Tunica albuginea versus buccal mucosa graft urethroplasty for anterior urethral stricture:A prospective randomised pilot study
Mohammad Shazi Faridi , Vikas Sharma ,Adittya K.Sharma , Rahul Yadav
a Division of Urology, Department of Surgery, Hamdard Institute of Medical Sciences & Research and HAHC Hospital, New Delhi, India
b Department of Urology, Rajiv Gandhi Super Speciality Hospital, Tahirpur, Delhi, India
c Department of Urology, Apollomedics Super Speciality Hospital, Lucknow, Uttar Pradesh, India
KEYWORDS Buccal mucosa;Male urologic surgery;Tunica albuginea;Urethral stricture;Urethroplasty
Abstract Objective: The objective of the study was to compare the outcome of tunica albuginea urethroplasty (TAU) and buccal mucosa graft (BMG) urethroplasty for anterior urethral stricture.Methods: Thirty patients who met the inclusion criteria were randomised into two groups:TAU(Group A) and BMG urethroplasty (Group B).Surgical outcome was evaluated with pre- and post-operative work-up involving retrograde urethrogram, voiding cystourethrogram, uroflowmetry, and urethroscopy.Patients were followed up till 1 year.Results: Mean duration of surgery was statistically significant between two groups(p=0.0005).Maximum urine flow rate was comparable when compared between two groups (p=0.22) but statistically significant when compared pre-and post-operatively (p<0.001).At follow-up of 1 year,the successful outcomes were 80%in Group A and 87%in Group B.A total of five patients who had unsuccessful results required redo urethroplasty.Complications were minimal in both the groups.Conclusion: TAU provides outcomes equivalent to those of BMG urethroplasty.TAU has less operative time, easy to perform, and beneficial in patients with poor oral hygiene.
1.Introduction
Urethral stricture is defined as the scarring involving the urethral epithelium or spongy erectile tissue of corpus spongiosum[1].Urethral stricture is a complex problem and various modalities of treatment have been advocated over the years, and even today there is not much consensus on the best mode of treatment.Study showed that in 4196 men of urethral diseases, most common surgery performed was urethroplasty (bulbar, penobulbar, or penile) in 55.2% patients [2].The gold standard treatment of short segment bulbar urethral stricture is end-to-end anastomosis[3,4]and in some conditions augmented anastomotic urethroplasty[5].However,for anterior urethral stricture more than 2 cm the treatment of choice is buccal mucosa graft (BMG) urethroplasty[6—9].BMG is superior to full thickness graft as it is hairless and easier to harvest with better regenerative capacity of the donor site, concealed donor site scar [10]but it is also associated with fewer donor site complications[11—14].
There are few conditions which make the patient not ideal for BMG harvesting including patients with restricted mouth opening due to previous mouth or tongue surgery,submucous fibrosis (tobacco chewer), or active oral infections (candida, lichen, varicella-virus, or herpes-virus)[15,16].Moreover, the donor site complications like oral pain, numbness, and difficulty in mouth opening and speech, changed salivation demands for substitution[12,13].
To overcome the graft site morbidities and unsuitability of harvesting BMG,there is a requirement of an alternative with equivalent outcomes as BMG urethroplasty.The Monsieur’s tunica albuginea urethroplasty (TAU) is a technique where no graft material is required [17—19].
The aim of the study was to compare the TAU and BMG urethroplasty for anterior urethral stricture with respect to intraoperative, postoperative parameters, and urethroplasty outcomes.To our knowledge, there is no previous randomised study comparing the two techniques.
2.Patients and methods
2.1.Study design
It is a prospective,cohort,single-blind,pilot,single-centre study conducted from July 2018 to June 2019 after obtaining approval from institutional review board(RGSSH/REB/2018/29).Inclusion criteria were: male patients aged≥18 years with penile, penobulbar, and bulbar stricture,strictures >2.5 cm in length, and patients requiring repeated optical internal urethrotomy (OIU) or dilatations.Exclusion criteria were: multiple urethral strictures, previous failed urethroplasty, periurethral phlegmon, urethrocutaneous fistula, associated with chronic kidney disease or balanitis xerotica obliterans, scarred perineum,oral diseases, and those who refused to enrol in the study.The null hypothesis was that there was no difference in the endpoints between the two groups.The primary endpoint of the study was the success rate and the secondary outcomes were the complications and recurrence of both the procedures.The comparison was performed using the combined endpoint method.
In all,38 patients were enrolled in the study,of which 30 patients met inclusion criteria.Out of the eight patients who were excluded, five patients refused to participate in the study and three patients dropped out due to deviation from the study protocol.It was a single-blind randomised trial in which patients were only blind with the procedure performed.After providing written and informed consent,patients were randomised into two groups—TAU (Group A)and BMG urethroplasty (Group B) based on computer generated random number table (Fig.1).
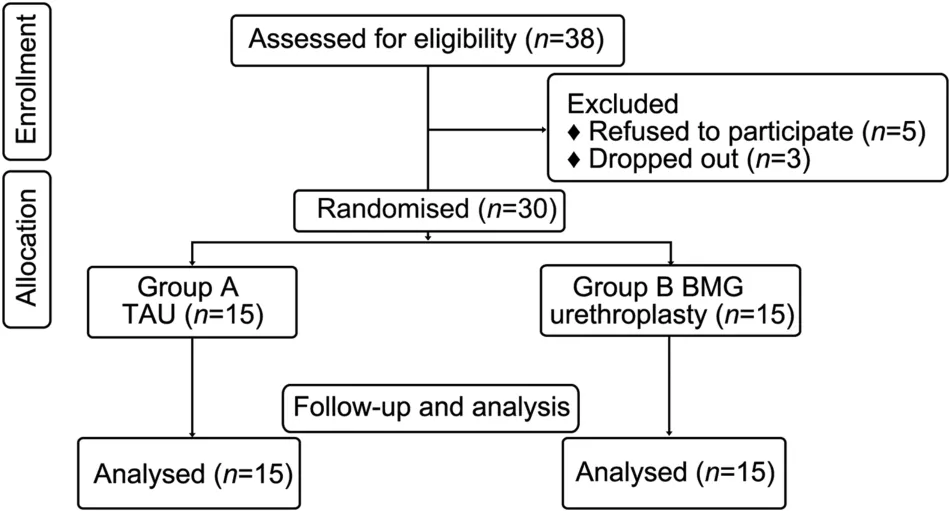
Figure 1 Flowchart of study design.TAU, tunica albuginea urethroplasty; BMG, buccal mucosal graft.
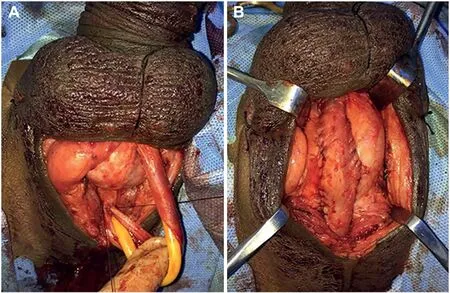
Figure 2 Intraoperative photograph.(A) Urethra incised dorsally after mobilisation; (B) Urethra stitched to tunica albuginea of corpora cavernosa.
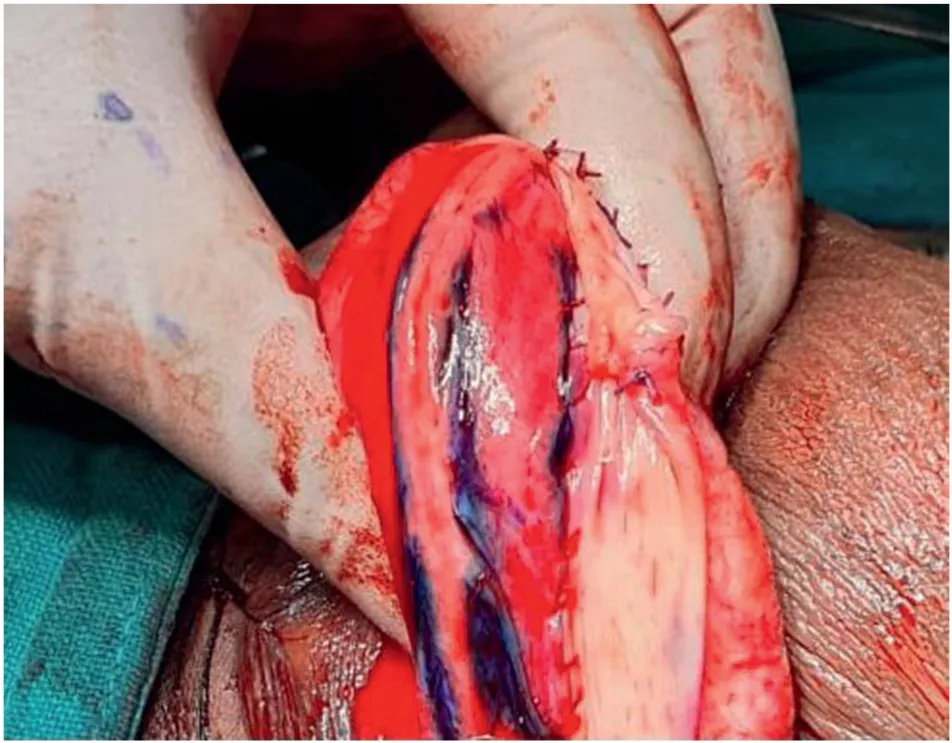
Figure 3 Intraoperative photograph of suturing of buccal mucosal graft margin to urethral margin.
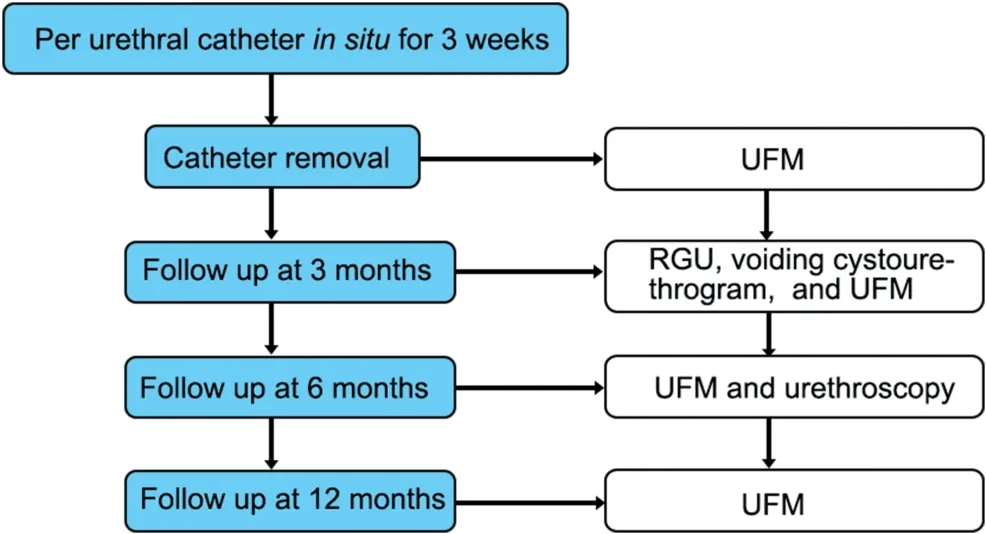
Figure 4 Follow-up protocol.UFM, uroflowmetry; RGU,retrograde urethrogram.
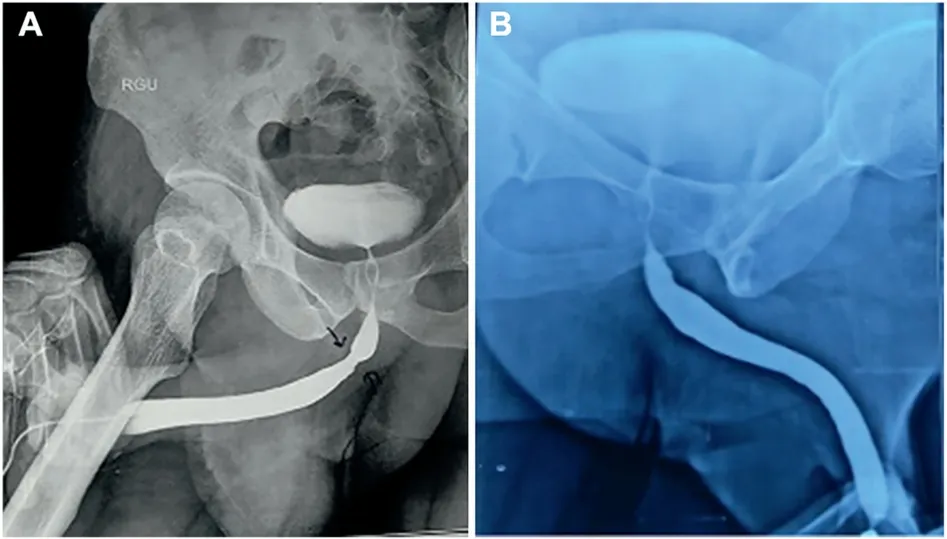
Figure 5 RGU of a patient.(A) Preoperative; (B) 3 months post tunica albuginea urethroplasty.RGU, retrograde urethrogram.The arrow means bulbar urethral stricture.
A detailed preoperative assessment along with history taking and physical examination was done on the first visit in the hospital.Further evaluations were performed with preoperative retrograde urethrogram (RGU), voiding cystourethrogram, uroflowmetry (UFM), and urethroscopy.All the details were recorded on the questionnaire designed for this study.
2.2.Surgical technique
The surgery performed includes standard TAU technique[18,20] under regional anaesthesia and dorsolateral onlay BMG urethroplasty technique [21,22] under general anaesthesia with nasal intubation as described below.In Group B,oral graft was harvested by another surgeon simultaneously.The width of the graft was 1.5—2.0 cm with appropriate length.The failure rate of both the techniques were 20% [17,23,24].
2.2.1.TAU procedure
The patient was placed in the simple lithotomy position,and a midline penoscrotal incision was made.The bulbar or penile urethra along with corpus spongiosum was completely mobilised from the tunica albuginea of the corpora cavernosa and the urethra was incised along its dorsal aspect [Fig.2A].The stricture was opened along its whole length.Hence, the lumen of the stricture segment faced the ventral aspect of the tunica albuginea of corpora cavernosa.A 16 Fr urethral catheter was then passed through the meatus into the bladder and retainedin situ.Then the edges of the slit urethra along with the tunica albuginea of the corpus spongiosum were stitched to the tunica albuginea of the corpora cavernosa using Vicryl 3-0 sutures [Fig.2B].Haemostasis was secured and fascia and skin were closed in layers.In this procedure, the ventral aspect of tunica albuginea of corpora cavernosa formed the roof of neourethra and the floor was formed by the stricture portion of the urethra along with corpus spongiosum.
2.2.2.BMG urethroplasty procedure
The patient was placed in a simple lithotomy position, and a midline perineal incision was made.The bulbar urethra was mobilised from the corpora cavernosa on one side,leaving the bulbospongiosus muscle and the central tendon of the perineum intact.On the left side, the urethra was partially rotated and the lateral urethral surface was underlined.The distal extent of the stricture was identified and the stricture was incised along its entire length on the dorsolateral aspect by extending the urethrotomy distally and proximally.After incision of entire stricture segment,the length and the width of the remaining urethral plate were measured.The oral mucosal graft was trimmed to an appropriate size according to the length and width of the urethrotomy, and then quilting of graft over the tunica albuginea of corpora cavernosa was done.The two apices of the graft were sutured to the proximal and distal apices of the urethrotomy by Vicryl 3-0 suture.The right margin of the oral graft was sutured to the left margin of the urethral mucosal plate[Fig.3].A 16 Fr foley catheter was inserted.After completion of graft suturing, the graft was completely covered by the urethra, and then by the muscles.Colles’ fascia, the perineal fat, and the skin were closed with interrupted absorbable sutures.
2.2.3.Follow-up protocol
After decatheterisation at 3 weeks,patients were followed up till 1 year.They were assessed based on UFM on each follow-up along with RGU and voiding cystourethrogram at 3 months of follow-up and urethroscopy at 6 months of follow-up period to evaluate the outcomes (Fig.4).
Success criteria were defined as when patient was voiding well without any need of urethral dilatation,maximum urine flow rate (Qmax) of >15mL/s without any obstructed flow pattern on UFM or without any narrowing on RGU or urethroscopy.If the patient required catheterisation in postoperative period, then the outcome was considered as failure.
2.2.4.Statistical analysis
The Statistical Package for the Social Sciences (SPSS®version 21; SPSS Inc.Chicago, IL, USA) was used for analysis.The mean and standard deviation(SD)were calculated for continuous variables.The χ2-test was used to compare categorical variables.The Welch two samplet-test was used to compare the difference between two continuous variables.The pre- and post-operative difference for Qmaxwas compared using paired samplet-test.The statistical difference between two groups for success and failure at different interval was calculated using Fisher’s exact test.One-sidedp-values were calculated for these analyses.Ap-value of <0.05 was considered to be statistically significant.
3.Results
Mean age, stricture length, post void residual urine, duration of stricture, width of urethral plate intraoperatively,mean Qmax(preoperative) and mean Qmax(postoperative)were statistically comparable between the groups(Table 1).When preoperative and postoperative Qmaxvalues were compared, the results were statistically significant (p<0.001).Mean duration of surgery were 121.73(SD:7.35)min and 132.20(SD:7.25)min for Group A and Group B, respectively and the difference was statistically significant(p=0.0005)(Table 1).Most of the strictures were present in bulbar urethra in 17 (56.7%) patients; 8(26.7%)patients had strictures in penobulbar urethra;and 5(16.7%)patients had in penile urethra.The aetiology of the stricture was idiopathic (46.7%), followed by inflammatory(23.3%) and traumatic (16.7%), and 13.3% had history of instrumentation.In Group A, two patients each had hypertension and diabetes mellitus whereas in Group B, hypertension was present in three patients and one patient had diabetes mellitus.Suprapubic cystostomy were inserted preoperatively in three patients and two patients in Group A and Group B, respectively, due to significant post void residual urine.
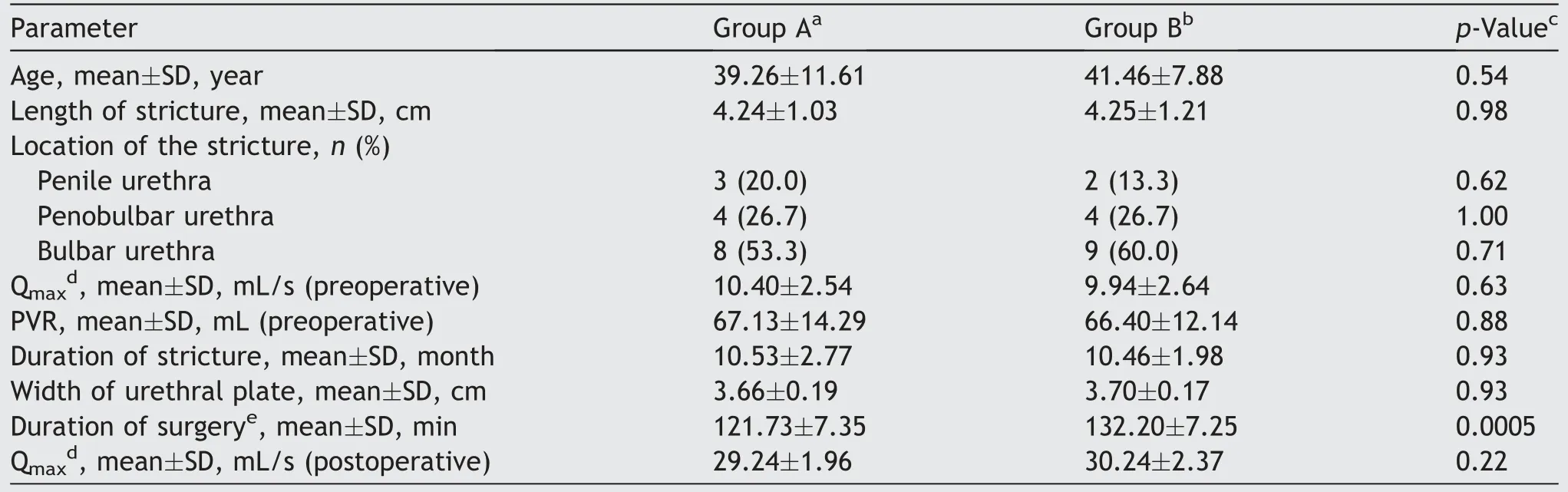
Table 1 Patient characteristics.
As per success criteria mentioned earlier, on 6 months of follow-up, 13 (87%) patients in Group A and 14 (93%)patients in Group B showed successful outcomes.However,the difference was statistically insignificant.Furthermore,the successful criteria were seen in 12 (80%) patients in Group A and 13 (87%) patients in Group B at 1 year of follow-up period, but the difference was still insignificant(p=1.00) (Table 2).After 1 year of follow-up, the success rates according to location of the urethral stricture were 66.7%(penile),75.0%(penobulbar),87.5%(bulbar)in Group A and 100% (penile), 75.0% (penobulbar), 87.5% (bulbar) in Group B.Fig.5 showed the RGU of a patient with successful outcome after TAU procedure.

Table 2 Outcomes of the two procedures.
Patients who showed no or poor improvement when compared with success criteria were considered as failure and required reoperation in the form of OIU or BMG urethroplasty after 1 year of follow-up.In Group A, one patient showed evidence of long dense re-stricture at penobulbar urethra and the other had bulbar urethral stricture on RGU; UFM was <6 mL/s; therefore, BMG urethroplasty was done.A single patient in Group A also developed short segment penile stricture evident both on RGU and urethroscopy with UFM of 11.2 mL/s, managed with OIU.Similarly,in Group B,one patient each developed dense re-stricture at penobulbar and the other had bulbar urethral stricture evident both on RGU and urethroscopy,and outcomes of UFM were 7.6 mL/s and 5.4 mL/s,respectively.Both of the patients were managed with redo BMG urethroplasty.
In Group A, one patient developed local site wound infection and in Group B, one patient had difficulty in opening the mouth(assessed by measuring the inter-incisal distance at maximum opening), and another patient developed erectile dysfunction (according to International Index of Erectile Function-5 criteria) as complications of the procedure.All these complications were managed conservatively.
4.Discussion
Management of anterior urethral stricture is still considered a challenge to urologist.BMG urethroplasty is one of the commonest surgeries performed for anterior urethral strictures of size more than 2 cm [6].However, harvesting buccal mucosa requires technical expertise and at times,it might also not be suitable to harvest buccal mucosa.Tunica albuginea is the layer present over both the corpora(cavernosa and spongiosa).The major difference between them is that the tunica of corpora cavernosa contains inner circular and outer longitudinal fibres whereas tunica of corpora spongiosa contains only circular fibres.However,the longitudinal layer of tunica of corpora cavernosa is absent between 5 o’clock to 7 o’clock position and this is the area where tunica of corpora cavernosa forms the urethral groove where the urethra rests [1].Therefore,histologically the tunica present at this groove has only circular fibres and hence, the histoanatomical properties of tunica corpora cavernosa and spongiosa are almost similar.The time tested tubularised incised plate urethroplasty is based on the same principle where the tunica exposed after incision of the urethral dorsal plate forms the roof of the neourethra [25].The outcome of tubularised incised plate urethroplasty has already been proven for hypospadias.Hence, we suggest that tunica albuginea in TAU urethroplasty also withstands the exposure of urine with time.
Urethroplasty of anterior urethral stricture by using locally available tunica albuginea is easy to perform without much technical expertise and is more feasible in patients of unhealthy buccal mucosa.TAU is also associated with limitations as it cannot be performed at meatal area due to absence of tunica albuginea.
In TAU, there are no graft site morbidities as no graft is harvested.In Group A, the mean duration of surgery was short (121.73 [SD: 7.35] min) when compared with Group B(132.2 [SD: 7.25] min) because there is no need of graft fixation to tunica of corpora cavernosa.In our study, the mean operative time of BMG urethroplasty was similar to the published data [26,27].However, this is the only study available till date which had calculated the operative time of TAU procedure.
In Group A, the success rate was 87% at 6 months follow-up period which dropped down to 80% at 1 year.The previous study also showed that the overall success rate of TAU was 80% at mean follow-up of 15.2 months[17].Literature on success rate of BMG urethroplasty was 80% at mean follow-up of 45 months [23,24], whereas in our study the success rate decreases from 93%at 6 months follow-up to 87% at 1-year duration.The difference may be due to short follow-up.However,when we compare the two studied groups in our study,the overall success rate of the two procedures declined with time,but the difference was not statistically significant.
In Group A, 3(20%) and in Group B, 2(13%) patients had failures and required surgery in the form of OIU or redo BMG urethroplasty after 1 year of follow-up.Studies also showed the same procedures for re-stricture patients [19,28].
In our study,1(7%)patient in Group A developed wound infection which was treated with appropriate antibiotic and regular dressing.In Group B, 2 (13%) patients had complications.One (7%) patient developed difficulty in mouth opening which resolved gradually in 6 weeks.Study revealed that trismus persisted in 5 (10%) patients till 1 month of follow-up [29].Moreover, the donor site morbidities were more common and persisted for longer duration in patients of chronic tobacco chewer[29].Another patient(6%) developed erectile dysfunction which also relieved over a period of 6 months [30,31].Studies showed that incidence of erectile dysfunction after BMG urethroplasty is around 10% [30,31].
Limitations of this pilot study were small sample size of 30 patients with mean follow-up of 1 year only.Therefore,this study also suggests the need for larger sample sizes in studies designed to have sufficient power to demonstrate that both the procedures are comparable.Moreover, histoanatomical properties of tunica albuginea and buccal mucosa are different.
5.Conclusion
TAU is easy to perform with a short learning curve and requires less technical expertise.The operative time is short and not associated with any graft morbidity.Technique has shown good and comparable success rates to BMG urethroplasty.Moreover, this technique can be used as an alternative in patients with unhealthy oral mucosa.
Author contributions
Study design: Mohammad Shazib Faridi.
Data acquisition: Mohammad Shazib Faridi, Vikas Sharma.
Data analysis: Mohammad Shazib Faridi.
Drafting of manuscript: Mohammad Shazib Faridi, Vikas Sharma.
Critical revision of the manuscript: Adittya K.Sharma,Rahul Yadav.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2023年2期
Asian Journal of Urology2023年2期
- Asian Journal of Urology的其它文章
- Role of circulating tumor cell clusters in patients with metastatic hormone-sensitive prostate cancer receiving a gonadotropin-releasing hormone antagonist: A pilot study
- Antioxidant status in patients with bladder cancer regarding cancer stage and grade
- Subadventitial resection of the ureter—new method for surgical corrections of the ureteropelvic junction and ureterovesical junction obstructions
- Percutaneous embolization by direct puncture for the treatment of high-flow priapism
- Analysis of the effect of holmium laser flexible ureteroscopic intrapelvic drainage in the treatment of parapelvic renal cysts
- The role of quick Sepsis-related Organ Failure Assessment score as simple scoring system to predict Fournier gangrene mortality and the correlation with Fournier’s Gangrene Severity Index: Analysis of 69 patients
