The role of quick Sepsis-related Organ Failure Assessment score as simple scoring system to predict Fournier gangrene mortality and the correlation with Fournier’s Gangrene Severity Index: Analysis of 69 patients
Bambang S.Noegroho, Kuncoro Adi, Akhmad Mustafa,Rais Syaeful Haq, Zola Wijayanti, Jason Liarto
Urology Department, Hasan Sadikin Academic Medical Center, Universitas Padjadjaran, Bandung,Indonesia
KEYWORDS Fournier gangrene;Quick Sepsis-related Organ Failure Assessment;Prognosis;Organ failure;Severity index
Abstract Objective: Fournier’s gangrene is a rare but life-threatening infection disease with high mortality rate.The quick Sepsis-related Organ Failure Assessment (qSOFA) is a new and simpler scoring system that may identify patients with suspected infection who are at greater risk for a poor outcome.The purpose of this study was to find out role of qSOFA in determining prognosis of Fournier’s gangrene patients.Methods: This study is a case control with retrospective review of Fournier’s gangrene patients treated at Hasan Sadikin Hospital from January 2013 to December 2017 who met inclusion criteria.Participants were divided into two groups according to qSOFA score as high qSOFA(2—3) and low qSOFA (0—1).Results: From 69 patients,the mortality rate was 24.6%.The sensitivity of qSOFA score to predict mortality was 88.2%;the specificity was 94.2%;positive predictive value was 83.3%;negative predictive value was 96.1%; positive likelihood ratio was 15.2; negative likelihood ratio was 0.12; and the area under the receiver operating characteristic curve of qSOFA was 94.2%.There was significant association between qSOFA scale and mortality with p-value of 0.0001.The qSOFA score has strong positive correlation with Fournier’s Gangrene Severity Index (p<0.0001, r=0.704).Conclusion: qSOFA scoring system has a high prognostic value and can be used to determine prognosis of Fournier’s gangrene patients.
1.Introduction
Fournier’s gangrene (FG) is a form of necrotizing fasciitis of the genital and perineum that is potentially life-threatening.Most FG cases were found in adult men,and rare cases in women and children.This condition is a urologic emergency that causes fulminant infection that spreads through fascia, leading to sepsis and death [1,2].The incidence of FG is one of 7500 populations, while in Indonesia,the incidence is not well documented.Globally,the incidence is increasing with the increase of population, diabetes mellitus, and multi-resistant pathogens[3,4].
In 1995,Laor et al.[5]reported the Fournier’s Gangrene Severity Index (FGSI) that modified from Acute Physiology and Chronic Health Evaluation (APACHE) II score that calculated nine parameters as specific prognostic index for FG patients.FGSI is the most used scoring system for evaluating the treatment of choice and disease progression[5,6].In 2010 Yilmazlar et al.[7] reported the Uludag Fournier’s Gangrene Severity Index(UFGSI)with addition of new parameters in FGSI, which were age and gangrene surface area with aim to get more accurate scoring system and better prognosis.
Both scoring systems have similarities that multiple laboratory findings are needed to complete the score.In developing countries such as Indonesia, especially in rural areas, most hospitals do not have such laboratory examinations.Most primary healthcare and hospitals in rural areas could not perform electrolyte and bicarbonate examination.Moreover, with more laboratory examination performed repeatedly, it will cause more cost that could have been saved.Hence, in such areas the FGSI is not applicable.Other simpler scoring system is needed that even a general practitioner in emergency room can calculate to determine if their hospital still can handle the patient, or referral to higher hospital should be made as soon as possible.
A simple scoring system “quick Sepsis-related Organ Failure Assessment” (qSOFA) is a simpler form of Sequential Organ Failure Assessment (SOFA) score.This scoring system is easy to calculate and efficient in daily practice.It could identify sepsis patients with poor prognosis with only three clinical parameters:blood pressure,respiratory rates, and the Glasgow Coma Scale (GCS) [8].This study aimed to determine the role of qSOFA score to predict mortality in FG patients, in order to help clinical decision making by physicians in rural area, whether their hospital is sufficient to handle a low-risk for mortality patient or referral should be made.
2.Methods
This is an observational retrospective analytic study.Data were obtained from FG patients admitted to Hasan Sadikin Hospital in 5-year interval(January 2013—December 2017).Demographical data were collected including sex, age,comorbidity, blood pressure, heart rate, respiratory rate,GCS score hemoglobin level, leucocyte count, thrombocyte, blood urea nitrogen, creatinine level, sodium, potassium, and bicarbonate.We calculated the qSOFA score based on three parameters: blood pressure, respiratory rate, and GCS.The FGSI score was calculated based on the study by Laor et al.[5].We included all FG patients with perineal and/or inguinal involvement and above.Patients with only isolated scrotal or penile involvement without Colles’fascia involvement were categorized as scrotal and/or penile abscesses and excluded from the study.
We divided patients according to the qSOFA score into two categories:low risk(0—1)and high risk(2—3),and then we analyzed the sensitivity, specificity, positive predictive value(PPV),negative predictive value(NPV),and likelihood ratio (LR) of qSOFA towards mortality (Table 1).We also made a correlation analysis between qSOFA score and FGSI using Pearson test to determine the correlation between qSOFA and FGSI.Statistical analysis was done using SPSS statistics for Windows (ver.21.0., IBM Corp., Armonk, NY,USA).
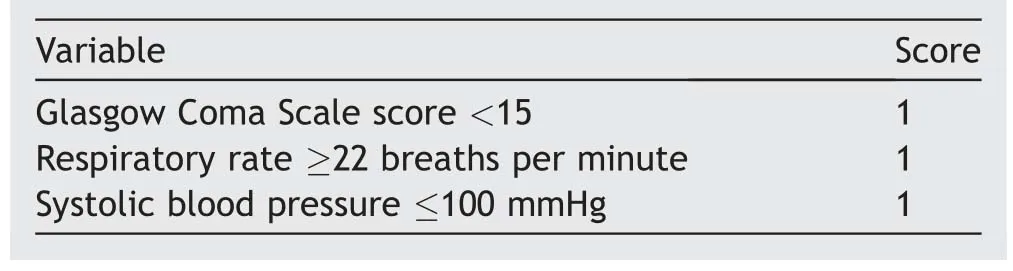
Table 1 Quick Sepsis-related Organ Failure Assessment score.
3.Results
Between 2013 and 2017, there were 69 patients admitted to Hasan Sadikin Hospital due to FG.Fifty-two (75.4%)patients survived and were able to receive primary closure of the defect using skin graft, while 17 (24.6%) patients died through the course of the treatment due to severe infection even after adequate debridement.The mean age of the survivor group (Group 1) was significantly younger than non-survivor group (Group 2) (51.13 [SD 14.56] yearsvs.60.17 [SD: 11.32] years,p=0.018; SD, standard deviation).The mean systolic blood pressure at hospital admission was significantly lower in Group 2 compared to Group 1 (117.86 [SD: 19.75] mmHgvs.103.50 [SD: 23.17]mmHg,p=0.031).The median initial GCS score was also significantly lower in Group 2 compared to Group 1 (15[IQR: 13—15]vs.13 [IQR: 10—15],p=0.0001; IQR, interquartile range).The mean respiratory rate of FG patients was significantly higher in Group 2 compared to Group 1(21.27 [SD: 2.88]vs.26.94 [SD: 5.34] breaths per minute,p=0.001) (Table 2).

Table 2 Fournier gangrene patient demographic.
We also documented the comorbidities of the FG patients such as diabetes, tuberculosis, human immunodeficiency virus,autoimmune diseases,and perianal abscesses.There was no single comorbidity that was significantly different between the two groups (p>0.05).From the laboratory result, the hemoglobin levels, leucocyte counts,sodium levels,potassium levels,blood urea nitrogen levels,creatinine levels, HCO3-levels, and random blood glucose levels were not significantly different between the two groups(p>0.05).Only mean thrombocyte count(384 921.57[SD: 175 107.00] per mm3vs.266 937.50 [SD:153 547.00] per mm3,p=0.018) and mean albumin level(2.383 [SD: 0.894] g/dLvs.1.730 [SD: 0.404] g/dL,p=0.017) were significantly different between the two groups,where in Group 1 the mean thrombocyte count and mean albumin level were higher than Group 2 (Table 2).
In Group 1,the qSOFA score were categorized as low risk in 49 (94.2%) patients and high risk in 3 (5.8%) patients,while in Group 2 the score were considered as low risk in 2 (11.8%) patients and high risk in 15 (88.2%) patients; the scores were significantly different between the two groups(p=0.0001).The sensitivity of qSOFA score to predict mortality was 88.2%; specificity was 94.2%; PPV of qSOFA score was 83.3%;NPV was 96.1%.The positive LR for qSOFA score predict mortality of FG was 15.2, while the negative LR was 0.12.The area under the receiver operating characteristic curve (AUC) was 94.2%.The sensitivity of FGSI score to predict mortality was 94.1%; specificity was 90.3%; PPV of FGSI score was 76.1%; NPV was 97.9%.The positive LR for FGSI score to predict mortality of FG was 9.7,while the negative LR was 0.065.The AUC for FGSI was 91.2% and 94.2% for qSOFA (Fig.1, Table 3).We also found that qSOFA score and FGSI score were significantly correlated(p<0.0001)with strong positive correlation(r=0.704)(Table 3).
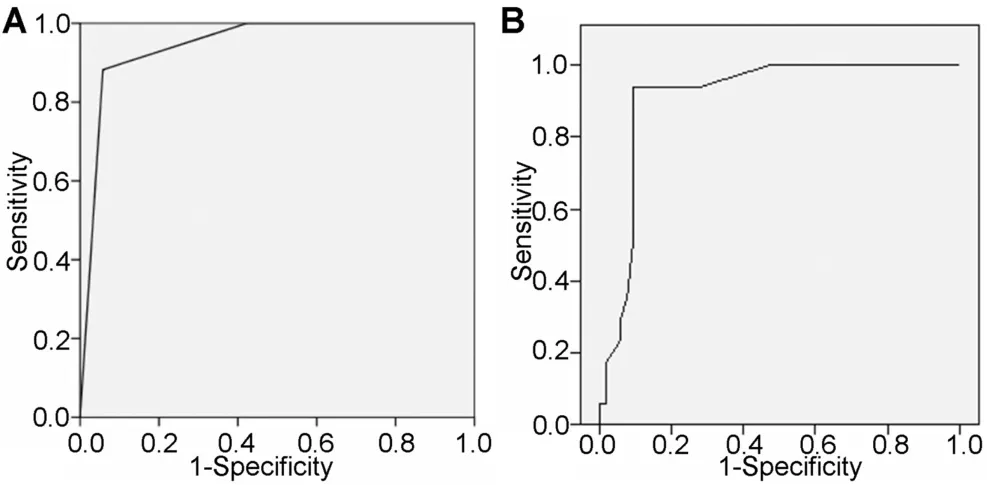
Figure 1 Area under receiver operating characteristic curve.(A) Quick Sepsis-related Organ Failure Assessment score; (B)Fournier’s Gangrene Severity Index score.
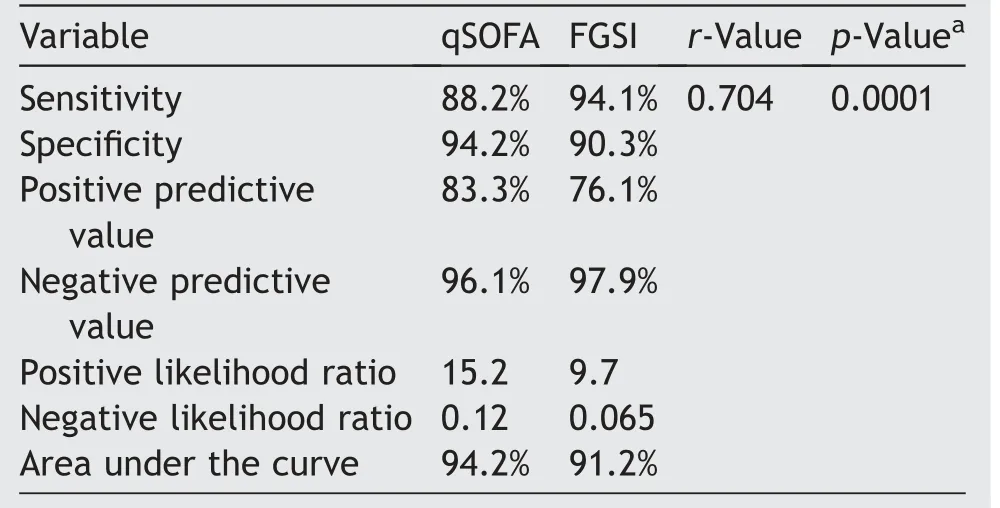
Table 3 Correlation of qSOFA and FGSI scores.
4.Discussion
FG is a form of fulminant necrotizing fasciitis of perineum and genitalia region that is potentially life-threatening.The course of infection spreads through the fascia of perineum and results in necrosis of the skin, subcutaneous tissue,fascia, and systemic infection [9].This condition is rare in developed countries, given the lack of data in previous studies.In previous series of FG, the largest series by Yilmazlar et al.[7] included 120 patients (80 males) in 16 years (seven patients per year) and Shukla et al.[11]included 57 patients in 4 years (14 patients per year).This study included 69 male patients over 5-years retrospective study (14 patients per year).This confirmed that the epidemiology of FG was varied in every country,and FG was more commonly found in developing countries than developed countries.This might be affected by poor hygiene factor, socio-economic status, and education level of developing countries (Table 4).We excluded isolated scrotal and/or penile abscess patient due to lack of perineal fascia involvement.This may contribute to survival of the patients and the high sensitivity of FGSI and qSOFA scores,since scrotal abscess patients generally have better clinical presentation than patients with perineal fascia involvement.This also explains the better mortality rate in previous studies by Hejase et al.[14] where 87% of their patients have no perineal and/or inguinal involvement and by Tahmaz et al.[15] where 42% of their patients have no perineal and/or inguinal involvement.

Table 4 Previous series of Fournier gangrene.
The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) task force recommended to assess sepsis-related organ dysfunction using SOFA.Due to the limitation of various regions in doing these tests, a simplified criterion, qSOFA, was used to assess organ dysfunction as soon as possible.Several studies had investigated the relationship of qSOFA and urosepsis due to another disorder such as acute pyelonephritis caused by upper urinary calculi.A study conducted in India compared the accuracy of this criteria and systemic inflammatory response syndrome (SIRS).In the study, qSOFA score of ≥2 was found in 14.2%participants,while SIRS score of ≥2 was found in 92.6%participants with mortality rate of 7.4%.The study then concluded that a higher score of qSOFA is associated with higher mortality rate (p<0.001) [16].Another study conducted in 141 Japanese diagnosed with acute pyelonephritis caused by upper urinary calculi also reported a higher predictive accuracy of in-hospital mortality and intensive care unit (ICU) admission compared to SIRS [17].
In our study,we analyzed the initial clinical presentation(vital signs), patient’s comorbidities, and initial laboratory results, and calculated the FGSI and qSOFA scores in survivor group (Group 1) and non-survivor group (Group 2).In initial vital signs, we found that the mean systolic blood pressure was significantly lower in Group 2.Low systolic blood pressure might be affected by various factors, but in sepsis condition, low blood pressure indicates a late phase of sepsis, due to severe inflammation and decreasing peripheral resistance.In a previous study by Roghmann et al.[18], they found that the non-survived FG patients had significantly lower mean arterial pressure than survived patients.Martinschek et al.[19] also found that nonsurvived FG patients had significantly lower mean systolic blood pressure (120.8 mmHgvs.92.8 mmHg,p=0.001),while Seymour et al.[8] stated that the mortality of sepsis patients with systolic blood pressure less than 100 mmHg increased 2.61 folds.
We also found that in our study,mean respiratory rate in Group 2 was significantly higher compared to Group 1(21.27 [SD: 2.88] breaths per minutevs.26.94 [SD: 5.34]breaths per minute,p=0.001).High respiratory rate indicates increased oxygen consumption due to hypoxemia in sepsis condition.High respiratory rate also indicates acidosis metabolic due to increasing anaerobic metabolism in severe sepsis condition.Seymour et al.[8] stated that increasing respiratory rate over 22 breaths per minute in sepsis patients increased the mortality up to 3.18 times.Previous studies by Erol et al.[20],Corcoran et al.[21],and Altarac et al.[22] also showed significantly increased respiratory rate of non-survived FG patients compared to survived patients, although the respiratory rates of those studies varied (Erol et al.[20]: mean 32.00 [SD: 4.99]breaths per minute; Corcoran et al.[21]: mean 25.4 [SD:5.9]breaths per minute;Altarac et al.[22]:median 22[95%confidence interval: 20—28] breaths per minute).
The median GCS score was also significantly different in this study(15[IQR:13—15]vs.13[IQR:10—15],p=0.0001).Even though GCS was primarily made for trauma patient assessment, several studies also used GCS for non-trauma patient assessment as in sepsis patients.In sepsis, complex process of inflammation may cause systemic disorder such as microglial hyperactivity, brain perfusion disturbance, blood—brain barrier dysfunction, and brain hypoxia[23].Seymour et al.[8]stated that decrease of GCS score of≤13 related with 4.31 times risk of mortality,while Vincent et al.[24] showed that mortality rates of sepsis patients with GCS scores 15, 13—14, 10—12, 6—9,and <6 were 26%,36%, 44%, 58%, and 70%, respectively.Dolan et al.[25]stated that even slight decrease of GCS score of <15 increased the risk of mortality by 1.37 times.
We found there was no single comorbidity that significantly increased the mortality risk in FG patients.Although heart failure and chronic kidney disease were more common in non-survivor group (17.6% and 29.4%), it was not statistically significant.Higher mortality rate was seen in patients with diabetes, heart disease, renal failure, and kidney disease.The difference of the results between this study and previous systematic review might be due to small-sized data to reach statistical significance.
In laboratory result, we found only thrombocyte and albumin levels that were significantly different between Group 1 and Group 2.Thrombocytopenia(platelet count <150 000/μL) is common in critically ill patients, with an estimated incidence of 20%—40%at some point during the ICU stay[26].The development of thrombocytopenia in patients with sepsis is secondary to various mechanisms.Platelets are activated in sepsis and bound to the endothelium,resulting in sequestration and destruction.Immune mediated mechanisms like nonspecific platelet-associated antibodies and cytokinedriven hemophagocytosis of platelets can also contribute to sepsis-induced thrombocytopenia.Severe sepsis is commonly associated with a net procoagulant state, and secondary consumptive conditions of thrombocytopenia, like disseminated intravascular coagulation,represent an extreme in the continuum of hemostatic abnormalities in patients with sepsis.Non-resolution of thrombocytopenia during the recovery from critical illness is a strong predictor of mortality.Patients with persistent thrombocytopenia had higher ICU,hospital, and 28-day mortality compared to those patients whose platelet counts have normalized[27].
Hypoalbuminemia is frequently detected in patients with sepsis.The cause for this condition was thought to be a combination of reduced hepatic synthesis, increased leakage into the interstitial compartment,and accelerated catabolism.Production of monocytic products such as IL-1,IL-6, and TNFα was thought to decrease synthesis of albumin.In a condition of sepsis, vascular permeability increased which made the process of transcapillary loss of albumin becoming much faster: the impairment in endothelium integrity caused an increased capillary loss, even 13 times higher compared to normal values [28].
In this study, we compared the prognostic value of both qSOFA and FGSI, and found that FGSI has better sensitivity but worse specificity compared to qSOFA (sensitivity of 94.1%vs.88.2% and specificity of 90.3%vs.94.2%) towards mortality to FG.The qSOFA score also has better PPV than FGSI score (83.3%vs.76.1%), but better NPV was found in FGSI score compared to qSOFA score(97.9%vs.96.1%).With better AUC (94.2%vs.91.2%), qSOFA score has better prognostic value for mortality due to FG.We also found strong positive correlation between qSOFA and FGSI to predict mortality in FG (r=0.704).This finding can be explained if we take a look at Table 3.In most of laboratory findings that were part of FGSI score, significant difference only found in thrombocyte count, since albumin was not part of FGSI score.With 2 points of qSOFA score were also part of FGSI score that significantly different between two groups, it would be reasonable that qSOFA score and FGSI score will be strongly correlated.In a meta-analysis conducted by Jiang et al.[29], the qSOFA score more than 2 was associated with a higher risk of mortality in emergency department patients with infection.The relative ratio of 4.55 suggesting qSOFA more than 2 predicts a moderate prognosis for emergency department patient with infection.The high specificity and good positive LR of qSOFA are good for screening infected patient which can be used to urge clinicians to investigate the presence of organ dysfunction in sepsis patient.On the other hand, poor sensitivity of qSOFA criteria means that even some patient who are actually at higher risk of death may be incorrectly classified and managed as non-severe infection that several additional biomarkers such as lactate could be a good solution[29].Another meta-analysis performed by Liu et al.[30]found that qSOFA was poorly sensitive but highly specific for prediction of mortality.In ICU patients, qSOFA was poorly sensitive(54%)and moderately specific(77%)for prediction of mortality in emergency department patient [30].
This finding confirms that qSOFA score could be used as predictor for mortality in FG patients, especially in rural area in Indonesia, where most laboratory examination could not be done.The qSOFA score is simpler and quicker to calculate than FGSI score, and even a general practitioner can calculate it at the time of patient arrival without having to wait for laboratory results.In case of low-risk patient (qSOFA score 0—1), primary hospital in rural area without ICU might be sufficient.In case of high-risk patient(qSOFA score 2—3), an admission to higher facility hospital with ICU and better facility might be required in order to prevent mortality.
5.Conclusion
The qSOFA score is a simple and quick scoring system with good prognostic value to predict Fournier gangrene patient with poor prognosis.The qSOFA score might be useful mainly in rural hospital where most laboratory examinations were not available.
Author contributions
Study concept and design: Bambang S.Noegroho, Kuncoro Adi, Akhmad Mustafa.
Data acquisition: Rais Syaeful Haq, Zola Wijayanti, Jason Liarto.
Data analysis: Rais Syaeful Haq, Zola Wijayanti, Jason Liarto.
Drafting of manuscript: Akhmad Mustafa, Zola Wijayanti,Jason Liarto.
Critical revision of the manuscript: Bambang S.Noegroho,Kuncoro Adi.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2023年2期
Asian Journal of Urology2023年2期
- Asian Journal of Urology的其它文章
- Radiofrequency ablation for renal tumours:A retrospective study from a tertiary centre
- Role of circulating tumor cell clusters in patients with metastatic hormone-sensitive prostate cancer receiving a gonadotropin-releasing hormone antagonist: A pilot study
- Percutaneous embolization by direct puncture for the treatment of high-flow priapism
- Subadventitial resection of the ureter—new method for surgical corrections of the ureteropelvic junction and ureterovesical junction obstructions
- Tunica albuginea versus buccal mucosa graft urethroplasty for anterior urethral stricture:A prospective randomised pilot study
- Antioxidant status in patients with bladder cancer regarding cancer stage and grade
