Analysis of the effect of holmium laser flexible ureteroscopic intrapelvic drainage in the treatment of parapelvic renal cysts
Yuanshen Mao , Wenfeng Li , Jun Da, Mingxi Xu, Yiwei Wang,Yufei Gu, Weixin Pan, Zhong Wang
Department of Urology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
KEYWORDS Flexible ureteroscopy;Holmium laser;Parapelvic renal cyst;B-ultrasound;Intrapelvic drainage
Abstract Objective: To explore the efficacy,safety,and feasibility of holmium laser flexible ureteroscopic intrapelvic drainage in the treatment of parapelvic renal cysts.Methods: From September 2012 to February 2019, a total of 18 patients, aged from 28 to 62(mean±standard deviation [SD]: 46.50±9.14) years, were diagnosed with parapelvic renal cysts and treated by holmium laser flexible ureteroscopic intrapelvic drainage.There were 10 males and eight females.All of the parapelvic renal cysts were unilateral, and two cases were complicated with pyelolithiasis.The diameters of the cysts ranged from 4.1 cm to 8.2 cm.Results: All the patients completed the operation successfully in one stage without conversion to open surgery; in two cases, it was difficult to find the cysts during the operation, and the localization was completed by B-ultrasound and percutaneous injection of methylene blue.The mean operative time was 33.89 (SD: 9.68; range: 22—54) min, and the mean hospitalization time was 2.67(SD:0.91;range:2—5)days.Three months and 6 months of follow-up were performed after surgery.The cysts disappeared in 13(72%)cases,and the diameter of the cysts in five (28%) cases decreased by more than 50%.Conclusion: Holmium laser flexible ureteroscopic intrapelvic drainage in the treatment of parapelvic renal cysts is simple, safe, and effective, and can be used as the first choice for the treatment of parapelvic renal cysts.
1.Introduction
A parapelvic cyst is a special type of renal cyst and includes perirenal cysts originating from the renal sinus and parapelvic cysts originating from outside the renal sinus and invading the renal sinus [1].The terms parapelvic and peripelvic cysts generally describe cysts around the renal pelvis or renal sinus.Most parapelvic cysts can be treated by laparoscopic renal cyst unroofing and decompression,but some parapelvic cysts are too endophytic to achieve complete unroofing, and it is easy to damage the structure of the renal hilum during the operation and even convert to open surgery.The latest 2019 edition of the Chinese guidelines for the diagnosis and treatment of urological diseases recommended that patients with large parapelvic cysts and local compression of the pelvis and calyces should be actively treated.This retrospective study aimed to confirm that holmium laser incision and internal drainage under flexible ureteroscopy have advantages of small trauma, rapid recovery, and a high success rate.In addition, the study also shared the techniques of finding the cyst wall during the operation.
2.Patients and methods
2.1.Patients
From September 2012 to February 2019, 18 patients with parapelvic cysts were treated with flexible ureteroscopic holmium laser incision and internal drainage.There were 10 males and eight females aged from 28 to 62(mean±standard deviation [SD] 46.50±9.14) years.All of them had unilateral parapelvic cysts, and two cases were complicated by renal pelvic stones, with sizes of 0.8 cm and 1.2 cm.The diameters of the cyst ranged from 4.1 cm to 8.2 cm (Table 1).Ten cases were found by physical examination; there were five cases with lumbar back discomfort and three cases with microscopic hematuria.Bultrasound and computed tomography (CT) examinations were performed before the operation.Imaging examinations showed that the cysts squeezed the renal pelvis and calyces.The Bosniak grade was Grade I.All patients had negative routine urinalysis and urine culture results.No preset double-J tubes were used before surgery in all patients.This study was approved by the Ethics Committee of Shanghai Ninth People’s Hospital(approval number:2016-47-C14/2).

Table 1 Patient characteristics.
2.2.Methods
All patients underwent general anesthesia (laryngeal mask anesthesia) in the lithotomy position.The 6/7.5 Fr Wolf rigid ureteroscope was performed to dilate and explore the ureter in order to confirm a normal ureter.The 10/12 Fr guiding sheath was placed along the guide wire, and the renal pelvis was ascended with a 7.5 Fr flexible ureteroscope (Storz Flex X2, Germany).Patients with renal calculi were treated with holmium laser lithotripsy.Combined with CT, the cyst wall was found to be light blue under the microscope.A few cyst walls were cut with a 200 μm holmium laser fiber (Raykeen Laser Technology Co., LTD, Shanghai,China).After the cyst wall was confirmed (it manifested as a light blue or translucent tissue slightly protruding into the renal pelvis, and this thin tissue had reduced vascular texture), the cyst wall in the blue area was removed by holmium laser, and the window diameter was approximately 1.5—2.0 cm so that the cyst was completely connected to the collecting system(Fig.1).The guide wire was inserted; the proximal end of the guide wire was located in the cyst; and a 6 Fr double-J tube was placed.The double-J tube was removed under cystoscopy 6 weeks after the operation.Patients underwent CT scan at 3 months and 6 months after surgery.
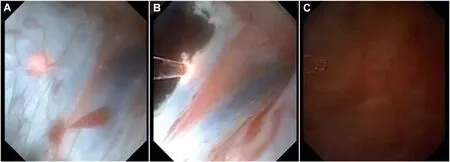
Figure 1 Video screenshots flexible ureteroscopic surgery with holmium laser for a simple parapelvic renal cysts.(A)Light blue or translucent thin tissue slightly convex to the pelvis with reduced vascular texture;(B)Cysts after fenestration;(C)Confirmation of the cystic cavity.

Figure 2 The puncture needle penetrated into the cyst and could be seen under flexible ureteroscope.The location of the puncture needle showed that the cyst wall was located at 6 o’clock.

Figure 3 Comparison of preoperative and postoperative CT.(A) Preoperative CT confirming a left parapelvic cyst; (B) CT scan showing that the position of double-J tube was normal and that the proximal portion was located in the cystic cavity; (C) CT scan showing that the cyst disappeared completely 6 months after the operation.CT, computed tomography.
During the operation, it was difficult to find the cyst in two cases.In one case, the affected side of the patient’s waist was raised.Under the positioning of B-ultrasound,percutaneous puncture of the lumbar costal cyst was performed.After the cystic fluid was confirmed, methylene blue was injected into the cystic cavity.The surgeon continued to look for the cyst wall with a flexible ureteroscope.The assistant used B-ultrasound combined with the cyst position and the swing of the flexible lens end of the ureter to assist in accurate positioning and finally found the capsule wall successfully.The other case was located at the lower pole of the kidney and was still difficult to locate with B-ultrasound alone.The puncture needle penetrated into the cyst and could be seen under flexible ureteroscope(Fig.2).It was proven that the cyst wall was located in the direction of 6 o’clock in the ureteroscopic field of vision,while the mucosa at 6 o’clock was opened with a laser.
The number of successful cases of one-stage operations,operative time(defined from the beginning of urethroscopy to successful placement of the double-J tube), postoperative symptom relief,length of stay,cyst changes(the cure standard is cystic cavity disappearance or cyst shrinkage more than 50%), and complications were evaluated [2].
3.Results
All 18 patients underwent successful operation in one stage, and there was no conversion to open surgery or difficult access for endoscopy.The mean operative time and SD was 33.89±9.68 min,ranging from 22 min to 54 min.There were no complications such as renal vascular injury,urinary extravasation, severe infection, or severe hematuria.The mean postoperative hospital stay was 2.67 (SD:0.91) days, ranging from 2 days to 5 days.
On the first day after the operation, CT scans showed that the position of the double-J tube was normal, and the proximal end was located in the cystic cavity.Patients underwent the CT scan at 3 months and 6 months after surgery.The cysts disappeared completely in 13 (72%)cases, and the diameter of the cysts in 5 (28%) cases decreased by more than 50% when compared with the diameter before the operation.The symptoms in five patients with lumbar back discomfort and three patients with hematuria disappeared after surgery,and postoperative CT review of two patients with calculus showed no residual or recurrence (Fig.3).
4.Discussion
Parapelvic cyst is an anatomic name that refers to a cystic lesion in the renal sinus.It includes urogenic cyst and nonurogenic cyst.The former is actually a simple cyst from the renal parenchyma growing into the renal sinus, while the latter mostly comes from the blood vessels or lymphatic vessels of the renal sinus.Clinically, they are generally referred to as pararenal cysts.The incidence rates range from 1%to 3%,and these cysts are benign.Most of them are Bosniak I type cysts.Type II cysts are rare and slow to progress [3].The latest 2019 edition of the Chinese guidelines for the diagnosis and treatment of urological diseases recommended that patients with large parapelvic cysts and local compression of the pelvis and calyces should be actively treated.In the past,it was generally believed that a cyst diameter of >5.0 cm with the abovementioned clinical symptoms necessitated surgery.However,due to its unique location, when a parapelvic cyst is relatively small,it can easily compress the collecting system or renal pedicle vessels.Therefore, some scholars suggest that the surgical indications of this disease should be relaxed appropriately:the cyst diameter of over 2.0 cm, obstruction of the compression collection system that may affect renal function, and complications of renal pelvis involvement, calyceal calculi, or secondary urinary tract infection, and surgery can be considered [4].
At present, the treatment of parapelvic cysts mainly includes incision and drainage, percutaneous renal puncture, and natural cavity drainage.Open drainage surgery includes open surgery [5], laparoscopic surgery [6], and robot-assisted laparoscopic parapelvic cyst unroofing decompression [7].The treatment of parapelvic cysts by percutaneous renal puncture includes percutaneous puncture and sclerotherapy under the guidance of B-ultrasound or CT [8] and percutaneous nephro-ureteroscopic laser unroofing of parapelvic cysts [9].The abovementioned surgical methods are traumatic, associated with a slow recovery, and can easily cause bleeding; therefore, they have been gradually replaced by natural lumen surgery in clinical application.As early as 2007,some foreign scholars reported that a case of parapelvic cyst with severe hydronephrosis was successfully cut and drained with a flexible ureteroscope [10].In 2010, Basiri et al.[11] reported two cases of parapelvic cysts treated with flexible ureteroscopic holmium laser incision and internal drainage.With the popularization and development of flexible ureteroscope technology, the reports on the treatment of renal cysts with a flexible ureteroscope have been increasing gradually.The indications for surgery have been further expanded by using a flexible ureteroscope [3].Compared with the traditional operation, flexible ureteroscopic holmium laser incision and internal drainage has the following advantages: (1) through the natural cavity of the human body, the operation is relatively simple, less damage, and short recovery time,and the curative effect is satisfactory.(2) Patients with bilateral parapelvic cysts or with upper urinary calculi can be treated at the same time without changing the body position during the operation.(3) For patients with extreme obesity, coagulation dysfunction, or general poor condition who are unable to tolerate laparoscopic surgery, flexible ureteroscopy has special advantages.(4)It can be repeated.However,the technology also has some shortcomings:(1)the cost is expensive.A flexible ureteroscope has a disadvantage of being damaged, and it is expensive to maintain.It has been reported that the mean number of uses of a flexible ureteroscope is 6—15 times,and it needs to be repaired every 3—13 h;therefore,it is difficult to implement in primary hospitals.(2) The success rate of flexible ureteroscopy is affected by the anatomical factors of the ureter.Approximately 10% of the patients cannot achieve the first stage successfully.The second stage of the operation increases the waiting time and treatment cost to patients.(3)Improper operation of a ureteroscope can easily bring out complications such as perforation of the ureteral mucosa, formation of a false passage, and mucosal avulsion injury, which may cause ureteral stricture in the long term.(4) Postoperative infection may occur.During the operation, bacteria may enter the blood and endotoxin may be absorbed due to poor perfusion fluid reflux and increased renal pelvis pressure.The incidence of infection after ureteroscopy is about 1.3%,and if the infection is not controlled in time, resulting in urinary sepsis or even septic shock, the mortality rate can be as high as 20%—40% [12].
The key of the operation is to identify the cyst position and determine the incision site;this is also the difficulty of the operation [13].Among the 18 cases treated in our department, the position of the light blue cyst in renal pelvic mucosa could be clearly located during the operation in 16 cases; it was mainly manifested as a light blue or translucent tissue slightly protruding into the renal pelvis,and this thin tissue had reduced vascular texture.However,there were two cases of renal pelvis mucosa without the obvious abovementioned manifestations.Therefore, it was necessary to locate the cyst with the help of B-ultrasound.Under B-ultrasound guidance,the outline of the soft mirror and holmium laser fiber could be roughly seen.Color Doppler ultrasound can be adjusted to blood flow imaging during high-pressure water injection, which is more convenient to locate the soft lens and understand the relationships among the incision site and cyst, pelvis,and calyces.In these two patients, it was still not possible to accurately determine the location of the cysts through B-ultrasound positioning.The affected side of the patient’s waist was raised.Under B-ultrasound positioning,percutaneous puncture of the lumbar costal cyst was performed.After the cystic fluid was confirmed, methylene blue was injected into the cystic cavity.The surgeon continued to look for the cyst wall with the flexible ureteroscope.The assistant used B-ultrasound combined with the position of cyst and the swing of the flexible lens end of the ureter again to assist in accurate positioning and finally found the capsule wall successfully.
A summary of our experiences is as follows: (1) Preoperative CT examination is essential for each patient because this modality can distinguish hydronephrosis and parapelvic cysts, assist in intraoperative localization, and determine the scope of the incision.Because pathological specimens cannot be obtained during the operation, preoperative CT can also perform Bosniak grading of cysts to exclude the possibility of cystic renal carcinoma.(2) The cyst wall should be cut from the weakest point as the center, and the window should be opened as wide as possible without damaging the blood vessels.For cysts that are close to the renal hilum, the direction of the incision should avoid damaging the renal pedicle blood vessels.(3)The double-J tube should be located in the cyst to effectively drain the cyst fluid and reduce the probability of contracture closure at the cyst wall incision.
5.Conclusion
Flexible ureteroscopic holmium laser internal incision for the treatment of parapelvic cysts, supplemented with B-ultrasound positioning if necessary,is a safe and effective treatment method,and has the advantages of being mostly noninvasive and having a rapid recovery and short hospital stay.This approach is worthy of clinical promotion and may become the preferred treatment for parapelvic cysts in the future.
Author contributions
Study design: Yuanshen Mao, Wenfeng Li.Data acquisition: Jun Da.
Data analysis: Mingxi Xu, Yiwei Wang.
Drafting of manuscript: Yufei Gu.Critical revision of the manuscript: Weixin Pan, Zhong Wang.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2023年2期
Asian Journal of Urology2023年2期
- Asian Journal of Urology的其它文章
- Radiofrequency ablation for renal tumours:A retrospective study from a tertiary centre
- The role of quick Sepsis-related Organ Failure Assessment score as simple scoring system to predict Fournier gangrene mortality and the correlation with Fournier’s Gangrene Severity Index: Analysis of 69 patients
- Role of circulating tumor cell clusters in patients with metastatic hormone-sensitive prostate cancer receiving a gonadotropin-releasing hormone antagonist: A pilot study
- Percutaneous embolization by direct puncture for the treatment of high-flow priapism
- Subadventitial resection of the ureter—new method for surgical corrections of the ureteropelvic junction and ureterovesical junction obstructions
- Tunica albuginea versus buccal mucosa graft urethroplasty for anterior urethral stricture:A prospective randomised pilot study
