 4.1.3 (http://www.r-project.org).
RESULTS
Baseline Characteristics
In total,we included 2274 patients over 60 years receiving medical treatment in the development cohort and 1929 patients in the validation cohort.The baseline characteristics of these two cohorts are displayed in Table 1.The mean age of patients was 71.7 ± 7.5 years in the development cohort and 71.7 ± 7.4 years in the validation cohort.Males comprised 52.2% of the development cohort and 53.6% of the validation cohort.In the development cohort,52.2% of patients had NYHA class III/IV,similar to the 47.6% of patients in the validation cohort.Severe MR was present in 28.2% of the development cohort and 28.9% of the validation cohort.Patients with SMR accounted for 52.2% in the development cohort and 64.6% in the validation cohort.At a one-year follow-up,207 deaths (9.1%) occurred in the development cohort,while 154 deaths (8.0%) occurred in the validation cohort.
Model Development
Eight predictors with clinical importance were selected through stepwise selection: age ≥ 75 years,BMI < 20 kg/m2,NYHA class III/IV,SMR,anemia,estimated glomerular filtration rate < 60 mL/min per 1.73 m2,albumin < 35 g/L,and LVEF < 60%.The model coefficients and hazards ratio (HR) are presented in Table 2.The model demonstrated adequate discriminative ability with a C-statistic of 0.73 (95% CI: 0.69-0.77).The calibration plot showed good agreement between predicted and observed mortality (Figure 1A).The overall performance was confirmed with a Brier score of 0.06.The model maintained its performance across different etiologies of MR(Table 3).

Figure 1 The performance of the Elder-MR score in the development cohort.(A): Calibration plot;and (B): one-year cumulative risk of patients categorized by the Elder-MR score.

Table 2 Development of the Elder-MR score.

Table 3 The performance of the Elder-MR score in predicting one-year mortality.
The Elder-MR score was constructed based on the variables’ coefficients as their weights.Ultimately,the Elder-MR score ranges from 0 to 15 points.The median Elder-MR score in the development cohort was 7 (25th-75thpercentile: 4-9).Every 1-point increase in the Elder-MR score was associated with a 1.27-fold risk of death(adjusted HR=1.27,95% CI: 1.21-1.34).When patients were classified into three risk groups,those in the moderaterisk group (5-9 points) and the high-risk group (10-15 points) were associated with a significantly higher risk of death compared to patients in the low-risk group (2.7%vs.9%vs.20%,Ptrend< 0.001;moderate-risk: adjusted HR=3.48,95% CI: 2.08-5.80;high-risk: adjusted HR=8.67,95%CI: 5.14-14.58) (Figure 1B).
Model Validation
Upon external validation,the model’s C-statistics were 0.73 (95% CI: 0.68-0.78) in the validation cohort,and the Brier score was 0.06 (Table 3).The predicted risk of death versus the observed risk showed good agreement in the validation cohort (Figure 2A).Measures of the model’s performance were similar across different etiologies of MR (Table 3).The median Elder-MR score in the validation cohort was 7 (25th-75thpercentile: 4-9).The Elder-MR score was significantly associated with the one-year mortality (adjusted HR=1.24,95% CI: 1.17-1.30,P< 0.001) of patients under medical management.When patients were classified into risk groups,those in the moderate-risk group and the high-risk group had a significantly higher risk of one-year mortality (2.9%vs.6.8%vs.17.7%,Ptrend< 0.001;moderate-risk: adjusted HR=2.46,95% CI: 1.46-4.12;high-risk: adjusted HR=7.24,95%CI: 4.30-12.20) (Figure 2B).

Figure 2 The performance of the Elder-MR score in the validation cohort. (A): Calibration plot;and (B): one-year cumulative risk of patients categorized by the Elder-MR score.
When the Elder-MR score was fitted into a logistic regression model as the sole predictor of mortality,it showed adequate performance in predicting one-year mortality (C-statistic=0.71,95% CI: 0.67-0.75,Brier score=0.06).Compared to EuroSCORE II,the Elder-MR score demonstrated better predictive accuracy for one-year mortality (C-statistic=0.71vs.0.70,Brier score=0.06vs.0.07,net reclassification improvement=0.320,P< 0.01;integrated discrimination improvement=0.029,P< 0.01)(supplemental material,Table 1S).
Predictive Accuracy in the Combined Cohort
Given the similarity in baseline characteristics and model performance between the two cohorts,we combined the development and validation cohorts to increase the number of events further and facilitate subgroup analyses (Table 1).In the combined cohort,1458 patients were aged above 75 years,and each point increase in the Elder-MR score was associated with a 1.25-fold risk of death(adjusted HR=1.25,95% CI: 1.18-1.32).Among the 3005 patients with moderate PMR or SMR,a per-point increase in the Elder-MR score was associated with a 1.27-fold risk of death (adjusted HR=1.27,95% CI: 1.22-1.33).The significant predictive values of the Elder-MR score were also seen across different subgroups,such as sex,etiology,LVEF,or NYHA class (Figure 3).The baseline characteristics of different subgroups are also summarized(supplemental material,Table 2S-Table 7S).

Figure 3 Independent association of the Elder-MR score with one-year mortality in selected sub-groups in the combined cohort (the Elder-MR score was demonstrated to be independently associated with death across various subgroups. *Refers to adjust to age and sex.NYHA: New York Heart Association.
DISCUSSION
In this study,we developed and validated a simple score based on routine clinical tests to predict mortality for older MR patients.The Elder-MR score demonstrated good performance in both the development and validation cohorts for predicting one-year mortality,irrespective of the etiologies of MR.Compared with EuroSCORE II,the Elder-MR score exhibited better predictive accuracy for one-year mortality in the validation cohort.Therefore,it may serve as a practical risk stratification tool to assist clinical decision-making.
Risk prediction for older MR patients is challenging.Surgical risk scores,such as the Society of Thoracic Surgeons score and EuroSCORE II,have shown limited accuracy in predicting risks for older patients or those receiving transcatheter treatments.[9,13,14]The underperformance of surgical scores in these patients has been attributed to the lack of assessments like frailty or nutritional status,which are increasingly recognized as essential for risk evaluations in older patients.[15,16]The Mitral Regurgitation International Database (MIDA) score,primarily based on echocardiographic values,was developed to assess mortality rates in patients with PMR due to flail leaflet and demonstrated good performance in predicting both one-year and long-term mortality.[8]However,patients with SMR may have a different risk profile compared to those with PMR due to the distinct pathophysiology and uncertain efficacy of intervention therapies.Kavsur,et al.[17]validated the MIDA score in patients with MR undergoing transcatheter mitral valve repair and found that the MIDA score remained a significant predictor of two-year mortality in both SMR and PMR patients.However,they considered patients as secondary when MR resulted from mixed causes,which means SMR patients in their study may also have organic damages and thus may have a risk profile close to patients with PMR.Therefore,the predictive accuracy of the MIDA score in patients with SMR still needs validation.Recently,the MitraScore was proposed to predict mortality for patients receiving TEER.This score consists of eight predictors,including details about medical treatment (high diuretic dose and no therapy with renin-angiotensin system inhibitors) and exhibited good performance in predicting two-year mortality (C-statistic=0.70 in the development cohort).[9]However,when externally validated,the Mitra-Score demonstrated only moderate performance (C-statistic=0.66 in the validation cohort).Spieker,et al.[18]validated the predictive accuracy of the MitraScore in patients undergoing mitral TEER in their registry.They found the performance of the MitraScore in predicting one-year mortality to be only mild (C-statistic=0.61),and it further decreased in patients with SMR (C-statistic=0.59).Therefore,a simple risk score applicable to all older MR patients with satisfactory performance is still lacking.
In this study,we developed the Elder-MR score to predict mortality based on a real-world cohort including consecutive elderly MR patients,regardless of their etiologies.The Elder-MR score showed good performance in predicting one-year mortality in the development cohort.When analyzed in SMR and PMR patients separately,the score maintained satisfactory predictive accuracy.This is especially important since no risk scores have been demonstrated to have accurate predictive accuracy in both SMR and PMR patients.Previous studies have confirmed that SMR patients have a worse risk profile than PMR patients.[19,20]Several echocardiographic variables,such as left atrial size and pulmonary artery systolic pressure,were found to have a strong association with PMR patients previously but were excluded from the current analysis,likely due to the different pathophysiology of PMR and SMR patients.[8]The Elder-MR score demonstrated satisfactory performance in both SMR and PMR patients because most predictors included in the Elder-MR score are common risk factors associated with adverse outcomes.For example,predictors like anemia,low BMI,and albumin are highly relevant to patients’ frailty status and nutritional conditions.[21-23]Other variables like age ≥75 years,NYHA class III/IV,and impaired renal function are also essential variables representing worse prognoses in SMR and PMR patients.Another strength of our study was that when the Elder-MR score was externally validated in an independent cohort,it maintained good predictive accuracy in all MR patients and patients across different etiologies.Compared to the EuroSCORE II system,the Elder-MR score demonstrated better predictive accuracy (net reclassification improvement for one-year mortality was 0.32,P< 0.01;integrated discrimination improvement=0.029,P< 0.01).
Variables in the Elder-MR score can be easily obtained from patients’ medical records (age,BMI,and symptoms) and routine clinical tests such as laboratory tests and echocardiographic values.This enables the Elder-MR score to have advantages in clinical practice not only for surgeons but also for physicians,as the EuroSCORE II system or the Society of Thoracic Surgeons score are all webbased score calculators,which are not routinely performed when surgery is not considered.The Elder-MR score may allow heart teams to accurately predict the risk of death in individuals in routine clinical practice.For patients under medical treatment,the score may indicate which patient needs early intervention or closer followup to optimize medical treatment and prevent mortality.The Elder-MR score may also provide helpful information for patient counseling.Patients and their families may be informed of their predicted one-year mortality based on a national risk-adjusted analysis of real-world patients with a risk profile comparable to theirs.For patients receiving interventions like surgery or transcatheter treatments,the Elder-MR score may have a role in adjudicating futility since several predictors are related to frailty and nutritional status,especially for those who fall into the high-risk category.However,no clinical decision-making should arbitrarily rely on a single score and instead be based on an integrated clinical approach.
LIMITATIONS
Several limitations exist in this study.Firstly,since local investigators reported the etiologies of patients in the China-DVD study and the China-VHD study,there may be some bias impacting the accuracy of our results.However,all participating centers in these two studies are large volume centers with well-trained investigators.A standardized definition of different etiologies of VHD and echocardiography protocol was provided to operators and reporters at participating sites.The core echocardiography lab randomly sampled and reviewed patients’ echocardiography videos to ensure their quality,reducing this bias.Secondly,because all participating hospitals are large academic hospitals,patients from these hospitals cannot represent the entire MR population,leading to selection bias.Last but not least,many emerging predictors related to frailty or advanced echo parameters are not included in the Elder-MR score due to the lack of these variables in the cohort.Future studies may incorporate emerging predictors related to frailty or advanced echo parameters into the Elder-MR score or build new models using these variables to better identify high-risk older MR patients.
CONCLUSIONS
The Elder-MR score,comprising eight predictors from routine clinical tests,demonstrated strong performance in predicting one-year mortality in both the development and validation cohorts.In comparison to EuroSCORE II,the Elder-MR score exhibited superior predictive accuracy.This score may serve as a valuable tool for risk assessment and clinical decision-making for older MR patients,in addition to traditional surgical risk scores.Nonetheless,prospective validation of this score in broader populations remains necessary.
ACKNOWLEDGMENTS
This study was supported by the National Key R&D Program of China (No.2020YFC2008100).All authors had no conflicts of interest to disclose.The authors would like to thank all the staff members involved in the China-VHD study and the China-DVD study.
 Journal of Geriatric Cardiology2023年8期
Journal of Geriatric Cardiology2023年8期
- Journal of Geriatric Cardiology的其它文章
- Prolonging dual antiplatelet therapy improves the long-term prognosis in patients with diabetes mellitus undergoing complex percutaneous coronary intervention
- Age-related outcomes in patients with cardiogenic shock stratified by etiology
- Prognostic value of hematological parameters in older adult patients with acute coronary syndrome undergoing coronary intervention: a single centre prospective study
- Transcatheter aortic valve implantation in a patient with anomalous right coronary artery originating from the left aortic sinus with interarterial course
- The first experience of multi-gripper robot assisted percutaneous coronary intervention in complex coronary lesions
- Feasibility of emergent transcatheter aortic valve replacement sequentially followed by cardiac computed tomography angiography: experience from the procedure
