Pneumonia and ocular disease as the primary presentations of Takayasu arteritis: a case report
Dong-Ming Xu
Department of Emergency Medicine, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China
Dear Editor,
Takayasu arteritis (TA) is a rare, idiopathic, granulomatous,large-vessel vasculitis, with preferential involvement of the aorta, its main branches, and pulmonary arteries[1].It has been reported that the ocular involvements were found in 8.1%-68%[2], non-specific arthralgia or myalgia in 13%-41%,aortic regurgitation in 5%-55%, coronary vessel stenosis in 25%, pulmonary hypertension in approximately 10%,cutaneous involvement in 3%-28%, and inflammatory bowel disease in 2.6% of TA patients[1].Pneumonia as the primary manifestation is a rare presentation of TA[3-5].We report a case of a young male patient who presented with blurry vision and antibiotic-unresponsive pneumonia, and was subsequently diagnosed with TA.
Ethical ApprovalThis study was approved by the Ethics Committee of Beijing Friendship Hospital, Capital Medical University, China (approval number: 2020-P2-006-01),and was conducted in accordance with the principles of the Declaration of Helsinki.Written informed consent was obtained from the patient.
A 32-year-old man, with complaints of fever, severe dry cough, and blurred vision in the right eye for 2wk.Two weeks ago, the patient reported feeling fatigue and developed a fever with a maximum body temperature of 38.5℃.The fever was accompanied with severe dry cough and blurred vision in the right eye.The patient had smoked 20 cigarettes/d for 20y.He also had a history of poorly controlled hypertension for 3y.He had been diagnosed with pneumonia and hypertension at a local hospital, and received moxifloxacin to treat the infection,telmisartan to control the blood pressure, and acetaminophen to reduce the fever.However, his symptoms persisted, and then he was transferred to our emergency department.At presentation, fundoscopic examination revealed optic nerve atrophy in the right eye and mild papilledema in the left eye.Laboratory examinations reported the following results:coronavirus disease 2019, negative; white blood cells,10 860/mm3(normal value, 4800-10 800/mm3); absolute value of neutrophils, 8680/mm3(normal value, 1800-6300/mm3);percentage of neutrophils, 79.9% (normal value, 50%-70%);erythrocyte-sedimentation rate, 91 mm/h (normal value,0-20 mm/h); C-reactive protein, 259.79 mg/L (normal value,0-5 mg/L); anti-extractable nuclear antigen antibody, negative;antineutrophil cytoplasmic antibody, negative; ferritin,negative; tumor markers, negative; and cerebral spinal fluid examination, negative.Chest computed tomography (CT) scan showed large ground glass opacities and consolidations in bilateral lungs (Figure 1A and 1B).Brain magnetic resonance imaging (MRI) scan showed multiple speckled or patchy ischemic lesions in the right and left basal ganglia and the right thalamus (Figure 1C), as well as stenosis of the A2 segment of the right and left anterior cerebral arteries and the M1 segment of the right middle cerebral artery (Figure 1D).Orbital MRI detected inflammatory changes in the right optic nerve (Figure 1E).Fundus fluorescein angiography revealed delayed fluorescence filling in the right ophthalmic artery and multiple early filling defects in the choroidal lobules.Optical coherence tomography angiography showed extremely thin retinal arteries bilaterally, which is consistent with ischemic changes.Echocardiography showed enlargement of both atria and the left ventricle, thickening of the left ventricular wall,and a decreased left ventricular ejection fraction of 36.1%.A fluorodeoxyglucose positron emission tomography/CT showed arterial wall thickening in bilateral internal carotid arteries, bilateral common carotid arteries, the brachiocephalic trunk, the superior mesenteric artery, and bilateral renal arteries, with slightly increased local18F-fluorodeoxyglucose uptake, suggesting systemic arteritis without significant lesions in the aorta or its branches or the pulmonary artery(Figure 2).We diagnosed him as TA.He received intravenous methylprednisolone (500 mg/d for 3d, decreased to 80 mg/d for 5d and then to 40 mg/d for 5d), cyclophosphamide (600 mg every 2wk), and tocilizumab (640 mg every 4wk).Anti-hypertensive agents (amlodipine 5 mg/d combined with sacubitril/valsartan 100 mg/d, spironolactone 40 mg/d, and metoprolol 50 mg/d),ventricular rate control agent (ivabradine 5 mg/d), cardiac function improvement agent (lyophilized recombinant human brain natriuretic peptide 0.5 mg/d), ophthalmic vascular circulation improvement agent (extract ofGinkgo bilobaleaves 17.5 mg/d), and a neuroprotective agent (vitamin B12500 μg/d) were also given.The patient experienced significant improvements in the clinical manifestations of fever and dry cough.Chest CT showed significant shrinkage of the ground glass opacities and consolidations in both lungs.Orbital MRI,however, showed no change in the lesion in the right optic nerve.The patient was discharged and was followed up in the clinic.
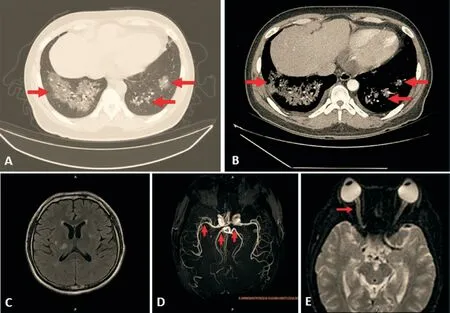
Figure 1 Chest CT, brain MRI, and magnetic resonance angiography examinations Non-contrast-enhanced CT imaging (A) and contrastenhanced CT imaging (B) show large ground glass opacities and consolidations (arrows) in bilateral lungs.In addition, aorta shows satisfactory contrast filling without stenosis or wall thickening (B, arrowhead).Brain MRI showing multiple speckled or patchy ischemic lesions in both the right and left basal ganglia and the right thalamus (C).Brain magnetic resonance angiography reveals stenosis of the A2 segment of the right and left anterior cerebral arteries (arrows) and the M1 segment of the right middle cerebral artery (arrowhead, D).Orbital MRI presents an abnormally high signal in the orbital segment and intraductal segment of the right optic nerve (arrow) on diffusion-weighted imaging,suggesting inflammatory changes in the right optic nerve (E).CT: Computed tomography; MRI: Magnetic resonance imaging.
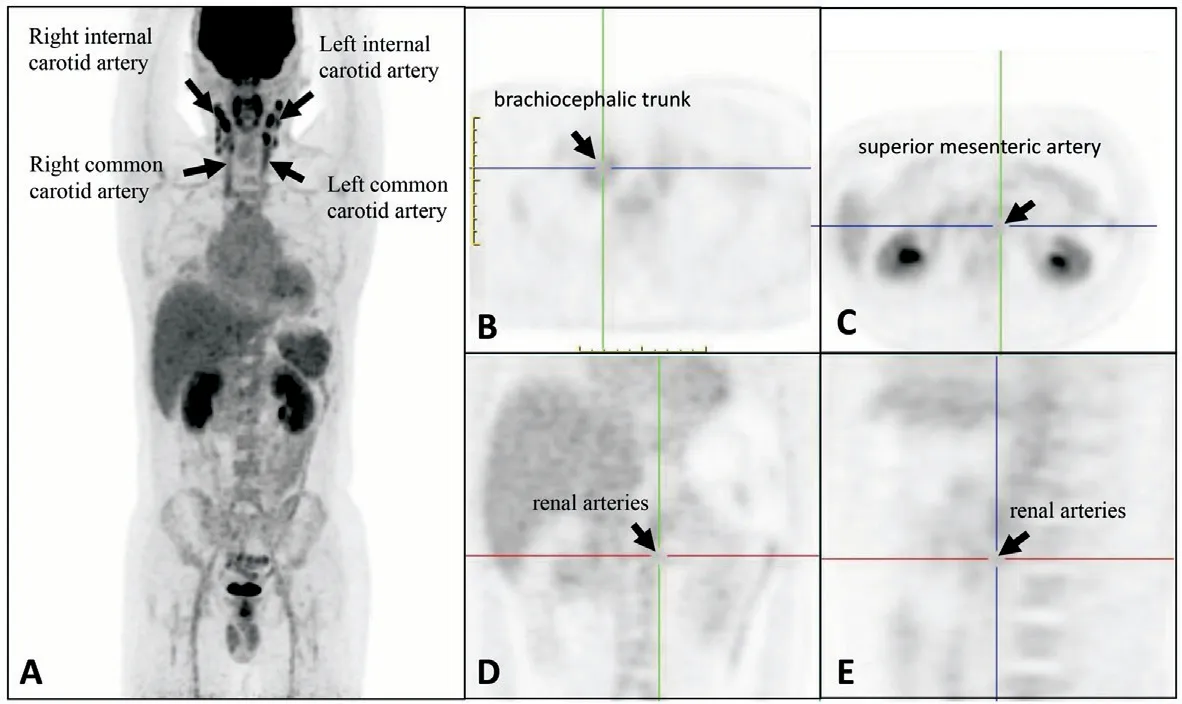
Figure 2 Fluorodeoxyglucose positron emission tomography/computed tomography images Increased radiolabel uptakes at the internal carotid arteries (A), common carotid arteries (A), brachiocephalic trunk (B), superior mesenteric artery (C), and renal arteries (D and E), without significant uptakes in the aorta, its main branches, and the pulmonary arteries (A).
The clinical features of TA are variable.The concordance of at least 3 of the 6 features proposed by the American College of Rheumatology criteria has been commonly accepted as a diagnostic standard for TA[6].However, the diagnosis of TA may be challenging in patients with non-specific or rare clinical presentations[1].In this study, we report a case of TA with dry cough and blurred vision as the chief complaints.Our patient did not show any sign of vascular inflammation in the aorta and its main branches.However, positron emission tomography/CT demonstrated systemic arteritis involving bilateral internal carotid arteries, bilateral common carotid arteries, the brachiocephalic trunk, the superior mesenteric artery, and bilateral renal arteries.After the exclusion of cancer and autoimmune diseases, the patient was diagnosed with TA, with pneumonia and ocular disease as the primary manifestations.Pulmonary involvement in TA mainly consists of stenosis or occlusion of the pulmonary artery[1].Other forms of pulmonary involvement are rare, such as pulmonary fibrosis,acute interstitial pneumonitis, parenchymal consolidations, and organizing pneumonia[3-5].Our patient had bilateral opacities and consolidations that were unresponsive to antibiotics,but resolved after methylprednisolone, cyclophosphamide,and tocilizumab administrations.Hence, his pulmonary involvement was considered to be pneumonitis but not bacterial pneumonia.Ocular diseases are one of the most frequent manifestations of TA, and retinal alterations are the most common ocular lesions of TA[2].TA-associated retinal alterations may be secondary to carotid artery stenosis leading to eye hypoperfusion or to renal artery stenosis leading to renal hypertension and hypertensive retinopathy[7].However, TA patients with ocular involvement show variable responses to treatment with steroids and/or immunosuppressants.Pallangyoet al[8]reported a 24-year-old TA woman with bilateral ocular ischemic blindness.She was treated with dexamethasone,methotrexate, and low-dose aspirin; however, her vision did not improve but rather deteriorated further.Christiansenet al[9]described a 19-year-old TA woman with vision loss in the right eye and bright light-induced amaurosis in the left eye.Administrations of steroids, methotrexate, and infliximab improved the left eye vision, but the vision loss in the right eye was permanent[9].Guptaet al[7]reported an 18-year-old man with sudden loss of the vision due to TA with occlusions of the central retinal artery and superior temporal branch of the retinal vein.After prednisolone and methotrexate administrations, the patient's visual acuity improved 3mo later, with evidence of neovascularization 2.5y later[7].In the present case, the patient was considered to have optic neuritis and absolute ophthalmic artery occlusion in the right eye.This patient received the steroids and immunosuppressant treatment.In addition, we also usedGinkgo bilobaextract that was reported to improve the ocular blood circulation[10].However, he had no significant improvement in his right eye vision.He was suggested to regularly visit the ophthalmology clinic for follow-up.
Patients with certain systemic diseases can initially present with eye disorders.For example, a young man who presented with atypical keratitis was finally diagnosed with coronavirus disease 2019[10].Another patient with Adams-Oliver syndrome,a genetic disorder causing extremity and scalp defects, was reported to have signs of exudative vitreoretinopathy[11].These cases and the present case serve as a reminder that clinicians who evaluate patients with eye disorders must consider and rule out systemic diseases.
We have described a case of a young man who presented with antibiotic-unresponsive pneumonia and ocular disease,and was subsequently diagnosed with TA.The patient's pneumonia was significantly improved after the administration of methylprednisolone, cyclophosphamide, and tocilizumab.This case suggests that TA should be considered or excluded as a diagnosis in patients with antibiotic-unresponsive pneumonia and ocular diseases.
ACKNOWLEDGEMENTS
Conflicts of Interest: Xu DM,None.
 International Journal of Ophthalmology2023年7期
International Journal of Ophthalmology2023年7期
- International Journal of Ophthalmology的其它文章
- Research on classification method of high myopic maculopathy based on retinal fundus images and optimized ALFA-Mix active learning algorithm
- Predicting visual acuity with machine learning in treated ocular trauma patients
- ldentification of hub genes for glaucoma: a study based on bioinformatics analysis and experimental verification
- Protective effect of ginsenoside Rg1 on 661W cells exposed to oxygen-glucose deprivation/reperfusion via keap1/nrf2 pathway
- Effects of endogenous dopamine induced by low concentration atropine eye drops on choroidal neovascularization in high myopia mice
- Differential analysis of aqueous humor cytokine levels in patients with macular edema secondary to diabetic retinopathy or retinal vein occlusion
