Age-related outcomes in patients with cardiogenic shock stratified by etiology
Alexander Schmitt ,Kathrin Weidner,✉ ,Jonas Rusnak ,Marinela Ruka ,Sascha Egner-Walter ,Kambis Mashayekhi ,Péter Tajti,Mohamed Ayoub,Ibrahim Akin,Michael Behnes,Tobias Schupp
1.Department of Cardiology,Angiology,Haemostaseology and Medical Intensive Care,University Medical Centre Mannheim,Medical Faculty Mannheim,Heidelberg University,Mannheim,Germany;2.European Center for AngioScience (ECAS),German Center for Cardiovascular Research (DZHK) partner site Heidelberg/Mannheim,Mannheim,Germany;3.Department of Internal Medicine and Cardiology,Mediclin Heart Centre Lahr,Lahr,Germany;4.Gottsegen György National Cardiovascular Center,Budapest,Hungary;5.Division of Cardiology and Angiology,Heart Center University of Bochum-Bad Oeynhausen,Bad Oeynhausen,Germany
ABSTRACT BACKGROUND As a result of improved and novel treatment strategies,the spectrum of patients with cardiovascular disease is consistently changing.Overall,those patients are typically older and characterized by increased burden with comorbidities.Limited data on the prognostic impact of age in cardiogenic shock (CS) is available.Therefore,this study investigates the prognostic impact of age in patients with CS.METHODS From 2019 to 2021,consecutive patients with CS of any cause were included.The prognostic value of age (i.e.,60-80 years and > 80 years) was investigated for 30-day all-cause mortality.Spearman’s correlations,Kaplan-Meier analyses,as well as multivariable Cox proportional regression analyses were performed for statistics.Subsequent risk assessment was performed based on the presence or absence of CS related to acute myocardial infarction (AMI).RESULTS 223 CS patients were included with a median age of 77 years (interquartile range: 69-82 years).No significant difference in 30-day all-cause mortality was observed for both age-groups (54.6% vs.63.4%,log-rank P=0.169;HR=1.273,95% CI: 0.886-1.831,P=0.192).In contrast,when analyzing subgroups stratified by CS-etiology,AMI-related CS patients of the group > 80 years showed an increased risk of 30-day all-cause mortality (78.1% vs.60.0%,log-rank P=0.032;HR=1.635,95% CI: 1.000-2.673,P=0.050),which was still evident after multivariable adjustment (HR=2.072,95% CI: 1.174-3.656,P=0.012).CONCLUSIONS Age was not associated with 30-day all-cause mortality in patients with CS of mixed etiology.However,increasing age was shown to be a significant predictor of increased mortality-risk in the subgroup of patients presenting with AMI-CS.
The clinical syndrome of cardiogenic shock (CS)is a medical emergency associated with high mortality and complex hemodynamic pathophysiology involving multiple organ systems.[1]Depending on the observed patient cohort and CS etiology,in-hospital mortality ranges from 30%-50%,while CS is most commonly caused by acute myocardial infarction(AMI).[2-5]It has been estimated that 3%-13% of all AMI are complicated by CS.[6-9]To further stress the clinical significance of CS,it should be mentioned that approximately 32% of patients with AMI complicated by CS(AMI-CS) experience multiorgan failure.[10]
Despite the positive impact of percutaneous coronary intervention (PCI) on clinical outcomes of patients suffering from AMI-CS,additional significant mortality-reducing interventions or treatments for CS have yet to be determined.[11-13]Coronary artery reperfusion through PCI has substantially improved the management of AMI.[14,15]Therefore,it can be assumed that rates of AMI deteriorating to AMI-CS are reduced through early PCI.Accordingly,incidence of AMI-CS was shown to decrease.Nonetheless,an increase in heart failure related CS (HF-CS) and generally non-AMI-related CS could be observed.[3]Furthermore,mortality for HF-CS was shown to rise within the last decade.[16]With the continues ageing population,the prevalence of HF and general multimorbidity is steadily increasing,raising the importance of other forms of CS besides AMI-CS.[17-20]The complexity of managing patients admitted with multiple comorbid conditions is directly reflected in CS as incidence of multiorgan system failure in CS was shown to increase,especially in patients with higher baseline comorbidity.[10]This observation also has implications for the economic burden of CS because treatment cost is much higher when CS is accompanied by failure of additional non-cardiac organ systems.Mainly due to increased utilization of resources and longer hospitalization.[10]
Many parameters have been investigated for their prognostic impact in CS,but studies selectively and comprehensively assessing patients’ baseline characteristics as an indicator for short-term prognosis are limited.Given the current epidemiological trajectory with an ageing population and the comorbidities accompanied by ageing,the impact of age on prognosis in patients admitted with CS will continuously increase in relevance and therefore requires further evaluation.[19,20]
However,prior studies often comprised few elderly patients and primarily focused on patients with AMI-CS undergoing PCI[21-24]and receiving mechanical circulatory support (MCS),i.e.,venoarterial extracorporeal membrane oxygenation[25,26]or intra-aortic balloon pump[27].Consequently,the evidence concerning the prognostic value of age across different CS etiologies and in the elderly is scarce,although the significance of these cohorts is likely to increase in the future.
Therefore,our study aims to fill this knowledge gap by investigating the prognostic role of age in CS of different etiologies and patients of advanced age in a consecutively enrolled study cohort.
METHODS
Study Population,Design,and Data Collection
The present study prospectively included all consecutive patients presenting with CS of all entities on admission to the internal intensive care unit (ICU) at the University Medical Center Mannheim,Mannheim,Germany,from June 2019 to May 2021,as recently published.[28]All relevant clinical data related to the index event were documented using the electronic hospital information system as well as the IntelliSpace Critical Care and anesthesia information system (ICCA,Philips,Philips GmbH Market DACH,Hamburg,Germany) implemented at the ICU,organizing patient data such as admission documents,vital signs,laboratory values,treatment data and consult notes.The presence of CS,as well as important laboratory data,ICU-related scores,hemodynamic measurements,and ventilation parameters were assessed on the day of admission.
The present study derived from an analysis of the “Cardiogenic Shock Registry Mannheim” (CARESMAregistry),representing a prospective single-center registry including consecutive patients presenting with CS being acutely admitted to the ICU for Internal Medicine of the University Medical Center Mannheim,Mannheim,Germany (ClinicalTrials.gov Identifier: NCT05 575856).The registry was carried out according to the principles of the declaration of Helsinki and was approved by the Medical Ethics Committee II of the Medical Faculty Mannheim,University of Heidelberg,Mannheim,Germany.
Inclusion and Exclusion Criteria,Study Endpoints
For the present study,all consecutive patients with CS regardless of cause were included.All patients who were < 60 years of age were excluded.Risk stratification was performed according to patients’ age on admission(i.e.,60-80 years and > 80 years).
The diagnosis of CS was determined according to the current recommendations of the Acute Cardiovascular Care Association of the European Society of Cardiology.[29]Accordingly,CS was defined by hypotension(systolic blood pressure < 90 mmHg) for more than 30 min despite adequate filling status or need for vasopressor or inotropic therapy to achieve systolic blood pressure > 90 mmHg.Additionally,signs for end-organ hypoperfusion must be present such as oliguria with urine output < 30 mL/h,altered mental status,cold clammy skin,and increased lactate > 2 mmol/L.State of CS was classified using the SCAI (Society for Cardiovascular Angiography and Interventions) classification system.[30]
For the present study,further risk stratification was performed according to AMI and non-AMI related CS on admission according to current international guidelines.[15,31,32]ST-segment elevation myocardial infarction was defined as a novel elevation in the ST-segment in at least two contiguous leads with ST-segment elevation ≥2.5 mm in men < 40 years,≥ 2 mm in men ≥ 40 years,or≥ 1.5 mm in women in leads V2-V3 and/or 1 mm in the other leads.Non-ST-segment elevation myocardial infarction was defined as the presence of an acute coronary syndrome with a troponin I increase of above the 99thpercentile of a healthy reference population in the absence of ST-segment elevation,but persistent or transient ST-segment depression,inversion or alteration of T wave,or normal electrocardiogram,in the presence of a coronary culprit lesion.
The primary endpoint of the study was all-cause mortality at 30 days,which was documented using the electronic hospital information system and by directly contacting state resident registration offices (‘bureau of mortality statistics’).Identification of patients was verified by place of name,surname,day of birth,and registered living address.No patient was lost to follow-up regarding all-cause mortality at 30 days.
Statistical Analysis
Quantitative data is presented as mean ± SEM,medians (interquartile range,IQR),and ranges depending on the distribution of the data.They were compared using the independent Student’st-test for normally distributed data or the Mann-WhitneyUtest for nonparametric data.Deviations from a Gaussian distribution were tested by the Kolmogorov-Smirnov test.Qualitative data are presented as absolute and relative frequencies and were compared using the Pearson’s chi-squared test or the Fisher’s exact probability test,as appropriate.
Kaplan-Meier analyses according to patient age (i.e.,≤80 years and > 80 years) were performed within the entire study cohort and further stratified by the presence of AMI-CS and non-AMI-CS.Univariable hazard ratios(HR) were given together with 95% confidence interval(CI).Subsequently,multivariable Cox regression models were developed using the “forward selection” option,where only statistically significant variables (P<0.05) were included and analyzed simultaneously.Results of all statistical tests were considered significant forP-value < 0.05.All statistical analyses were performed with SPSS 25.0 (SPSS Inc.,IBM,Armonk,NY,USA).
语言主要分为声调和语调两类[7]。声调是贯通于整个音节的高低升降的调子,是指读每个音节时声音的变化,主要由音高决定[8]。其特点是通过不同长短、高低的声调来表达不同含义。语调指的是抑扬顿挫的腔调。语调语言的特点是,语言声调在不同样长短和高低时,只表示语气,而不影响语意。汉英分别属于声调和语调语言。所以,如果把普通话的声调语言特点用到具有语调语言特点的英语上就有问题。
RESULTS
Study Population
From June 2019 to May 2021,273 patients with CS were admitted to our institution.50 patients with < 60 years of age were excluded.The final study cohort comprised 223 CS patients with a median age of 77 years (IQR:69-82 years).The entire cohort was predominantly male(59%) but proportion of male sex was significantly different when comparing both age groups (65.1%vs.46.5%,P=0.008),with a higher percentage of female patients in the older cohort.
Table 1 displays further baseline characteristics of the study population divided by the age cut-off of 80 years.Vital signs and cardiovascular risk factors on admission were similar in both groups,except for smoking which was observed significantly more often in the younger group ≤ 80 years (42.8%vs.15.5%,P=0.001).While data on prior coronary artery disease (CAD) was alike,several other chronic conditions,i.e.,congestive HF (52.1%vs.30.9%,P=0.002),atrial fibrillation (52.1%vs.30.3%,P=0.002) and chronic kidney disease (52.1%vs.32.2%,P=0.005) were more prevalent in older patients > 80 years.Medication on admission was comparable in both groups except for higher use of beta-blockers (70.4%vs.50.0%,P=0.004) and diuretics (64.8%vs.40.1%,P=0.001) in the group > 80 years.
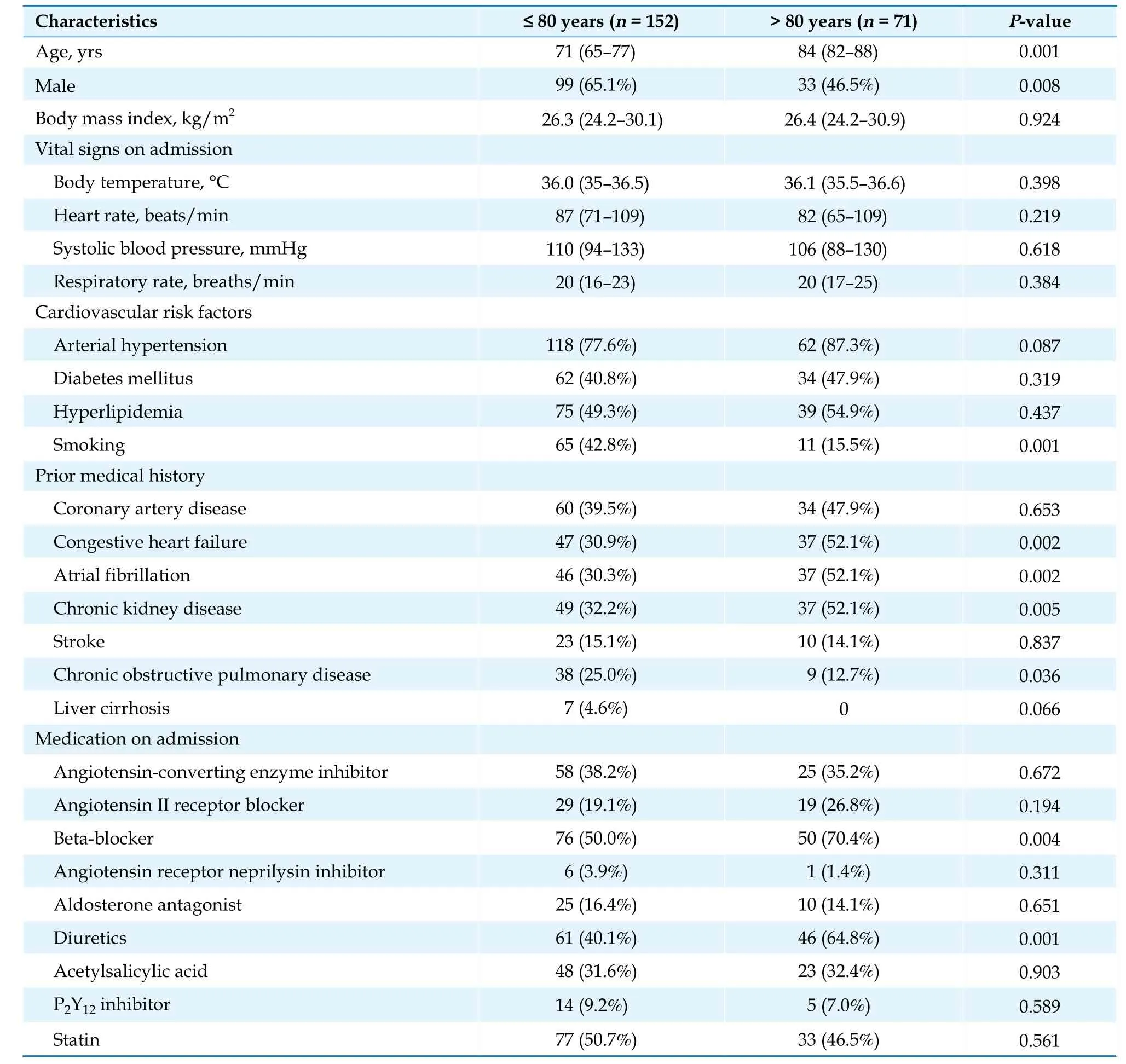
Table 1 Baseline characteristics for patients stratified by age ≤ 80 years and > 80 years.
Specific CS-related information,data on medical management,results of diagnostic procedures as well as endpoints for the two patient groups is illustrated in Table 2.Coronary angiography was performed similarly often in both groups (69.1%vs.64.8%,P=0.523).Status of CAD was observed to differ with 3-vessel disease being found more commonly in the older patient group > 80 years(73.9%vs.53.3%,P=0.012).Nonetheless,PCI was carried out more frequently in the younger group ≤ 80 years (75.2%vs.56.5%,P=0.021).Most CS cases were caused by AMI (49.3%vs.45.1%) and acute decompensated HF (25.8%vs.33.8%) whereas no statistically significant differences in CS-etiology between the younger and older patient cohort were observed (P=0.815).Patients ≤80 years were more often classified as having advanced stage CS (i.e.,stage E) (57.2%vs.36.6%,P=0.025).Furthermore,the rate of out-of-hospital cardiac arrest was higher in the younger group ≤ 80 years (40.1%vs.22.5%,P=0.012).Likewise,mechanical ventilation on admission (59.9%vs.39.4%,P=0.004) was more frequent in younger patients.Regarding laboratory values at baseline,only pH and white blood cell count showed significant differences,with lower pH (7.28vs.7.32,P=0.017) and higher white blood cell count (15.48 × 106/mLvs.12.24 × 106/mL,P=0.002) in the younger group ≤ 80 years.
Correlation of Age with Clinical and Laboratory Data
Table 3 outlines univariable correlations of age and selected parameters.Patients’ age correlated positively with levels of N-terminal pro-B-type natriuretic peptide (r=0.268,P=0.015).In contrast,an inverse correlation of age and the administered dose of norepinephrine on admission (r=-0.169,P=0.014) was demonstrated.

Table 3 Correlations of age with laboratory and clinical parameters in all patients.
Association of Age with 30-day All-cause Mortality
The primary endpoint of all-cause mortality at 30 days was observed in 54.6% of the cohort ≤ 80 years and in 63.4% of the cohort > 80 years (log-rankP=0.169).No significant difference regarding the risk of 30-day allcause mortality was observed when comparing the group of patients ≤ 80 years with patients > 80 years (HR=1.273,95% CI: 0.886-1.831,P=0.192) (Figure 1A).When further analyzing the subgroups of AMI-CS and non-AMI-CS patients,AMI-CS was shown to be associated with worse mortality in older patients > 80 years (78.1%vs.60.0%,log-rankP=0.032,HR=1.635,95% CI: 1.00-2.673,P=0.05) while non-AMI-CS was not (51.3%vs.49.4%,log-rankP=0.878,HR=1.042,95% CI: 0.606-1.791,P=0.881) (Figure 1B &1C).
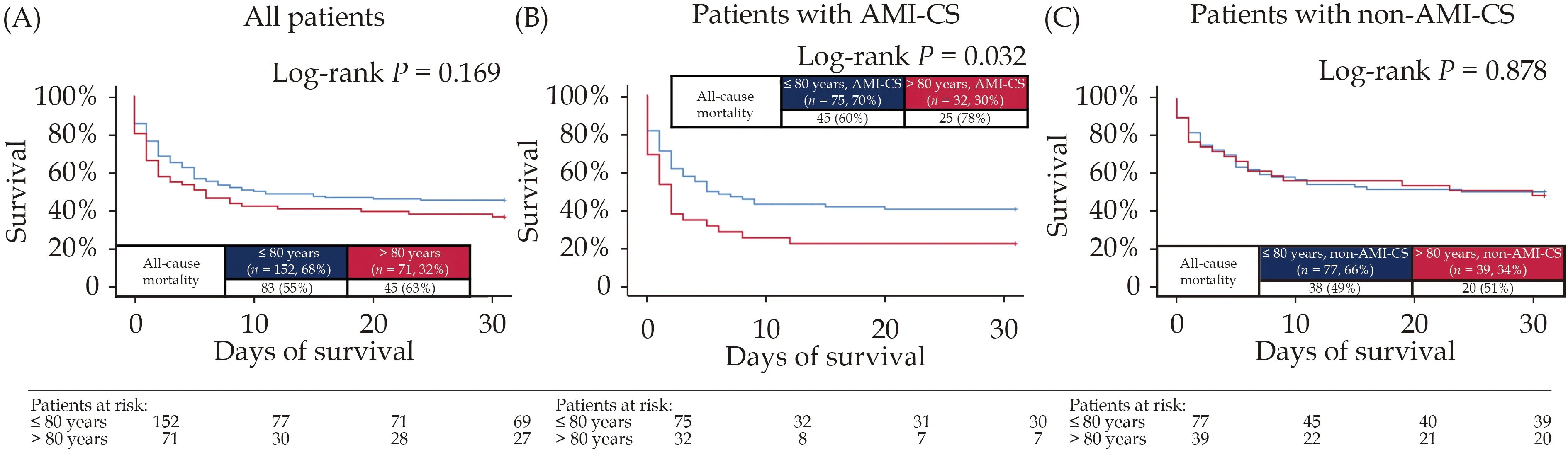
Figure 1 Kaplan-Meier analyses.Prognostic impact of age on the risk of 30-day all-cause mortality for the entire study cohort (A),patients with AMI-CS (B),and non-AMI-CS (C).AMI: acute myocardial infarction;CS: cardiogenic shock.
Multivariable Risk Prediction Models
Univariable and multivariable Cox regression ana-lyses were performed within the AMI-CS and non-AMICS cohorts.To take the important syndrome of frailty into account,biomarkers and comorbidities associated with frailty were incorporated in the analyses (i.e.,hemoglobin,C-reactive protein and malignancy).[33-35]Even after multivariable adjustment,age (i.e.,cut-off of 80 years) was associated with 30-day all-cause mortality within the cohort of AMI-CS (HR=2.072,95% CI: 1.174-3.656,P=0.012).Additionally,when age was included as a continuous variable,it remained an independent predictor of all-cause mortality in patients with AMI-CS(HR=1.035,95% CI: 1.002-1.069,P=0.039) (Table 4).

Table 4 Univariable and multivariable Cox regression analyses in patients with AMI-CS and non-AMI-CS regarding 30-day allcause mortality.
In the cohort of non-AMI-CS,age was not associated with an increased risk of all-cause mortality at 30 days(HR=1.274,95% CI: 0.676-2.400,P=0.453).However,lactate levels and the need for cardiopulmonary resuscitation were associated with higher mortality in univariable and multivariable Cox regression within the cohort of non-AMI-CS (Table 4).
DISCUSSION
This prospective observational study comprehensively investigated the prognostic value of age in consecutive patients with AMI and non-AMI-related CS admitted to an internal ICU between 2019 and 2021.There was no statistical difference in 30-day all-cause mortality when comparing CS patients of different age groups (i.e.,≤ 80 years and > 80 years).Selective analyses stratified by CS-etiology (i.e.,AMI-CSvs.non-AMI-CS) demonstrated a significantly increased mortality-risk in AMI-CS patients of the age group > 80 years,which was still evident after multivariable adjustment.Conversely,no difference in prognosis was observed when comparing the two age groups in the non-AMI-CS cohort.
Ageing is known to be a significant and independent risk factor for the development of cardiovascular disease(CVD) and many other conditions such as chronic kidney disease,hypertension,or type 2 diabetes mellitus.Therefore,elderly patients usually present with worse cardiovascular risk profile and generally more comorbidities when compared to their younger counterparts.[19,36]Besides multimorbidity,age is often accompanied by polypharmacy,frailty,and reduced functional reserve,continuously adding complexity to the management of CVD.[37,38]
Given these circumstances,there are relevant differences in the treatment and prognosis of elderly individuals with CVD.Studies investigating HF in the elderly have established that even diagnosing HF is challenging because symptoms are more frequently atypical and can be disguised or simulated by comorbidities.[39]In turn,delayed diagnosis and initiation of adequate treatment further contribute to worse outcomes.[40]However,patients of higher age are also less likely to receive guideline-directed treatments even after HF diagnosis[41,42]and the current recommendations for the management of HF are mainly based on evidence of clinical trials that have often excluded older patients despite this population being the most affected.[43,44]
Regarding AMI and CAD,adequate diagnosis in older patients also seems to be influenced by atypical symptoms and presentation,leading to delayed contact to medical professionals and initiation of therapy.[45-47]Furthermore,assessing eligibility for interventional reperfusion in older individuals remains complex and often culminates in less frequent utilization of PCI.[46,48]Even though,its prognostic benefits seem to be maintained in patient of advanced age.[49,50]
Despite the progressive ageing of the population and continuous increases in the rates of CVD,elderly patients remain underrepresented in clinical trials or registries investigating cardiovascular conditions related to strict exclusion criteria in randomized controlled trials.[51,52]This results in a lack of knowledge concerning the prognosis and management of this increasingly relevant cohort.The absence of reliable data in this cohort could prompt clinicians to more conservative treatment approaches which may diverge substantially from guideline recommendations.Therefore,investigating the prognostic impact of age,especially in very acute conditions such as CS,is paramount.
Previous studies and scoring systems have predominantly established age cut-offs between 65-75 years.[4,24,53-55]However,most prior studies investigated patient cohorts that were younger than our cohort [e.g.,RESCUE[53]:mean age of 66 ± 14 years;SHOCK trial[56]: mean age of 68.7 ± 11.8 years;CardShock[4]: mean age of 67 ± 12 years;Cardiovascular Shock[57]: median age of 72 years (IQR:63-81 years);compared to our cohort: median age of 77 years (IQR: 69-82 years)].Especially the Cardiovascular Shock Registry did not observe age to be associated with impaired survival.However,the authors themselves note that this could have been attributable to their relatively low number of elderly patients.[57]Considering the progressively increasing life expectancy,advancing treatment capabilities,high median age of our cohort and lack of data in patients at very advanced age;we decided to set the age cut-off slightly higher than previous studies (i.e.,≤ 80 years and > 80 years).In addition,prior investigations in patients with acute HF as a possible cause of CS observed the steepest increase in mortality between the age groups 75-84 years and 85-94 years.[41]Due to the high proportion of CS related to acute decompensated HF in our cohort (25.8% and 33.8% in the groups ≤80 years and > 80 years,respectively),we wanted to take these findings into account to improve discrimination of effects on mortality.Patients < 60 years of age were excluded because of the high heterogeneity regarding comorbidities within this cohort.These patients commonly suffer from less comorbidities than patients at a more advanced age.Since we wanted to compare the prognosis of old versus very elderly patients,we decided it was appropriate to exclude those < 60 years.
The current state of evidence suggests that advanced age may be associated with higher mortality rates in patients suffering from CS.[4,36,53,54]This finding was primarily attributed to age-related factors like the aforementioned multimorbidity,frailty or reduced functional reserve.While higher comorbidity among older patients was also present in our study,mortality did not differ between the two age groups when considering the entire cohort.Even though our entire study cohort was predominantly male,the percentage of female patients increased significantly in the cohort > 80 years (34.9%vs.53.5%) which is also in line with investigations from Jentzer,et al.[54]and Kanwar,et al.[36]A high proportion of females is a notable finding since they are generally underrepresented in CS studies.[58-60]It suggests that the emergency of CS could progressively affect more females as average life expectancy increases.
Even though significance of non-AMI-CS was observed to increase,[3,16]selective analyses of CS mortality in different age groups stratified by CS-etiologies besides AMI-CS were beyond most previous studies.Data derived from studies that did in fact perform such analyses is heterogeneous,especially due to differences in the chosen age cut-offs and inclusion of CS-etiologies in the non-AMI-CS cohorts.Kanwar,et al.[36]divided their cohort into AMI-CS and strictly HF-CS.Statistically significant higher mortality rates in older patients were only found in the HF-CS group.However,a trend towards higher mortality was also observed in the AMI-CS group.Osman,et al.[61]performed age stratified sex-related differences in CS patients which is not entirely applicable to our study settings and selective analysis for age alone was not performed.Nonetheless,their data also suggests increasing mortality with advancing age as well as generally higher mortality in AMI-CS when compared to non-AMI-CS.
In our study population,selective analyses stratified by CS-etiology (i.e.,AMI-CSvs.non-AMI-CS) demonstrated significantly higher 30-day all-cause mortality in AMI-CS patients > 80 years but no age-related difference in the non-AMI-CS cohort.It should be noted that mortality rates of both age groups in the AMI-CS cohort were rather high (60% and 78%),compared to prior studies investigating AMI-CS patients.[13,62,63]Since advanced age as well as CS stage have been shown to predict higher mortality,this could be attributable to the high median age of our entire cohort (77 years) and the circumstance that of all patients,50.7% of patients presented with advanced CS (the Society for Cardiovascular Angiography and Intervention stage E).[54]Of note,median age in CS patients included in randomized controlled trials varies from 66-71 years.[13,62-64]Furthermore,distribution of CS severity can show substantial differences between studies due to the use of varying definitions of classifying CS.[54]
Regarding treatment approaches in the entire cohort,more intensive medical management,including mechanical ventilation and invasive coronary revascularization (PCI),was observed in the younger patient group ≤80 years.Although,coronary angiography rates were similar in both groups and status of detected CAD severity was even worse among older patients.This suggests that many older patients may have been ineligible for PCI or that physicians were often reluctant to perform invasive revascularization,potentially due to age-related reasons such as higher morbidity,assumed risk or limited life expectancy.This finding may have the greatest impact on mortality,especially in the subgroup of patients with AMI-CS,as PCI is currently the only medical intervention that was shown to reduce mortality in randomized clinical trials.[13,65]In addition,the use of mechanical circulatory assist devices only narrowly missed the level of statistical significance for higher use in younger patients (7.9%vs.1.4%,P=0.054).This could be cautiously interpreted as a statistical trend further corroborating more extensive medical treatment in younger patients and would be in line with observations in prior CS studies.[3,54,55]However,routine use of MCS devices like the intra-aortic balloon pump have not been shown to improve survival in AMI-CS patients and their utilization is associated with additional inherent risks,such as vascular complications,risk of infection,bleeding or mechanical malfunction.[63,66]Furthermore,age was shown to be a major predictor of worse outcomes in several studies investigating the use of extracorporeal membrane oxygenation.[67,68]Finally,the potential benefit of MCS devices must be weighed carefully against their complications,especially because older patients might have decreased physiologic reserve which could render them unable to withstand these complications.[69]Nonetheless,advanced age should be considered together with other factors,such as baseline comorbidity or clinical presentation,when determining the utilization of interventional revascularization or initiation of MCS devices and it should not be viewed as an absolute contraindication if cardiac recovery seems feasible.[70]Our findings,particularly the higher mortality observed in older AMI-CS patients > 80 years,underscore the importance of a comprehensive risk assessment in clinical decisionmaking and further research is needed to identify patients of advanced age where the benefit of escalating medical management outweighs the potential risks.
LIMITATIONS AND STRENGTHS
This study has several limitations.Due to the singlecenter and observational study design,results may be influenced by measured an unmeasured confounding regardless of performing multivariable Cox regression to adjust for potential confounders.Further,we only observed a modest sample size and patients with out-of-hospital cardiac arrest not transferred to our institution could not be included in the study.In addition,no information on mortality beyond 30 days was available for the present study.
Despite these limitations,our study provided relevant data investigating the prognostic impact of age in CS patients through comprehensive statistical analysis of a diverse patient cohort presenting with CS.Unlike previous studies where predominantly younger patients and AMI-CS were investigated,our study cohort was characterized by high median-age and CS caused by different pathologic conditions.Furthermore,patients were enrolled consecutively,ensuring a more randomized and representative study cohort.
CONCLUSIONS
In conclusion,our study demonstrated that 30-day allcause mortality was not associated with patient age in a CS cohort of different etiology,while medical management showed significant disparities in patients with advanced age.The selective group of patients with AMI-CS was observed to be at higher risk of mortality when compared to non-AMI-CS with higher age being an impactful factor contributing to higher mortality in this cohort.
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose.
 Journal of Geriatric Cardiology2023年8期
Journal of Geriatric Cardiology2023年8期
- Journal of Geriatric Cardiology的其它文章
- Prolonging dual antiplatelet therapy improves the long-term prognosis in patients with diabetes mellitus undergoing complex percutaneous coronary intervention
- Development and validation of a score predicting mortality for older patients with mitral regurgitation
- Prognostic value of hematological parameters in older adult patients with acute coronary syndrome undergoing coronary intervention: a single centre prospective study
- Transcatheter aortic valve implantation in a patient with anomalous right coronary artery originating from the left aortic sinus with interarterial course
- The first experience of multi-gripper robot assisted percutaneous coronary intervention in complex coronary lesions
- Feasibility of emergent transcatheter aortic valve replacement sequentially followed by cardiac computed tomography angiography: experience from the procedure
